Breathing And Exchange Of Gases Introduction
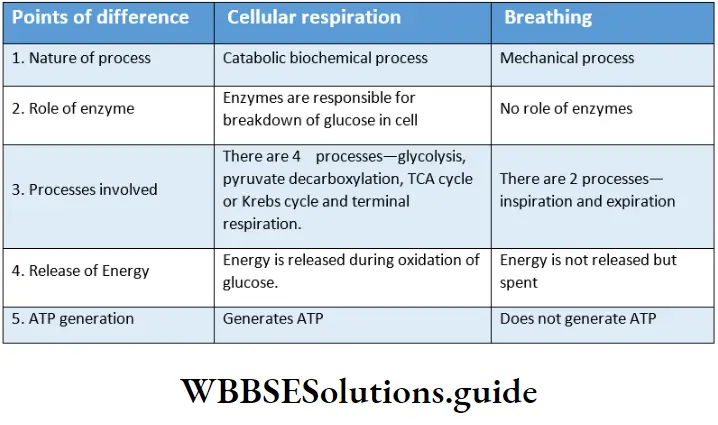
Cellular respiration:
If you hold your breath, even for a few seconds, you will gasp for air. Thus, breathing is an indispensable process in our body.
Through breathing, we take in oxygen. It reaches the cells and oxidises organic food substances to release energy.
This is called respiration also known as cellular respiration. The organ system concerned with breathing and respiration is called the respiratory system.
Breathing and exchange of gases notes for NEET PDF
Breathing Definition: The process by which air from the environment enters the body and after an exchange of gases in the tissues, goes out of the body is known as breathing.
Breathing is also known as ventilation.
Breathing Stages: There are two stages of breathing—
- Inspiration— intake of air from the environment into the body;
- Expiration— release of air from the body to the environment.
Breathing Importance: Breathing helps in the intake of oxygen from the environment into the body (specifically into the lungs of terrestrial animals including humans), through inspiration.
Within the lungs, the gaseous exchange takes place and carbon dioxide is released from the body into the environment through expiration.
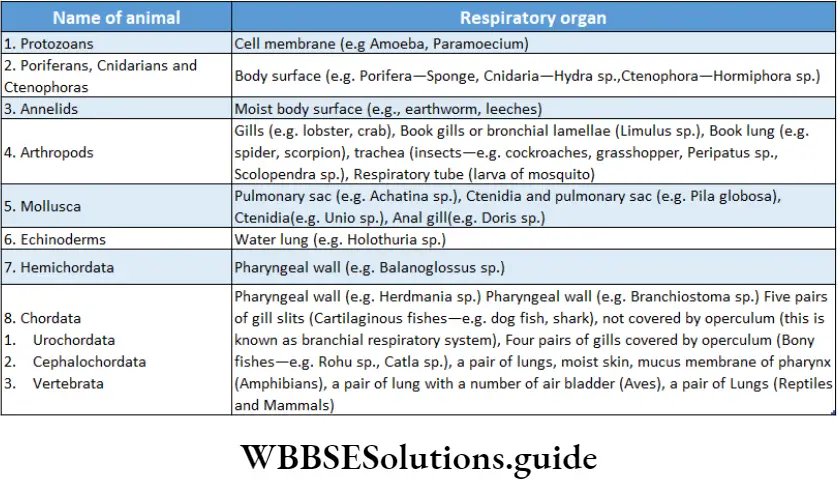
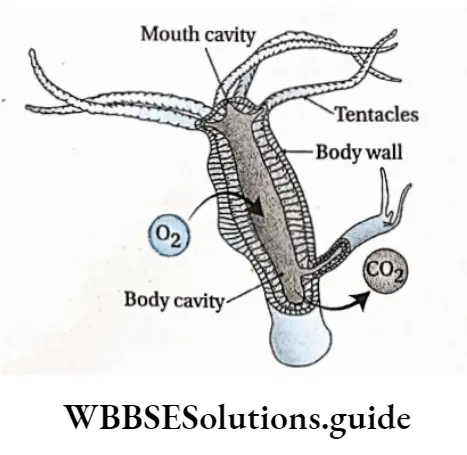
Respiratory Organs In Animals
Respiratory organs have evolved in animals according to their physical requirement and adaptation to the environment. According to their requirement, these organs are of various types.
The following table shows various types of respiratory organs in different organisms.


Respiratory Organs In Human Beings
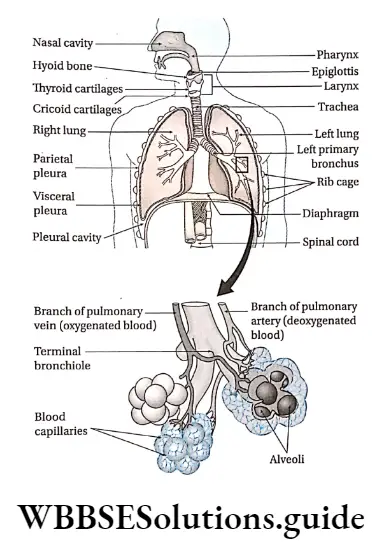
Respiratory system
The organ system of the human body through which the exchange of gases occurs between the body and the environment is called the respiratory system.
Components of the respiratory system: The organs and structures of the human respiratory system are—
- Nostrils and nasal passage,
- Pharynx
- Larynx,
- Trachea,
- Bronchi and bronchioles
- Lungs
Nostril And Nasal Passage
Nostril And Nasal Passage Definition: The openings by which the nose opens outward are known as nostrils or external nares and two cavities that extend from the external nares to the pharynx at the posterior end is called nasal passage or nasal cavity
Nostril And Nasal Passage Structural Features:
- Nostrils or external nares are present as two small openings at the base of the nose.
- The two openings through which nasal passages are connected to the pharynx are called internal nares.
- Each nostril leads into a nasal passage. The two nasal passages are separated from each other by a cartilaginous partition called nasal septum.
- Each nasal passage or cavity is divided into three parts— the lower vestibular region, middle respiratory region and upper olfactory region.
- The dilated chamber inside the nasal cavity is the vestibule. The inner surface of the vestibular region is made up of stratified squamous epithelium.
- This surface contains sebaceous glands and nose hairs (vibrissae) which serve to filter out inhaled particulates.
- The next region is the middle region called the respiratory region. The walls of the respiratory region are lined with respiratory mucosa. This respiratory mucosa is made up of pseudostratified ciliated columnar epithelium containing mucous cells.
- The mucous cells produce mucus, while the serous cells produce a watery fluid containing an anti-bacterial enzyme.
- The respiratory region is highly vascular and hence appears reddish. This region helps to condition the inhaled air.
- The upper region of the nasal chamber is called an olfactory region. The wall of this region is lined by olfactory epithelium.
- The olfactory region appears yellowish-brown in colour. It helps to detect the odour of the inspired air.
Nostril And Nasal Passage Functions:
- The nostrils and nasal passages provide a pathway for the air to enter the body.
- The nose and nasal cavity filter and clean any foreign particles present in the inhaled air.
- These particles get stuck into the mucus, which prevents them from entering the lungs.
| Class 11 Biology | Class 11 Chemistry |
| Class 11 Chemistry | Class 11 Physics |
| Class 11 Biology MCQs | Class 11 Physics MCQs |
| Class 11 Biology | Class 11 Physics Notes |
Pharynx
Pharynx Definition: The tube-like structure that connects posterior nasal and oral cavities to the larynx and oesophagus is known as the pharynx.
It extends from the base of the skull to the level of the sixth cervical vertebrae.
Pharynx Structural features:
- The pharynx is the common part of both the digestive and respiratory systems. Its length is approximately 12-14 cm.
- Structurally, the pharynx can be divided into three parts according to its location. These three parts are nasopharynx, oropharynx, and laryngopharynx.
- The nasopharynx is located between the internal nares and the soft palate and lies superior to the oral cavity.
- The oropharynx is a space present between the soft palate and the root of the tongue that extends inferiorly as far as the hyoid bone. The palatine and lingual tonsils are present in this region.
- The laryngopharynx is the part of the throat that connects to the oesophagus. It is located between the mouth and sixth cervical vertebrae. The superior boundary of this structure is at the level of the hyoid bone.
- The ventral face of the pharynx possesses an opening known as the glottis. Through this opening pharynx is connected with the larynx.
- The anterior part of the glottis has a cartilaginous outgrowth, known as epiglottis. When food is swallowed, epiglottis prevents food from entering the larynx by covering the glottis as a lid.
- The upper part of the pharynx contains a small muscular structure known as the uvula.
Pharynx Functions:
- The pharynx serves as a pathway for both the digestive system and respiratory system since both food and air passes through it.
- The surface of the nasopharynx is covered with pseudostratified ciliated epithelium tissue. It filters the inhaled air.
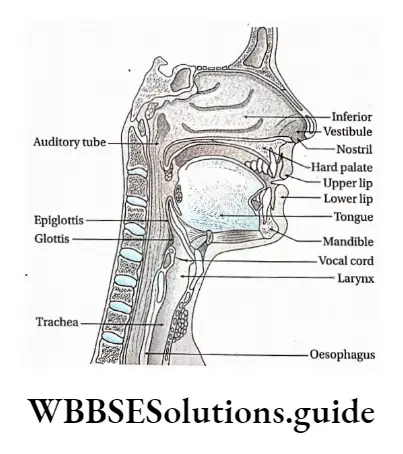
The Larynx
The Larynx Definition: The cartilaginous structure located between the pharynx and the trachea that helps to produce sound is called the larynx.
Larynx Structural features:
- The larynx is a cartilaginous triangular box whose apex, known as the Adam’s apple in males, is visible at the front of the neck. The larynx is also known as the voice box. The size of the larynx is larger in men at puberty than in females. For an adult male, it is 4.5 cm but for a female, it is 3.5 cm.
- The laryngeal skeleton is composed of nine cartilages—three unpaired (thyroid, cricoid, and epiglottis) and three paired (arytenoid, corniculate, and cuneiform) that are connected by membranes and ligaments.
- The thyroid cartilage is larger in size. It has two parts or laminae. A clear groove is visible between the two laminae, known as the thyroid notch.
- The upper part of the larynx bears a ‘U’ shaped bone known as hyoid bone. This bone remains connected with the larynx by a flat, extended membrane.
- Ligaments of the larynx are paired. The upper two pairs are known as ventricular folds (also known as false vocal cords) and the lower two pairs are known as vocal folds.
- The vocal folds are responsible for producing sound. These are known as vocal cords. During expiration, air comes out through the vocal cord creating vibrations which produce sound.
- Below vocal folds, the epithelium is of pseudostratified ciliated columnar type. Here, the action of the cilia directs mucus movement upward towards the pharynx. This helps in removing mucus from the lungs.
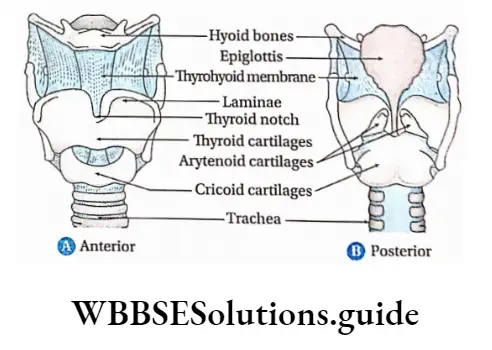
Larynx Functions:
- The ciliated mucous lining of the larynx has the ability to remove foreign particles and to warm and moisten the inhaled air.
- The other important function of the larynx is sound generation (phonation).
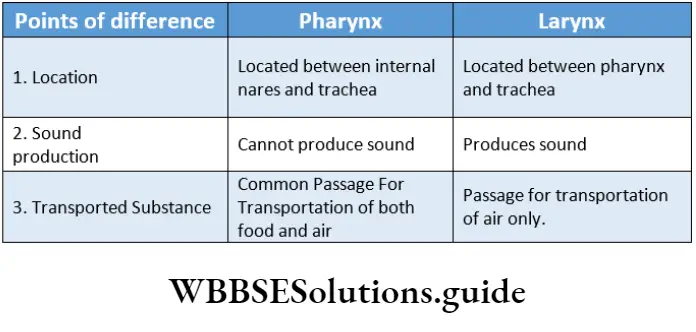
Trachea
Trachea Definition: The membranous tube-like structure, surrounded by rings of cartilage and extends from the posterior end of the larynx to the bronchial tubes and conveys air to and from the lungs, is known as the trachea or windpipe.
Trachea Structural Features:
- The trachea is a rigid tube, about 12 cm long and 2.5 cm in diameter.
- The trachea is encircled by 16-20, C-shaped cartilaginous rings, made up of hyaline cartilage.
- Posteriorly, it has a flat band of muscle and elastic connective tissue. This is called the posterior tracheal membrane. It closes the C-shaped rings.
- The cartilaginous rings hold and support the trachea preventing it from collapsing in the absence of air. However, it also provides some flexibility for any neck movement.
- The tracheal mucosa consists of pseudostratified ciliated columnar epithelium tissue. The mucous layer has goblet cells that secrete mucus. Its submucosa contains cartilage, smooth muscle and seromucous glands.
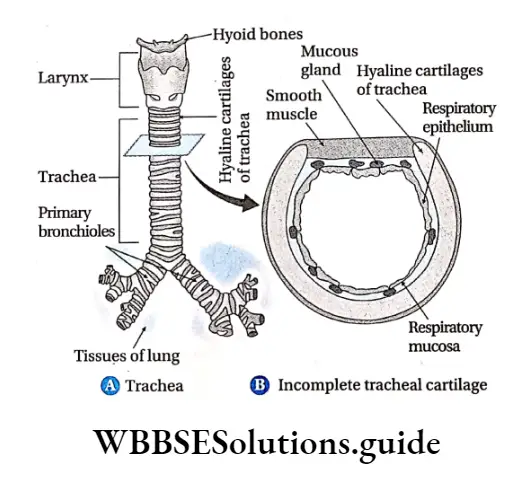
Trachea Functions: The ciliated epithelium of the trachea washes out the mucus-containing debris towards the pharynx. This prevents their accumulation in the lungs.
On coughing, the wall of the trachea contracts, narrowing its diameter. Therefore, coughing causes air to move out faster through the trachea, thus expelling mucus and foreign objects.
Class 11 biology breathing and exchange of gases notes with diagrams
Bronchi
Bronchi Definition: The two channels, formed by the branching of the trachea and leading to the lungs at the level of the 5th thoracic vertebra, are known as bronchi.
Bronchi Structural features:
- The two primary bronchi arise from bifurcation of the trachea. The right bronchus is wider (2.5 cm), shorter in length and more vertical than the left bronchus. Its length is approximately 5 cm.
- Each bronchus continues for 2 to 3 cm and enters the hilum (a slit in the lung) of each lung, respectively. Like the trachea, the primary bronchi are also surrounded by C-shaped hyaline cartilages.
- The main right bronchus (primary bronchus) is further subdivided into three secondary bronchi while the main left bronchus (primary bronchus) divides into two secondary bronchi.
- Each of the secondary bronchus again divides into branches forming tertiary bronchi and finally smaller terminal bronchi.
- The divisions of the respiratory passageways are known as the bronchial tree.
- The bronchial tree has a substantial amount of elastic connective tissue, which is important in expelling air from the lungs. The inner wall of the bronchus possesses ciliated epithelium.
Functions: Bronchi carry the air from the trachea, all the way to the alveolar air sacs.
Tracheobronchial tree
The structure consisting of the trachea, bronchi, and bronchioles that form the airways in the upper part of the lung is called a tracheobronchial tree. It is referred to as a tree because its branching pattern resembles that of a tree.
Bronchioles
Bronchioles Definition: The numerous branches into which a bronchus divides are known as bronchioles.
Structural features:
The bronchioles are of three types, each becoming progressively smaller in size. These are—
- Lobular
- Terminal bronchioles,
- Respiratory bronchioles.
- The terminal or transitional bronchioles divide into respiratory bronchioles. Apart from air conduction, they are also involved in gaseous exchange between blood and air.
- These respiratory bronchioles divide further into smaller branches to form alveolar ducts.
- The terminal end of these ducts forms a sac-like structure known as alveoli (singular: alveolus).
- Human lungs contain approximately 300-500 million alveoli.
- Bronchioles are lined with muscular walls.
Bronchi Functions:
- The bronchioles conduct air from the bronchi to the alveoli. They also regulate the amount of air that passes through the lungs during inspiration and expiration.
- The lobular and terminal bronchioles are known as dead space—as no gaseous exchange occurs in these places.
- The respiratory zone begins with the respiratory bronchioles, leading to the alveoli where the exchange of gases takes place.
- There are very small alveoli present at certain points on the wall of the respiratory bronchiole. These help to carry out gaseous exchange within the respiratory bronchioles.
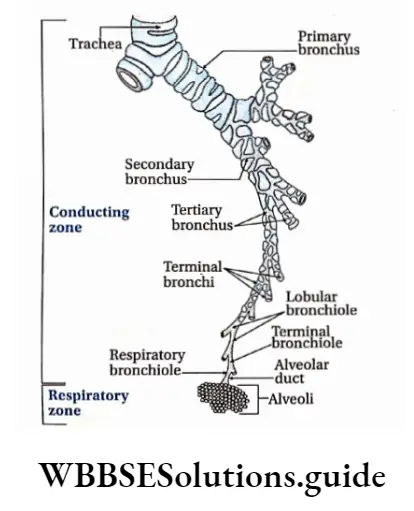
Bronchi Conducting and Respiratory zones
The airways beyond the larynx can be divided into two zones. The conducting zone extends from the top of the trachea to the beginning of the respiratory bronchioles.
It contains no alveoli and so, no gaseous exchange with blood occurs. The respiratory zone extends downwards starting from the respiratory bronchioles. It contains alveoli and is the region where gas exchange occurs with the blood.
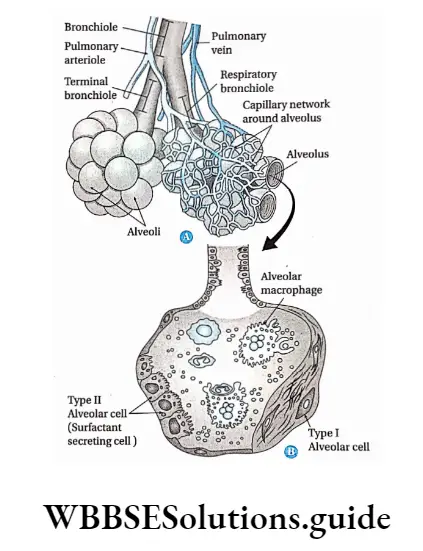
Lungs
Lungs Definition: The paired, cone-shaped spongy organs required for breathing, present on both sides of the human heart in the thoracic cavity are known as lungs.
Lungs Structural features:
- Lungs occupy a considerable portion of the thoracic cavity. A muscular partition called the diaphragm separates the thoracic cavity from the abdominal cavity.
- The lungs do not fill the entire rib cage. Most of the space within the rib cage, inferior to the lungs, is occupied by organs like the liver, stomach and spleen.
- The right lung is divided by an oblique fissure and a horizontal fissure into three lobes—superior, middle and inferior.
- The left lung is divided by an oblique fissure into two lobes—superior and inferior. Each lobe is subdivided into lobules, and each lobule contains a bronchiole serving many alveoli.
- The left lung is slightly smaller than the right lung. The anterior part of the left lung has an indentation called the cardiac notch to accommodate the heart.
- Lungs are enclosed within a thin, transparent, double-layered membrane called pleura. The space between the two layers of pleurae is called the pleural cavity.
- The pleural cavity is filled with a film of watery fluid, called the pleural fluid.
- The space between the pleural sacs of the two lungs is the central compartment of the thoracic cavity. This is called the mediastinum.
- Bronchus, blood vessels, lymphatic vessels, and nerves enter into the lungs through a slit in the mediastinal surface of the lungs, called the hilum.
- The outer pleural layer (attached to the chest wall) is called the parietal pleura, while the inner layer (attached to the surface of the lung) is called the visceral pleura.
Functions of pleurae and pleural fluid
Lungs Reduce friction: Pleural fluid acts as a lubricant that enables the lungs to expand and contract with minimal friction.
Creation of pressure gradient: Pressure in the pleural cavity is lower than atmospheric pressure. This creates a pressure gradient, which actually assists in the inflation of the lungs.
Compartmentalisation: Pleurae, mediastinum and pericardium compartmentalise the thoracic organiser This compartment formation prevents the spreading of infections to another organiser
The inner wall of the lungs is lined by numerous alveoli. It lacks any cartilage or smooth muscle. The wall of the alveoli and alveolar duct is lined by a single layer of squamous epithelial tissue.
The cells that remain lining the alveoli are called pneumocytes which include four types of cells, such as—
Type 1 alveolar cell: The walls of alveoli are mainly composed of these cells. These are flat and elongated cells with extremely thin cytoplasm and flattened nuclei. They are mainly involved in gaseous exchange. It occupies around 95% of the surface area of the alveolus,
Type 2 alveolar cells: It occupies around 2% of the surface area. These cells are small, cuboidal cells that are usually found scattered in the squamous epithelium of the alveolus.
Type 2 cells secrete a detergent-like lipoprotein called pulmonary surfactant. This surfactant forms a thin film inside the alveoli and bronchioles. It is also responsible for regeneration of the normal alveolar structure subsequent to injury,
Type 3 alveolar cells: They are also known as brush cells, due to their characteristic appearance under the electron microscope. These cells remain scattered throughout the lungs, closely associated with nerves.
Type 3 cells may function as chemoreceptors.
Macrophage cells: These cells kill pathogens that enter the respiratory system.
Function Of Alveolar Or Pulmonary Surfactant
- Pulmonary surfactant is a lipoprotein complex produced by type II alveolar cells. The surfactant reduces the surface tension of the alveoli.
- As a result, alveoli do not collapse due to surface tension, even though, they are very small in size. The alveoli can, thus, always remain open, to make breathing easier.
- Moreover, due to the reduction in surface tension, fluid cannot enter the alveoli from the surrounding blood capillaries. In this way, surfactant prevents pulmonary oedema.
- The most studied surfactant protein is SP-A, which is mostly found in Clara cells (dome-shaped cells with short microvilli, found in bronchioles) and Type II alveolar cells.
Macrophage cells Functions:
- Lungs are the main components of the respiratory system, as they carry out the gaseous exchange (which takes place within the alveoli).
- Lungs may also release certain useful substances into the blood. Some of these substances play local regulatory roles within the lungs.
- Lungs also act as a “sieve” that traps and dissolves small blood clots generated in the systemic circulation. Thus, the lungs prevent them from reaching the systemic arterial blood.
Mechanism Of Breathing And Its Regulation In Humans
The mechanism of breathing involves oxygen-rich air entering the alveoli within the lungs and carbon dioxide from the alveoli being expelled out of the body.
Bones And Muscles Associated With Breathing
During breathing, the bones of the rib cage that play major roles, are—
- Sternum, present at the front of the rib cage,
- 12 thoracic vertebrae and
- 12 pairs of ribs.
The muscles that are necessary to carry out breathing are called respiratory muscles. The main respiratory muscles are—
- Diaphragm And
- Intercostal Muscles
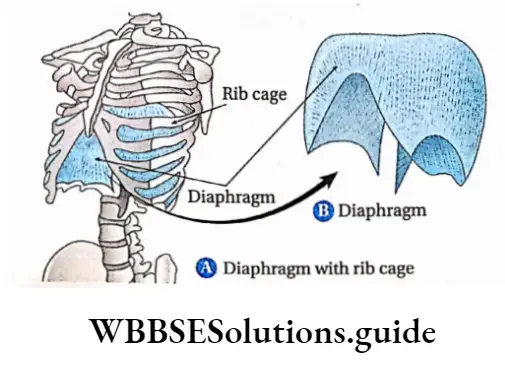
Diaphragm
- Thin, dome-shaped muscle, attached to the lower ribs and vertebral column is the diaphragm. When the diaphragm contracts, it moves downward which increases the vertical dimensions of the chest cavity and inspiration occurs.
- The diameter of the thorax also increases as the ribs are lifted outward.
- During expiration, the diaphragm relaxes and moves upward which decreases the volume of the chest cavity. Generally, in normal breathing, the diaphragm moves about 1 cm.
- It may move up to 10 cm during forced expiration. Paralysis of the diaphragm causes paradoxical movement.
- During this movement, the diaphragm moves up rather than down, with inspiration. This occurs when a person sniffs.
- The phrenic nerve is the nerve associated with the diaphragm, that controls its functioning.
Intercostal muscles
Muscles associated with the rib cage are called intercostal muscles. There are 11 pairs of internal intercostal muscles and 11 pairs of external intercostal muscles, located adjacently, at an angle of 90° to each other.
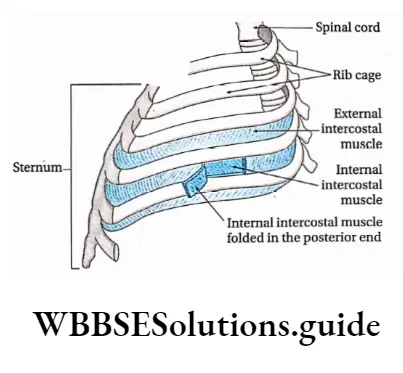
External Intercostal Muscles: Due to the action of these muscles, ribs move upward and forward at the time of contraction of the muscles during inhalation.
Cough and sneeze
These are a type of reflex action controlled by the nervous system. Generally, a sneeze occurs when the inner surface of nasal passages gets stimulated or irritated and a cough occurs when the inner surface of the trachea gets stimulated.
Hiccup
A hiccup is a sudden inspiration due to the contraction of the diaphragm. This phenomenon is observed when the phrenic nerve of the diaphragm becomes stimulated.
During this sudden inspiration, the air strikes the vocal cord, which produces the sound.
Internal Intercostal Muscles: The action of these muscles pulls the ribs downward and inward (antagonistic function to external intercostal muscles) during Exhalation.
Mechanism Of Breathing
There are two stages of breathing—inspiration and expiration. The mechanism of breathing is discussed on the basis of these two stages.
Inspiration
Inspiration Definition: The active phase of breathing in which O2 rich atmospheric air enters into alveoli is called inspiration.
Inspiration Mechanism:
The diaphragm is dome-shaped in its relaxed state. During deep inspiration, it contracts and i move downward.
Simultaneously, the external intercostal muscles contract and the rib cage moves upward and outward.
Due to the contraction of the diaphragm and the external intercostal muscles, the volume of the thoracic cavity increases.
The sternum moves upward and forward. This also causes a further increase in the volume of the thoracic cavity.
An increase in the thoracic cavity increases intrathoracic pressure by 3 mm Hg with respect to atmospheric pressure.
The lungs expand as the thoracic volume increases. As a result, a partial vacuum is generated in the alveoli, since the air pressure within the alveoli decreases.
Short notes on breathing and exchange of gases for quick revision
As the alveolar pressure is now less than atmospheric pressure (air pressure outside the lungs), air naturally flows into the Alveoli, Via the respiratory passages.
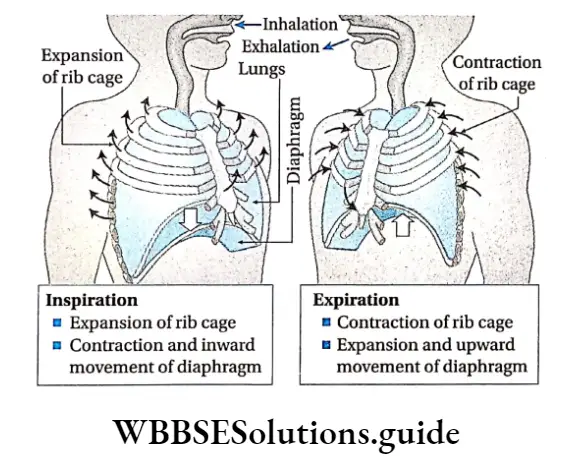
Expiration
Expiration Definition: The passive phase of breathing, in which CO2 rich air is expelled from alveoli to the atmosphere is called expiration.
Expiration Mechanism:
- During expiration, the thoracic wall and lungs recoil due to their elastic properties.
- The diaphragm and external intercostal muscles move upward and relax. As a result, the rib cage and sternum move down and inward.
- Contraction of internal intercostal muscles moves the rib cage and sternum more downward and inward.
- This causes a reduction in the thoracic cavity volume.
- The intrapulmonary pressure in the alveoli increases by 3 mm Hg with respect to the atmospheric pressure. Then, CO2 rich air flows through respiratory passages and is expelled out.
Path Of Expiration
CO2 rich air → alveoli → alveolar duct → bronchiole bronchi → trachea → larynx → open glottis → internal nares pharynx → nasal passage → external nares.
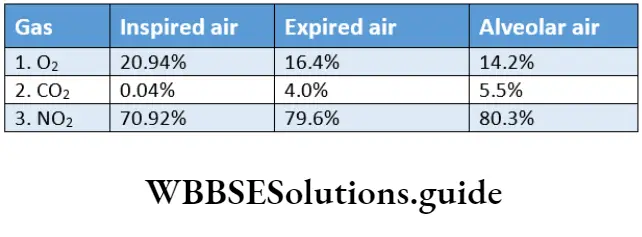
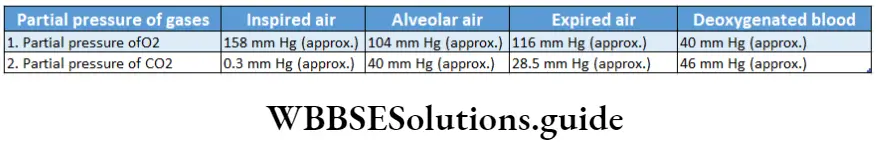
Inspired Air, Expried Air, Alveolar Air
Inspired air
Inspired air Definition: The volume of air taken in the respiratory system under resting conditions, during normal inspiration or forceful inspiration, is called inspired air.
Volume: A person can normally inspire 500 ml of air under resting conditions, but the volume increases to 3500 ml during forceful inspiration.
Expired air
Expired air Definition: The volume of air released by the respiratory system under resting conditions, during normal expiration or forceful expiration, is called expired air.
Volume: A person can normally expire 500 ml of air under resting conditions, but the volume increases to 1000 ml or 1500 ml during forceful expiration.
Alveolar air
Alveolar air Definition: The volume of air that enters the alveoli, located in both the lungs, during inspiration, is called alveolar air.
Volume: During normal inspiration, out of the 500 ml of inspired air, 150 ml remains as anatomical dead space air and the remaining 350 ml enters the alveoli.
Regulation Of Breathing
Unlike all other organ systems, the respiratory system demonstrates both involuntary as well as voluntary modulation. We breathe involuntarily, but we can willingly modify our breathing pattern.
We can hold our breath up to a certain point called “breaking point.” Beyond this point, we can no longer hold our breath.
Our breathing pattern is also modulated by the activities of speech and singing. Respiration is regulated by two mechanisms— The nervous or neural mechanism and the Chemical mechanism.
Nervous mechanism
The nervous mechanism involves respiratory centres and afferent and efferent nerves. The respiratory centres are stimulated by impulses received from various receptors.
Respiratory centres: The rhythmic pattern of breathing is carried out by four separate respiratory centres, located in the medulla oblongata and pons.
These centres in the medulla are divided into the Dorsal Respiratory Group (DRG) and the Ventral Respiratory Group (VRG). The respiratory centres in the pons are the pneumatic centre and the apneustic centre.
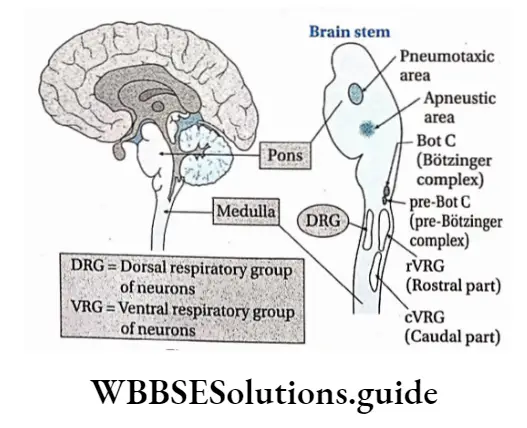
Dorsal respiratory groups (DRG): Dorsal group of respiratory neurons (DRG), also known as the inspiratory centre, is located in the dorsal part of the medulla oblongata. Apart from their voluntary control over respiration DRG centre, is located in the dorsal part of the medulla oblongata.
Apart from their voluntary control over respiration DRG also has a role in controlling speaking, crying, laughing, singing and other physical activities. However, the impulses originating from the DRG neurons are primarily responsible for inspiration.
Inspiration is initiated by a rhythmical on-off pattern. During the “on” part of the cycle, neurons in the DRG cause the inspiratory muscles to contract. This, in turn, initiates inspiration.
During the I “off” part of respiratory cycles, the neurons from the DRG stop sending impulses.
The inspiratory muscles relax and passive expiration occurs.
Ventral respiratory groups (VRG): The VRG, also known as the expiratory centre, is located in the central part of the medulla. It consists of both inspiratory and expiratory neurons. Although it receives nerve impulses from DRG, it is mainly responsible for expiration.
Apneustic centre: It is located in the posterior part of the pons. It has a stimulatory effect on the inspiratory centre. Thus, it lengthens inspiration by preventing inspiratory neurons from being “switched off”. This is accomplished by providing a constant stimulus to continue inspiration.
Pneumotaxic centre: It is located in the anterior part of the pons. It is a collection of neurons called the pontine respiratory group. Its primary role is to decrease inspiration or “switch off” the inspiratory neurons and initiate expiration.
It inhibits the impulses from the apneustic centre, which helps to slow inspiration and control the rate of respiration. Chemical control mechanism Chemical control of breathing is carried out by chemoreceptors.
The chemoreceptors are sensory nerve endings that are stimulated by changes in the chemical composition of blood. These changes in the composition of blood may be due to changes in the partial pressure of oxygen and carbon dioxide.
There are two groups of chemoreceptors—central and peripheral chemoreceptors. The central chemoreceptor is in the central nervous system. The other group, the peripheral chemoreceptor, is located in the periphery of the body and is exposed to the arterial blood.
Central chemoreceptor: These are specialised cells, present on the ventral surface of the medulla oblongata. At rest, most respiratory responses are mediated by these central chemoreceptors.
These cells are sensitive to CO2-induced changes in hydrogen ion concentration in the brain interstitial fluid.
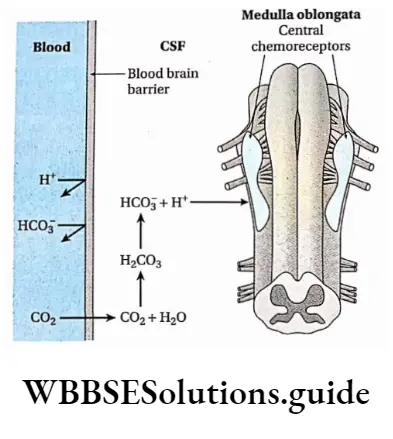
Hydrogen ion is not able to cross the blood-brain barrier but CO2 can. This CO2 enter into the CSF and reacts with a water molecule to form carbonic acid. Carbonic acid is broken down into H+ and HC03″.
So, increasing CO2 concentration in blood also increases H+ concentration in CSF. The CSF has a very small amount of buffers; the excess of hydrogen ions (or low pH) in the CSF stimulates the central chemoreceptor in the medulla.
As a result, respiratory rate and tidal volume increase to decrease acidity (i.e., increased pH). The remaining carbon dioxide is exhaled into the atmosphere.
The arterial partial pressure of CO2 ( Pco ) and hydrogen ion concentration of the CSF return to normal to maintain homeostasis of the gases.
In contrast, if the level of CO2 and hydrogen ion concentration is low, then the respiratory rate decreases. This allows the concentration of CO2 and H+ in the blood to increase.
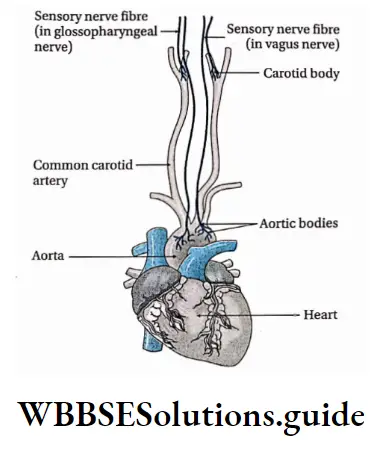
Peripheral chemoreceptors: These are located in the arch of the aorta (aortic bodies) and in the bifurcation of carotid arteries (carotid bodies) in the neck.
They sense changes in pcO2 and H+ concentration in the arterial blood. If pCO2 and H+ concentrations increase (with a decrease in pH), the peripheral chemoreceptors sense hypoxia in the arterial blood.
The glossopharyngeal nerve carries the impulses from the carotid bodies, while the vagus nerve carries those from the aortic bodies.
This network of neurons in the medullary respiratory centre sends signals through motor neurons to the respiratory muscles.
These signals help to restore Pco to a relatively constant level. This is done by increasing the rate of respiration to increase carbon dioxide elimination from the body and increase blood pH.
Exchange Of Gases
The exchange of gases takes place inside the lungs and in the tissues. Transportation of sufficient O2 from the lungs to the tissues is carried out by both the respiratory and circulatory systems simultaneously.
O2 is transported to the tissues, CO2 is transported from the tissues to the blood and eventually exhaled by the lungs.
Unique transport mechanisms not only enable these two processes (O2 uptake and CO2 release) to occur simultaneously, but they also facilitate each other. This exchange of gases in the tissues occurs by simple diffusion.
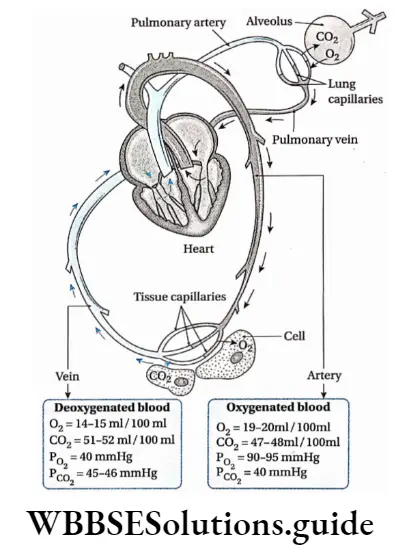
Exchange Of Gases In Lungs
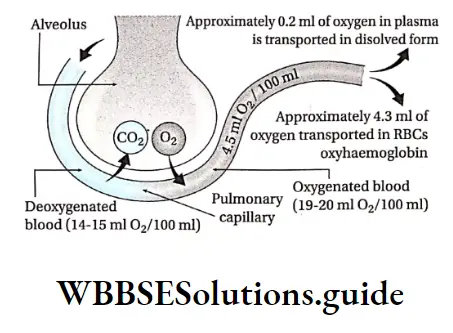
The exchange of gases in the lungs occurs through two steps, which are discussed below. Entry of oxygen from alveolar air to pulmonary capillaries Every 100 ml of oxygenated blood (arterial blood) contains 19-20 ml of oxygen and 100 ml of deoxygenated blood (venous blood) contains 14-15 ml of oxygen.
Therefore, the average difference in oxygen content between the arterial and venous blood is approximately 4.5 ml.
Hence, it is to be noted that during the circulation of blood in pulmonary capillaries, approximately 4.5 ml of oxygen (per 100 ml) from the alveolar air diffuses to pulmonary capillaries.
The partial pressure of oxygen (PO2) in alveolar air is 104 mm Hg. But PO2 in deoxygenated blood of pulmonary capillaries is 40 mm Hg. Due to this difference, oxygen diffuses through the squamous epithelium layer of the alveolus and enters into the blood of pulmonary capillaries.
This process of diffusion continues until PO2 in pulmonary capillaries increases to 100-104 mm Hg.
But, generally, this does not happen because some amount of oxygen gets absorbed by the alveolar tissue layer. So, the PO2 in pulmonary capillaries is approximately 90-95 mm Hg.
Pulmonary shunt
Pulmonary shunt occurs when the alveoli and lungs are perfused with blood but due to some reason gaseous exchange (ventilation) cannot take place.So the pulmonary shunt is a route through which blood perfuses unventilated shunt.
Carbon Monoxide Poisoning
Carbon monoxide has 250 times more affinity towards haemoglobin than oxygen. In the presence of carbon monoxide, haemoglobin reacts fast and forms a carboxyhaemoglobin compound. [CO + Hb = CO.Hb].
As a result, the oxygen-carrying capacity of blood reduces and oxygen content decreases in tissues (hypoxia).
This results in increased CO2 content (asphyxia) and may prove fatal. Generally, igniting a fire or stove in a closed room causes incomplete combustion, leading to the formation of carbon monoxide. This CO2 combines with the blood, causing carbon monoxide poisoning.
A person affected by carbon monoxide poisoning is treated by supplying a mixture of oxygen and carbon dioxide. This mixture helps to bind haemoglobin, thereby releasing carbon monoxide from haemoglobin.
Release of carbon dioxide from pulmonary capillaries to alveolar air
Every 100 ml deoxygenated blood contains 52 ml carbon dioxide in different forms, such as bicarbonate (in red blood cells and blood plasma), carbamino compound and a smaller amount in dissolved state.
During the circulation of blood in pulmonary capillaries, 5 ml of carbon dioxide per 100 ml of deoxygenated blood is released in the alveoli.
The PcO2 of deoxygenated blood is approximately 45-46 mm Hg. However, the Pco of alveolar air is approximately 40 mm Hg. Due to this difference, carbon dioxide from deoxygenated blood diffuses into alveoli.
Exchange Of Gases In Other Parts Of The Body
The exchange of gases in other parts of the body occurs through two steps, which are discussed below.
Entry of oxygen from blood capillaries to its associated tissues
Oxygen enters the associated tissues from the blood capillaries in the following steps—
- At first, oxygen from oxygenated blood in capillaries of different body parts diffuses in plasma and then to associated viable cells.
- The PO2 in blood capillaries is approximately 90-95 mm Hg, but pO2 in tissues is 40 mm Hg.
- Due to the pressure gradient, O2 diffuses from the blood to the tissues.
- 4.5 ml O2 per 100 ml of oxygenated blood diffuses in tissues and helps in oxidation. This 4.5 ml O2 is formed from 0.2 ml dissolved O2 in blood plasma, and approximately 4.3 ml from the dissociation of oxyhaemoglobin.
Conditions needed for the dissociation of oxyhaemoglobin are—a decrease in an increase in Pco in tissues, an increase in temperature in tissues and low pH.
Release of carbon dioxide from the tissues to blood capillaries Carbon dioxide is mainly generated during the oxidation of glucose in living cells.
Carbon dioxide diffuses from tissues to blood plasma and then to its associated capillaries. Carbon dioxide content is 48 ml per 100 ml of oxygenated blood and 52 ml per 100 ml of deoxygenated blood.
During the circulation of 100 ml of blood through various capillaries throughout the body, it collects 4-5 ml of carbon dioxide from tissues.
Pcc,2 in tissues is 46 mm Hg, but Pcc,2 in deoxygenated blood is 40 mm Hg. Due to this pressure gradient, carbon dioxide diffuses from tissues to blood capillaries.
This balance is maintained in order to transport carbon dioxide from tissues to capillaries.
Transport Of Gases
- The transportation of oxygen, from the atmosphere to the individual cells, occurs through a series of steps.
- The heart, lungs and blood circulation generate a flow of oxygenated blood to the tissues to maintain aerobic metabolism.
- However, oxygen transportation occurs with the concomitant expulsion of carbon dioxide.
- For this transportation, some respiratory pigments play an important role. In this section, the respiratory pigments and the process of transportation have been discussed.
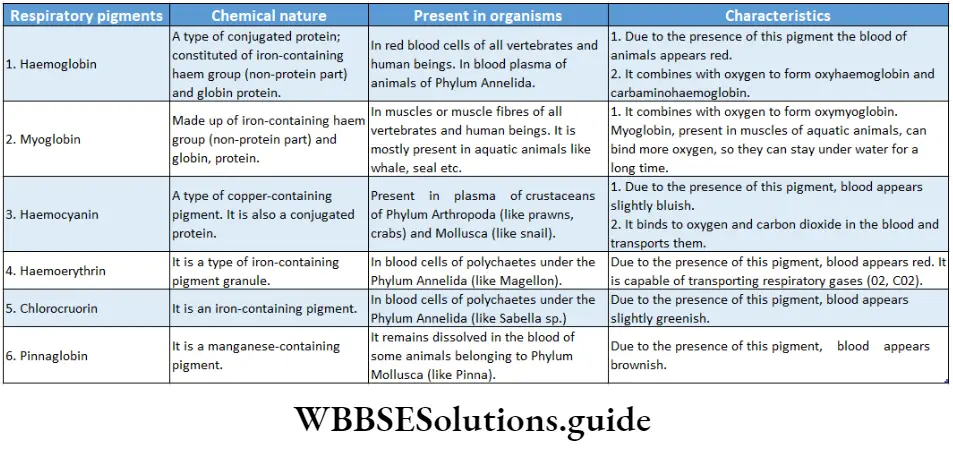
Respiratory Pigments
The pigments present in animal bodies that carry O2, and CO2 and transport them for cellular respiration are called respiratory pigments.
The different types of respiratory pigments, their chemical nature and features are discussed below in the table.
Transport Of Oxygen
O2 transport system in the body consists of the lungs and the cardiovascular system.
Deoxygenated blood releases carbon dioxide and gets saturated by oxygen. This oxygenated blood enters the left ventricle of the heart by the pulmonary vein.
From the heart, the blood passes through the aorta, arteries and arterioles and reaches capillaries surrounding different body organiser
Finally, it reaches the associated tissues. At normal atmospheric pressure, the number of oxygen molecules present in each litre of blood is normally equivalent to 200 ml of pure gaseous oxygen.
Oxygen is present in two forms—
- As dissolved form and
- A combined form (oxyhaemoglobin). Both these forms have been discussed below
Transport As Dissolved Gas
- Oxygen diffuses passively from the alveoli and dissolves in the plasma. In its dissolved form, O2 maintains its molecular structure and gaseous state.
- The quantity of oxygen that dissolves in a fluid, such as blood, is predicted by gas laws (Henry’s law and Graham’s law) and it depends on the partial pressure of gas and temperature.
- In a healthy normal adult, approximately 0.3 ml of O2 is dissolved in 100 ml of blood.
- This is commonly expressed as 0.3 volume per cent (vol%), where the vol% is equal to the millilitre of O2 per 100 ml of blood.
- Only a small percentage of O2 is carried in this dissolved form, and its contribution to total O2 transport is small.
Transport As Oxyhaemoglobin.
Amount to be transported: As oxygen is relatively insoluble in water, only 3 ml can be dissolved in every 1 L of blood at the normal arterial PO2 of 100 mm Hg.
Among the rest 197 ml (out of 200 ml total oxygen) of oxygen in a litre of arterial blood is transported through the erythrocytes as oxyhaemoglobin.
So, more than 98% of oxygen content is transported through erythrocytes as oxyhaemoglobin.
Formation of oxyhaemoglobin: The dynamics of the reaction of haemoglobin with O2 makes it a suitable O2 carrier.
Each haemoglobin (Hb) molecule is a protein made up of four subunits joined together. Each of these subunits consists of a molecular group known as haem and a polypeptide attached to it.
Haem is a porphyrin ring complex that includes one ferrous ion (Fez+). Each of the four ferrous ions in Hb can reversibly bind one O2 molecule each.
In normal adults, most of the haemoglobin molecules contain two or two chains.
The binding of O2 to haemoglobin alters the absorption of Hb, which is responsible for the change in colour between oxygenated arterial blood (HbOz) and deoxygenated venous blood (Hb).
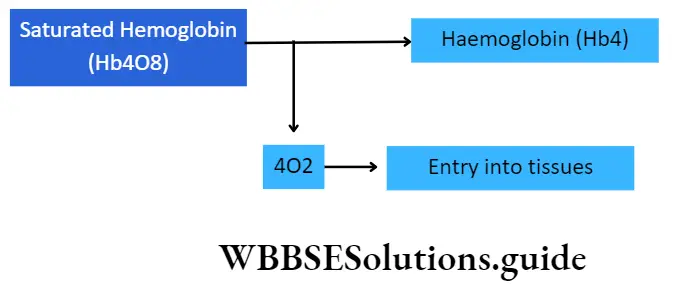
The binding of four O2 molecules to each Hb molecule forms a complex called oxyhaemoglobin. This happens in four stages which are as follows
⇒ \(\left.\begin{array}{l}\text { (1) } \mathrm{Hb}_4+\mathrm{O}_2 \longrightarrow \mathrm{Hb}_4 \mathrm{O}_2 \\ \text { (2) } \mathrm{Hb}_4 \mathrm{O}_2+\mathrm{O}_2 \longrightarrow \mathrm{Hb}_4 \mathrm{O}_4 \\ \text { (3) } \mathrm{Hb}_4 \mathrm{O}_4+\mathrm{O}_2 \longrightarrow \mathrm{Hb}_4 \mathrm{O}_6\end{array}\right\} \begin{aligned} & \text { Unsaturated } \\ & \text { oxyhaemoglobin }\end{aligned}\)
⇒ \((4) \mathrm{Hb}_4 \mathrm{O}_6+\mathrm{O}_2 \longrightarrow \mathrm{Hb}_4 \mathrm{O}_8 \quad Saturated oxyhaemoglobin\)
The readily reversible binding of O2 to haemoglobin facilitates the delivery of O2 to the tissues from the blood. In saturated conditi ons, 1g of haemoglobin can transport 1.34 ml of oxygen.
Conditions required for oxyhaemoglobin Formation:
- Increase in PO2 in alveolus;
- Decrease in PcO2 in alveolus;
- High pH in blood; Maintenance of warm condition in lungs.
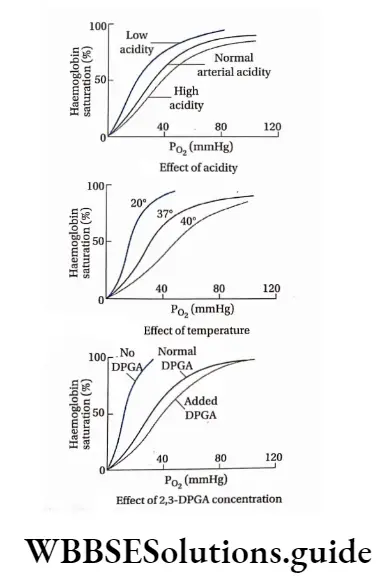
The oxygen dissociation curve or ODC
The graph in which the partial pressure of O2 (PO2 is plotted against the X-axis and percentage saturation of haemoglobin (Hb) by O2, along the Y-axis to determine the rate of O2 binding to haemoglobin is called the oxyhaemoglobin dissociation curve or oxygen dissociation curve or ODC.
The O2 molecules present in the pulmonary capillaries of human lungs mostly bind with haemoglobin to form oxyhaemoglobin.
The formation of oxyhaemoglobin is dependent on various factors, such as PO2 Pcc,2, H+ ion concentration in blood, temperature, etc.
The curve, obtained by plotting oxyhaemoglobin formation against PO2 is S-shaped or sigmoid. The effect of the factors stated above can be studied by this plot.
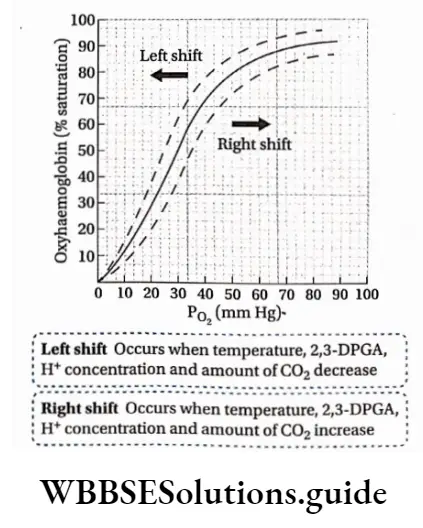
Reasons behind the sigmoidal shape of the oxygen dissociation curve: Each haemoglobin molecule contains four haem groups that can bind with four O2 molecules, at the most.
The binding occurs sequentially in the following manner—
The binding of the first haem in the Hb molecule with O2 occurs slowly so that no change in ODC occurs. However, this changes the structure of haemoglobin and increases the affinity of the second haem for O2.
Oxygenation of the second haem increases the affinity of the third and these reactions occur easily. As a result, ODC shifts to the right.
When PO2 is 25 mm Hg, Hb becomes 50% saturated by O2 At this portion of the curve, a large amount of O2 is released from haemoglobin with only a small change in PO2. This response facilitates the diffusion of O2 to the tissues.
Breathing and exchange of gases chapter summary with important points
The point on the curve at which 50% of a haemoglobin molecule is saturated with O2 (two oxygen molecules on one Hb molecule) is called the P50.
After binding of the three haem groups, however, binding of the fourth O2 molecule is a bit difficult, this type of binding is known as co-operative binding.
After this binding, ODC becomes almost plateau. From this point, a further increase in PO2 produces only a smaller increase in oxygen binding.
The significance of the flat portion of the ODC is that a drop in PO2 from about 100 mm Hg to about 60 mm Hg still results in a haemoglobin saturation of more than 90%. This virtually ensures adequate O2 transport.
Factors controlling the oxygen dissociation curve
Three important factors that affect ODC are pH, CO2, temperature and concentration of 2,3-diphosphoglycerate (2,3-DPGA).
- pH: A decrease in pH shifts ODC to the right (enhancing O2 dissociation) whereas an increase in pH shifts the curve to the left (increasing O2 affinity). During cellular metabolism, CO2 is released into the blood and therefore hydrogen ion concentration increases and thus, a decrease in pH occurs.
- CO2: An increase in CO2 concentration leads to an increase in H+ ion concentration. This causes ODC to shift to the right. CO2 has a direct effect on haemoglobin. This effect is known as the Bohr effect.
- Temperature: The body temperature increases during muscular exercise. This effect shifts the dissociation curve to the right and it enables more O2 to be released in the tissues. When the weather is cold, a decrease in body temperature shifts the O2 dissociation curve to the left (higher Hb affinity).
- 2,3-Diphosphoglycerate (2,3-DPGA): 2, 3-Diphosphoglycerate is produced during glycolysis. It is found abundant in red blood cells. The affinity of 2, 3-DPGA for Hb is greater than that of O2 As a result, 2, 3-DPGA directly competes with O2 and binds to the p chain of Hb binding sites. This reduces the transport of oxygen by Hb.
⇒ \(\mathrm{HbO}_2+2,3-\mathrm{DPGA} \rightleftharpoons \mathrm{Hb}-2,3-\mathrm{DPGA}+\mathrm{O}_2\)
Bohr effect
It is the phenomenon in which an increase of carbon dioxide in the blood and a decrease in pH results in a reduction of the affinity of haemoglobin for oxygen.
It results in a right shift of the ODC reflecting the release of oxygen from haemoglobin. The Bohr effect is closely related to the fact that deoxygenated haemoglobin binds H+ more actively than oxygenated haemoglobin.
This phenomenon was first described by the Danish scientist Christian Bohr(1904).
Thus, the oxyhaemoglobin dissociation curve is shifted to the right. Conditions that increase 2, 3-DPGA include hypoxia, decreased Hb concentration, and increased pH.
Haldane effect
Haldane effect states the effect of oxygen on carbon dioxide transport. This phenomenon describes the binding of oxygen to haemoglobin and promotes the release of carbon dioxide from carbaminohaemoglobin. This effect was first observed by J.S.Haldane(1914)
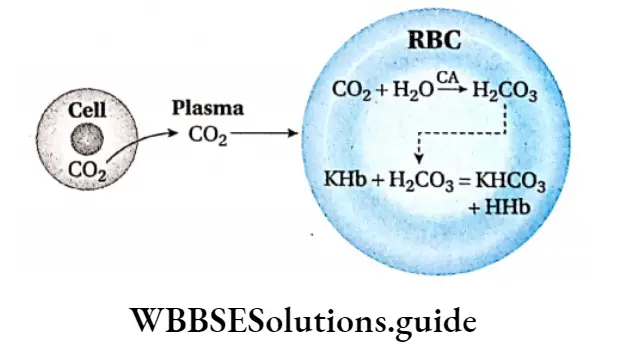
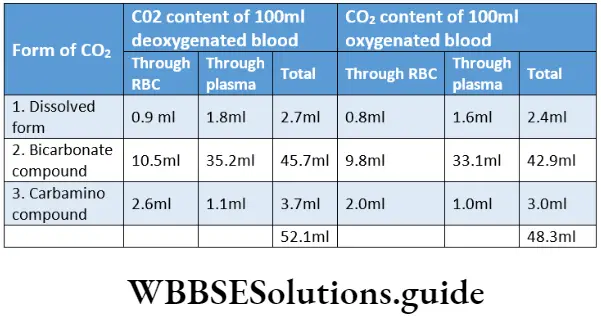
Transport of carbon dioxide
During cellular respiration, CO2 is produced and reaches the heart through blood vessels. From the heart, the deoxygenated blood comes to the lungs by pulmonary arteries.
The CO2 content is approximately 52.1 ml per 100 ml of deoxygenated blood and 48.3 ml per 100 ml of oxygenated blood.
CO2 is carried and transported through the blood in both plasma and red blood cells as three distinct chemical forms.
These are namely, bicarbonate (HC03 ), dissolved CO2 and carbamino protein complexes. In plasma, CO2 binds to various plasma proteins, and in red blood cells, CO2 binds to haemoglobin. By far, the predominant transport mechanism of CO2 is HC03 within RBC.
Transport as bicarbonate (HC03)
Every 100 ml of deoxygenated blood containing 45.7 ml of CO2 and 100 ml of oxygenated blood containing 42.9 ml CO2 is transported as different bicarbonate compounds by blood and plasma.
Formation of bicarbonates in blood plasma: The plasma of 100 ml each of deoxygenated and oxygenated blood contains 35.2 ml and 33.1 ml CO2 respectively, as bicarbonate compounds. The reactions that are involved are as follows.
The plasma protein (Pr) of blood plasma remains bound to sodium (Na) which is designated as NaPr. This reacts with H2C03 to form sodium bicarbonate (NaHC03)
⇒ \(\begin{gathered}
\mathrm{CO}_2+\mathrm{H}_2 \mathrm{O} \rightarrow \mathrm{H}_2 \mathrm{CO}_3 \\
\mathrm{NaPr}+\mathrm{H}_2 \mathrm{CO}_3 \rightarrow \mathrm{NaHCO}_3+\mathrm{HPr}
\end{gathered}\)
Blood plasma contains alkaline phosphates such as disodium hydrogen phosphate (Na2HPO4). This Na2HPO4 reacts with carbonic acid to form sodium bicarbonate (NaHCO3) and sodium dihydrogen phosphate (Na2PO4).
⇒ \(\mathrm{Na}_2 \mathrm{HPO}_4+\mathrm{H}_2 \mathrm{CO}_3 \rightarrow \mathrm{NaHCO}_3+\mathrm{NaH}_2 \mathrm{PO}_4\)
Formation of bicarbonate compound in red blood cells: RBC of 100 ml deoxygenated and oxygenated blood contain 10.5 ml and 9.8 ml of CO2 respectively, as bicarbonate compounds.
CO2 in RBCs is transported as potassium bicarbonate (KHCO3). Due to the presence of the enzyme carbonic anhydrase, CO2 and water react to form carbonic acid. Carbonic acid dissociates to form bicarbonate and H+ ions.
Hb forms the compound KHb with potassium in RBC which then reacts with carbonic acid. Bicarbonate ions react with potassium to form potassium bicarbonate and the H+ ions bind to haemoglobin to form a HHb complex.
Transport as carbamino protein complexes Each 100 ml of deoxygenated and oxygenated blood contains 3.7 ml and 3.0 ml CO2 respectively, as carbamino compounds.
Out of these, some amount of CO2 remains in plasma as carbamino-plasma and some of the amount remains in RBCs as carbaminohaemoglobin.
In blood plasma: 100 ml of deoxygenated blood contains 1.1 ml and 100 ml of oxygenated blood contains 1.0 ml of carbon dioxide which is transported as carbamino compounds. The amino acids of plasma proteins react with CO2 to form carbamino proteins.
⇒ \(
\mathrm{Pr} \cdot \mathrm{NH}_2+\mathrm{CO}_2 \longrightarrow \mathrm{Pr} \cdot \mathrm{NH} \cdot \mathrm{COOH}
(Carbamino protein)\)
In red blood cells: 100 ml of deoxygenated blood j contains 2.6 ml of CO2. 100 ml oxygenated blood contains 2.0 ml of carbon dioxide which reacts with Hb of RBCs to form carbaminohaemoglobin. In this case, carbonic anhydrase plays no role.
Transport as dissolved CO2
The remaining 5% of the CO2 is carried in the blood as dissolved gas. Although CO2 is 20 times more soluble in water than O2, the dissolved form of CO2 still constitutes a small fraction of the total transported CO2.
Hence, the dissolved form of CO2 is much more important in CO2 transport than the dissolved form of O2. Cv dissolves in red blood cells and blood plasma to form carbonic acid.
RBCs and plasma of 100 ml of deoxygenated blood contain 0.9 ml and 1.8 ml of CO2 respectively, i.e., a total of 2.7 ml in dissolved state. RBCs and plasma of 100 m oxygenated blood contain 0.8 ml and 1.6 ml CO2 respectively, i.e., a total of 2.4 ml in the dissolved state.
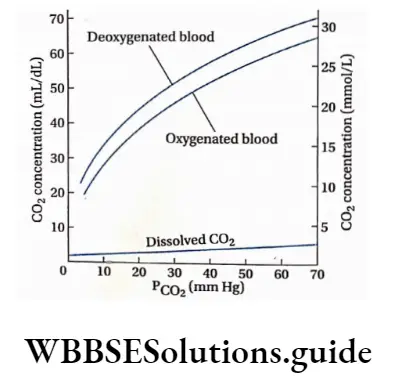
Carbon Dioxide Dissociation Curve
In contrast to the behaviour of O2, the dissociation of CO2 from blood is almost directly proportional to the Pco.
Hence, the dissociation curve for CO2 is linear, the saturation of haemoglobin with O2 has a major effect on the CO2 dissociation curve.
Although O2 and CO2 both bind to haemoglobin at different sites, deoxygenated haemoglobin has a greater affinity for CO2 than oxygenated haemoglobin.
The deoxygenated Hb more readily forms carbamino compounds and also binds faster with free H+ ions that are released during the formation of HCO2. Thus, deoxygenated blood (venous blood) freely takes up and transports more CO2 than oxygenated arterial blood.
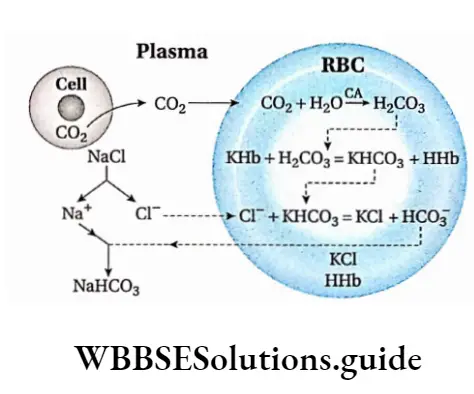
Chloride Shift Or Hamburger Phenomenon
When CO2 enters the cellular capillaries, NaCI in blood plasma breaks down to release Cl” ions which enter into the RBC.
The reverse phenomenon occurs in the lungs. As CO2 enters pulmonary capillaries, RBCs release Cl- to regenerate NaCI in plasma.
This phenomenon regarding the shifting of chloride ions is known as the chloride shift or Hamburger phenomenon. It was discovered by Hamburger in 1927.
Chloride Shift In Cellular Capillaries
Cations like K+, and Na+ cannot move across the membrane of RBCs but anions like Cl-, and HCO3 can. Carbon dioxide produced in tissues of body parts, other than the lungs, enters into the blood.
The majority of this carbon dioxide enters into the RBC. Due to the presence of the enzyme, carbonic anhydrase (CA) in RBCs, carbon dioxide reacts with water to form carbonic acid (H2C03).
H2C03 produced in RBC reacts with haemoglobin bound to potassium (KHb) to form potassium bicarbonate (KHCO3) and haemoglobinic acid (HHb). Due to the production of KHC03, the content of bicarbonate in RBCs increases and it becomes slightly alkaline.
To maintain the pH of blood, either K+ ions should be released from the blood or some anions like Cl” should enter the blood.
Since K+ ions cannot move across the membrane of RBC, NaCI dissociates and releases Cl” ions. These ions penetrate through the membrane of RBC and react with KHCO3 to form KCI and HCO3.
Due to the formation of HCO3 in RBCs, it becomes slightly acidic. To neutralise this, HCOJ diffuses into blood plasma and reacts with Na+ to form sodium bicarbonate (NaHCO3)
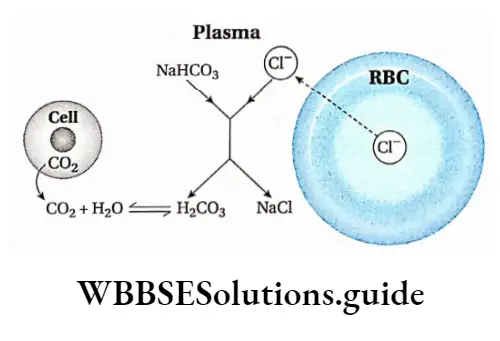
Chloride shift in lung capillaries
Cl- from RBCs of pulmonary capillaries gets released into blood plasma. This Cl- reacts with NaHCO3 to form NaCl and H2CO3.
This H2CO3 dissociates to produce carbon dioxide that diffuses into alveoli. Chloride shift occurs reversibly in the capillaries of other body parts except the lungs.
Regulation Of Respiration
Respiration is regulated by a number of factors which have been discussed separately.
Central chemoreceptors: The imbalance of gaseous components (O2, CO2) in blood and CSF causes stimulation of these receptors in the spinal cord and hypothalamus. Details have been discussed in previous sections.
Peripheral chemoreceptors: Receptors in blood vessels sense an imbalance in gaseous components (O2, CO2) in blood and body fluid. These receptors send signals to the respiratory centres in the brain and thus control respiration. Details have been discussed in previous sections.
Baroreceptors: Baroreceptors in blood vessels, tubular organs, muscles, joints of bones etc., can distinguish between expansion and contraction, thus controlling respiration.
Reflex: Reflex in alveoli, visceral pleura, respiratory tract etc., generates sensory impulse that triggers the respiratory centres in the brain, thus controlling respiration.
Temperature: The rate of respiration is proportional to body temperature. On increasing temperature, the rate of respiration also increases. Again, on decreasing the temperature, the rate of respiration decreases too.
NEET breathing and exchange of gases revision notes with MCQs
Blood pressure: The rate of respiration is also proportional to blood pressure. On increasing the blood pressure, the rate of respiration increases and vice-versa.
Pain: Due to excess pain, respiration may stop. Pain in visceral organs reduces the rate of respiration.
Tracheal stimulation: Due to tracheal stimulation, respiration may cease for a moment and this, in turn, causes a cough or sneeze.
Stimulation in the limbic system: The limbic system in the human brain gets excited due to emotional stimuli which influences respiration accordingly.
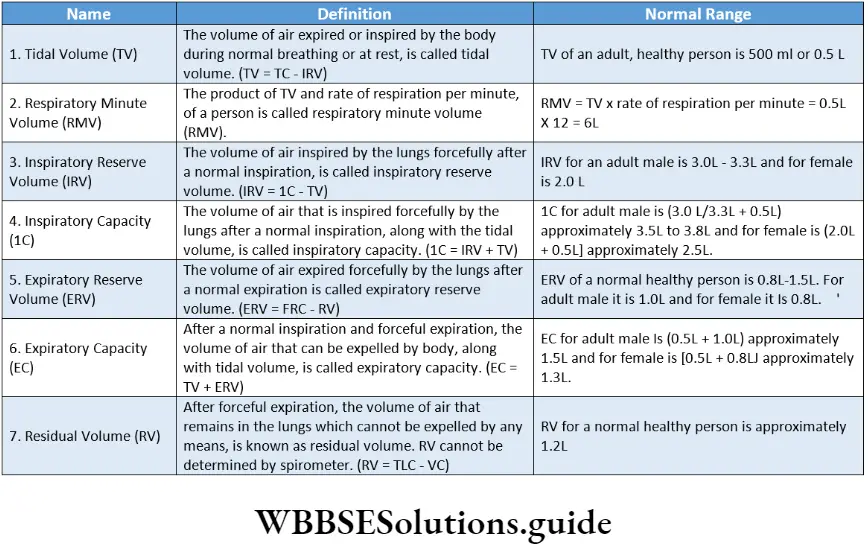
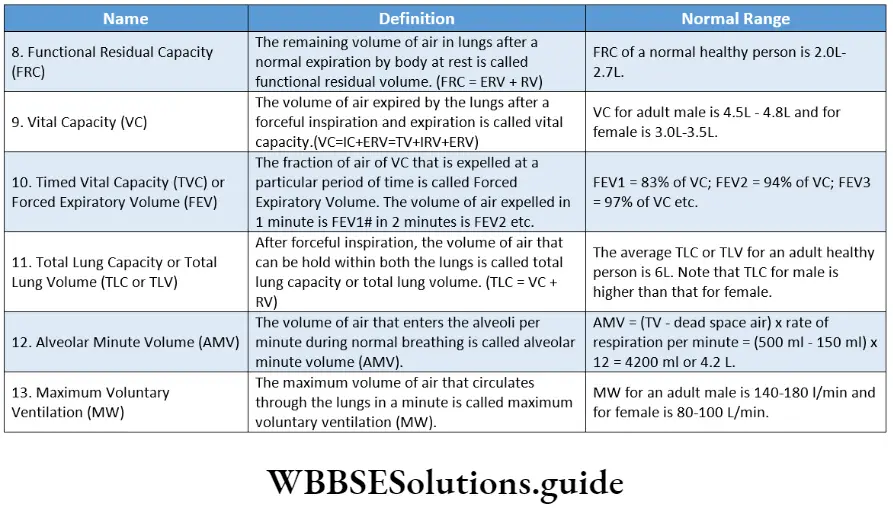
Respiratory And Pulmonary Volumes
The total amount of air that the lungs can accommodate is divided into a number of volumes.
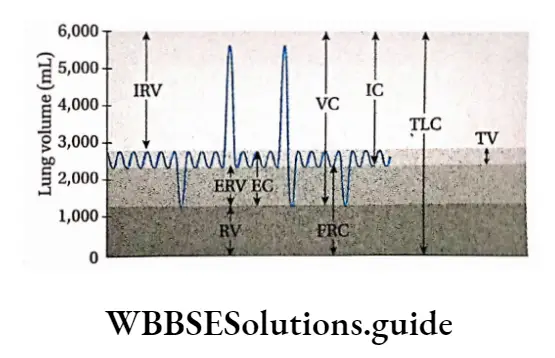
Combinations of these lung volumes can be used to determine lung can accommodate varies primarily with the age, height and sex of the individual.
The various lung volumes and capacities and their definition.
Importance of RV
The residual volume maintains gaseous exchange between O2 and CO2 in the alveoli and associated pulmonary capillaries during breathing. Otherwise, deficiency of oxygen may be observed due to oxidation of glucose and cellular respiration would be hampered.
Release of RV
RV cannot be released in living conditions. However, if holes are made in the wall of the thoracic region or in the pneumothorax region of a person, atmospheric air enters the thoracic cavity through these holes.
As a result, air pressure in the thoracic cavity increases. This causes the collapse of the lungs and RV releases from the body. During open heart surgery, the lungs collapse totally. RV is also released during death.
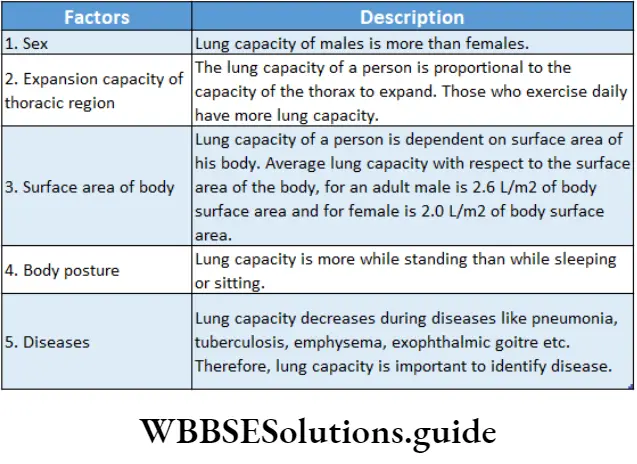
Instrument for measurement of pulmonary volume—spirometer
A spirometer is an instrument used to measure different volumes of air involved in breathing. spirometry is a basic test for the study of lung functioning. Basically, there are two vessels in a spirometer—
A larger vessel containing water and having a breathing hose attached to it,
A smaller vessel inverted and suspended in the water. A counterweight and indicator are attached to the inverted chamber.
The indicator is associated with a machine named Kymograph. The kymograph cylinder is provided with graph paper which records data.
This is known as spirogram. Air blown into the inverted chamber will cause it to rise, thus moving an indicator arrow along the horizontal scale.
It is calibrated in litres to give lung volume measurements. If the spirometer index moves by 1 mm up-down, it indicates 30 ml of air. It is essential for the evaluation and monitoring of respiratory diseases.
Dead Space
Dead Space Definition: The part of the respiratory system which does not take part in the gas exchange process is called dead space.
Types: Based on the volume of air contained in these spaces, dead spaces are classified into two types—
Anatomical dead space and physiological dead space
Anatomical dead space and anatomical dead space air: The airways from the human nasal passage to the terminal bronchiole where no gaseous exchange with pulmonary capillaries takes place, are known as anatomical dead space.
The air present in anatomical dead space is known as anatomical dead space air. In human beings, it is approximately 150 ml in volume and constitutes 20% – 30% of TV (tidal volume).
Physiological dead space and physiological dead space air: The frontal part of the lungs where alveoli cannot take part in gas exchange due to uneven distribution of several respiratory disorders seen in the human body capillaries is known as physiological dead space.
The air present in physiological dead space is known as physiological dead space air.
For a normal healthy individual anatomical dead space air volume is almost the same as physiological dead space air volume.
Its normal volume is approximately 150-200 ml.
Importance: Inspired air becomes saturated with water vapour, in the anatomical dead space and enters the alveoli.
Some particles of size more than 0.2 mm are trapped in that space before entering the alveoli.
An increase in physiological dead space air and air volume indicates diseased or ill-condition alveoli.
It helps to determine lung diseases. For example, in a respiratory disorder called emphysema, blood circulation decreases due to the presence of coagulated blood. This means during any lung disease physiological dead space air volume increases.
Apneustic breathing: It is another abnormal breathing pattern that is characterised by sustained periods of inspiration, separated by brief periods of exhalation.
Loss of inspiratory-inhibitory activities is the mechanism responsible for this type of ventilatory pattern. Individuals with central nervous system injury.
Mechanism of breathing and transport of gases notes
Disorders Related To Respiratory System
Several respiratory disorders are seen in the human body and some of these disorders.
Asthma
Asthma is a disease of the bronchi and bronchioles that is marked by wheezing, breathlessness, and sometimes cough and expectoration of mucus.
Asthma Types and causes: There are two types of asthma that are discussed below.
Allergic or atopic asthma: This type of asthma generally occurs due to air pollution. Different foreign substances and allergens, such as dust particles, pollen grains etc., on entering the body cause allergy.
In this condition, the number of eosinophils and mast cells increases. They secrete leucotriene, histamine etc. These substances constrict the bronchioles and cause allergic asthma. Generally, this type of asthma is observed during childhood.
Non-atopic or idiosyncratic asthma: This type of asthma affects elderly people. It is caused due to viral infection, polyp formation or excessive smoking. During viral infection, inflammation of the wall of bronchioles occurs.
As a result, the diameter of the inner cavity of bronchioles reduces and non-atopic asthma is observed.
The asthmatic trauma becomes frequent during dawn or late night. Cold air enhances the chances of such asthma. Anxiety, mental pressure etc., also increase the chances of this disease.
Asthma Symptoms:
- Contraction of smooth muscles of the wall of bronchioles occurs which reduces the diameter of the lumen of bronchioles. So, the circulation of air through it gets obstructed and this creates difficulty in breathing.
- Inflammation of the wall of bronchioles occurs. From that layer, a thick mucus is secreted that sticks to the smaller cavities of bronchioles. This mucus obstructs the airways and causes dyspnoea (painful respiration).
- Asthmatic patients face difficulty in expiration than inspiration and in some cases, whistling sound is observed during expiration.
- Tachycardia or an increase in the rate of heartbeat is observed.
- During chronic asthma, the skin may turn blue (due to deficiency of O2), and loss of consciousness, and respiratory arrest leading to death may also occur.
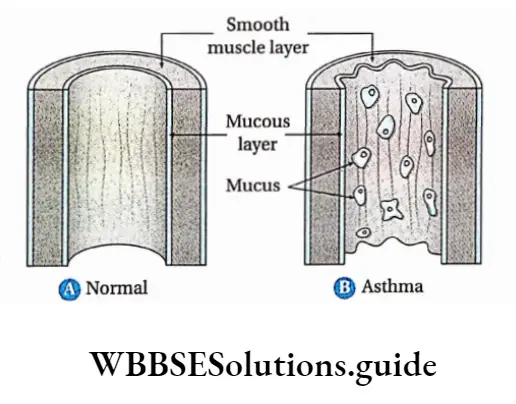
Asthma Prevention and Treatment:
- Air pollution and smoking are the two main causes of asthma. So, prevention of smoking and avoiding inhalation of polluted air are the two best possible ways to prevent asthma.
- Cold waves of air increase the disease. So, care should be taken that the patient is not exposed to cold air during dawn.
- At present, corticosteroids or other medicines are used to treat asthma. They act as bronchodilators.
- Homes should be cleaned and made germ-free or dust-free.
- The patient should not suffer from any anxiety or tension.
Emphysema
Emphysema is a chronic disease or disorder of the lungs due to which the elasticity of the walls of the lungs reduces, the lungs expand and the surface area for absorption of oxygen reduces.
Emphysema Causes:
- Cigarette smoking, air pollution, lung infections and some occupational hazards are the main causes of emphysema. It occurs due to the release of proteolytic enzymes as part of the inflammatory process that follows irritation of the lungs.
- The lungs actually undergo self-destruction by these proteolytic enzymes secreted by leukocytes in the lungs.
- In about 2% of cases, it’s a rare hereditary disease.
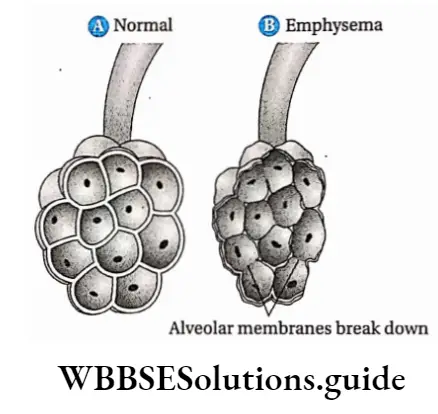
Emphysema Symptoms: The symptoms of emphysema.
- Reduction or loss of elasticity of the walls of the lungs: The elasticity of the walls of the lungs is reduced thereby causing narrow airways.
Excessive smoking leads to an increase in the number of macrophages. These macrophages secrete chemicals which attract WBCs. These WBCs then secrete elastase and other proteolytic enzymes. These enzymes cause damage to the lungs and reduce their elasticity.
Hypoxia: This occurs due to the malfunctioning of the lung tissue during emphysema and uneven blood flow due to the destruction of capillaries.
Enlargement of chest: Emphysema may lead to an enlarged or barrel-shaped chest.
Enlargement of heart: The right side of the heart is observed to be enlarged for people suffering from emphysema.
Types: The different types of emphysema are discussed below.
- Panacinar emphysema: In this case, walls of adjacent alveoli break down, alveolar tubules become swollen and intra-alveolar elastic tissue gets damaged.
- Centrilobular emphysema: In this case, bronchioles become thick and so when air enters these lobules (i.e., bronchioles and alveolar region) oxygen pressure reduces and hypoxia occurs.
- Interstitial emphysema: When air occupies intrathoracic tissue, the condition is known as interstitial emphysema. External wounds by knife or breaking of the rib cage, and asthma may create such conditions.
Emphysema Prevention and treatment: Currently no form of treatment can cure emphysema reverse the damage to the lungs, or even control the disease and its symptoms. However, emphysema can be prevented by avoiding cigarette smoking.
Antibiotics may be used to treat and prevent infections within the respiratory system. Special breathing exercises are often helpful and breathing equipment that delivers extra oxygen and medications may be provided for home use.
Corticosteroids or steroids are used to decrease the inflammation of the airway walls.
Occupational Respiratory Disorders
Occupational respiratory disorders are a group of disorders that are caused by long or brief exposure to toxic substances while working in coal mines, factories, etc.
Common occupational lung diseases include anthracosis, mesothelioma, occupational asthma, silicosis, and asbestosis.
Occupational respiratory disorders Symptoms: In the case of occupational diseases, different particulate matter enter, the lungs along with the inhaled air and get deposited on the walls of the lungs as well as those of the alveoli. As a result, the wall of the alveoli thickens. Due to this, gaseous exchange slows down, and difficulty in breathing and coughing are experienced.
Occupational respiratory disorders Types: Some occupational diseases are discussed below. Black lung disease or Anthracosis: The people who work in coal mines inhale minute particulate matter like small fine particles of coal during inspiration.
These particles deposit on the inner walls of the lungs and create a black layer over them. This disease is known as black lung disease or anthracosis. In this case, symptoms of bronchitis and emphysema can also be observed.
Asbestosis: Asbestosis is a respiratory disease that results from the presence of microscopic asbestos fibres in the air. These small asbestos fibres deposit on the lungs over time and can cause scarring or fibrosis of the lungs.
This scarring causes the lungs to stiffen and makes it hard to breathe. Earlier, asbestos was used widely as a fireproofing and insulating agent, whereby unwanted exposure has occurred, causing asbestosis.
Mesothelioma: Mesothelioma is a fatal type of cancer also caused by exposure to asbestos. Millions of construction and general industry workers have been exposed to asbestos fibres over a very long period of time, causing mesothelioma.
Usually, mesothelioma does not show up until 20 to 40 years after exposure. Most of the deaths resulting from the disease are the result of exposures that occurred decades ago.
Silicosis: People who work in gold, copper mines or factories where glass, slate etc., are manufactured, suffer from this disease.
It includes the deposition of silicon particles within the alveoli. WBCs and macrophage phagocytose silicon particles.
However, sometimes these particles may not get removed from the body. The X-ray plates of the lungs of patients suffering from this disease show an orange line, showing the presence of silica.
Byssinosis: The people who work in textile manufacturing industries for a long time, inhale thin fibres of cotton, jute, silk etc. These fibres enter the lungs and cause the disease byssinosis. The symptoms of this disease are breathing trouble, asthma, chest pain etc.
Prevention and treatment: To prevent these diseases, workers must be aware of the consequences. They must be provided with proper aprons, masks, gloves etc., that prevent them from coming in contact with this harmful substance.
Hypoxia
Hypoxia is a condition where the supply of oxygen to the tissues is less than the volume of oxygen required by them.
Hypoxia Types: It is mainly of four types. Each of them is discussed below
Hypoxic hypoxia: The reduction in oxygen content in the tissues due to a reduction in partial pressure of oxygen in the artery, is known as hypoxic hypoxia.
In this form of hypoxia, the arterial PO2 is below normal because either the alveolar Pÿ is reduced for environmental reasons such as altitude or the blood is unable to equilibrate fully with the alveolar air as in lung diseases.
Anaemic hypoxia: The reduction of oxygen content in the tissues due to anaemia and less haemoglobin in blood, is known as anaemic hypoxia.
Ischemic or hypokinetic hypoxia: Reduced oxygen content in tissues due to a reduction in blood flow because of a reduction in the activity of the heart, is known as ischemic or hypokinetic hypoxia.
Low cardiac output or perfusion (shock or ischemia), severe hypotension or low pulmonary venous outflow are examples of conditions that reduce circulation, seriously decreasing oxygen transport to the tissues.
Histotoxic hypoxia: The reduction in oxygen content due to the toxicity of tissues is known as histotoxic hypoxia, This is the most severe form of hypoxia.
Lung cancer
Cancerous growth may develop in epithelial cells lining the bronchi and bronchioles. It is most common among smokers.
The smoke released by burning tobacco in a cigarette, etc., contains harmful compounds that cause cancer.
Pulmonary Tuberculosis
Tuberculosis is an infectious disease which usually affects the lungs. It is also known as pulmonary tuberculosis. In humans, tuberculosis is caused by the bacterium Mycobacterium tuberculosis.
Mountain sickness and acclimatisation When a person reaches 12,000-18,000 ft altitude, he/she suffers from mountain sickness due to a lower level of oxygen. Its symptoms are headache, nausea and dyspnoea.
But after 4-8 days, several physiological changes are observed in his body. Due to these changes, the person can adjust to the changing environment. This phenomenon is called acclimatisation.
These physiological changes enable proper oxygen supply to the body. For example, the spleen contracts, the amount of blood in blood capillaries and the number of RBCs increase, and heart rate and rate of blood flow also increase.
As a result, sufficient oxygen reaches the tissues. Under the effect of erythropoietin, RBC production increases in the bone marrow.
Breathing And Exchange Of Gase Notes
- Allergy: It is a symptom that occurs due to hypersensitivity of the immune system which is caused by some environmental factors.
- Antibiotic: It is a drug or medicine which inhibits the growth of a micro-organism or destroys it.
- Bradycardia: Decrease in heart rate.
- Bronchodilator: A drug which helps in the widening of bronchi.
- Chemotherapy: Use of drug to treat any disease (mainly cancer)
- Corticosteroid: A class of steroid hormones which is produced in the adrenal cortex.
- Dyspnea: Painful respiration due to some reason.
- Pigment: It is a natural colouring matter of animal or plant tissue.
- Phonation: Production of speech sound.
- Radiation therapy: It is a process where high-energy particles or waves are used to treat cancer.
- Tachycardia: Increase in heartbeat
Points To Remember
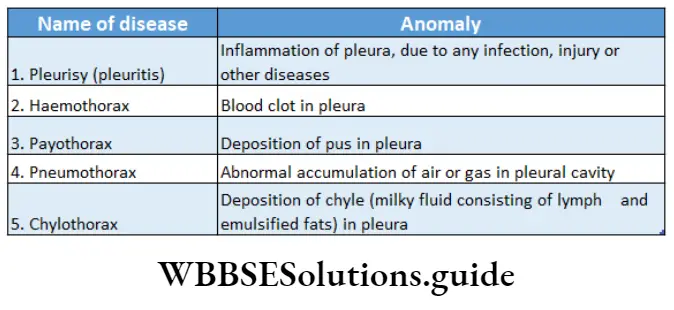
- Breathing is a physical process by which animals exchange gases between their body and the atmosphere.
- Human breathing takes place in two stages— inspiration and expiration.
- Each lung is covered by a double-layered membrane, known as pleura. The outer layer of the pleura is called the parietal pleura and the inner layer is called the visceral pleura.
- The nerve present in the diaphragm is the phrenic nerve
- Inflammation of the mucous membrane of the nasal passage is called rhinitis.
- Arrest of the functioning of the central nervous system along with its respiratory control systems is known as narcosis.
- Inflammation of the larynx is called laryngitis.
- Tuberculosis or TB occurs due to the infection of the bacteria Mycobacterium tuberculosis. The infection mostly occurs in the lungs and pleural membrane.
- Inflammation of bronchi is known as bronchitis.
- Infection and inflammation of the pleura are known as pleurisy.
- In dry pleura or pleuritis, the pleura becomes rough and the sound of rubbing against the rough pleura can be heard by a stethoscope.
- Fluid may deposit in interpleural space due to infection. This is known as pleural effusion. Haemothorax, pyothorax, chylothorax etc., are examples of pleural effusion.
- The abnormal condition in which the intrapleural region is filled with air is known as pneumothorax.
- Deposition of blood in the intrapleural region is known as haemothorax
- The deposition of pus between the two layers of the pleura is known as pyothorax.
- In the interpleural region, deposition of chyle i.e., the lymph appearing as a milky fluid, containing undissolved fat, is known as chylothorax.
- Although the volume of fluid deposition is not too high, yet occurrence of this condition is an indication of cancer (e.g., lymphoma) and choking of important lymphatic vessels.
- The presence of coal particles in the lungs causes bronchitis, emphysema etc. This condition is known as anthracosis.
- The disease that occurs due to inhalation and deposition of silicon compounds in the lungs, is known as silicosis.
- Inhalation of thin fibres of cotton, jute etc., for a long time causes byssinosis.
- A normal respiration rate is known as eupnea.
- The arterial oxygen that is utilised by the tissues is expressed by the oxygen utilisation coefficient. Its value is expressed in terms of the following ratio.
- ⇒ \(\frac{\text { Amount of oxygen utilised in tissues }}{\text { Amount of oxygen present in artery }} \times 100\)
- The normal value of the oxygen utilisation coefficient is 25%. But during exercise, its value increases to 75-80%.
- Dissociation of oxyhaemoglobin increases in the presence of 2, 3-BPG or 2, 3-bisphosphoglycerate. So, this compound is important for acclimatisation.
- The vital capacity of athletes and people living in mountains is more than the vital capacity of people living in plains. Due to their, necessity for more energy, they require more oxygen.
- Red blood cells contain zinc-containing enzymes known as carbonic anhydrase. It increases the rate of binding of RBC to carbon dioxide by 5000 times.
- Due to this reason, 70% of the amount of carbon dioxide that enters the blood from tissues, remains bound to red blood cells.
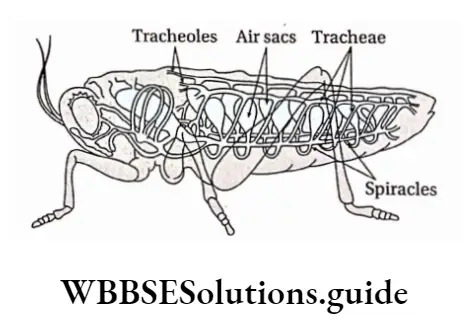
- Animals belonging to the class Insecta have a complex respiratory system called the trachea. By the trachea (10 pairs), they transport air to the tissues directly.
- Fishes breathe by gills. The blood vessels in the gills are so arranged that the flow of blood in the vessels is in opposite directions to the water flow.
- Inflammation of the alveoli of the lungs due to the infection of the bacteria Streptococcus pneumoniae is known as pneumonia.
- Lung cancer occurs due to excessive smoking. In this disease, cells of the lungs divide uncontrollably. As a result, blood vessels rupture and death occurs due to loss of blood (haemorrhage).
- A decrease in the normal rate of respiration is known as hypopnoea.
- An increase in the normal rate of respiration is known as hyperopnoea.
- A deficiency of carbon dioxide in the blood is known as hypocapnia.
- The absence of CO2 in the blood is known as apnoea.
- Excess carbon dioxide in the blood is known as hypercapnia.
- Painful respiration due to some reason is called dyspnea.
- Obstruction of respiration due to some reason is known as apnea.
