Body Fluids And Circulation Introduction
You Must Have Noticed that when your skin gets cut or pierced a red-coloured fluid oozes out from that particular region.
This fluid is called blood. But do you Know What blood Actually Is And what is its exact role inside your body as you are breathing you are taking in oxygen from the air.
The Oxygen That you take in is Transported To each cell Of Your body by blood. Apart From Oxygen Blood Transports Many Other Important Substances Like Nutrients Hormones etc., across the body.
Besides blood, there are some other fluids that also act as transporters. Together these are called body fluids.
Read and Learn More Class 11 Biology Notes
There are certain organs that help in the circulation of these fluids. The body fluids together with these organs, constitute the circulatory system. Evolution has produced larger animals with specialized organisers.
These organs carry out specific functions of the body. These organs would almost be useless without the circulatory system. This system consists of a network of thin tubes filled with body fluids that can deliver vital substances to all the cells of the body.
They also carry different waste products from all the cells to the excretory organs of the body.
These harmful waste products are removed continuously by the excretory organs outside the body.
The basic components involved in the circulatory system are—
- A fluid that flows through the system carrying materials across the body,
- A network of tubes that carries the fluid and
- A pump that maintains the flow of the fluid through tubes.
Body Fluids
Body Fluids Definition: Body fluids are those natural fluids present in the body through which the substances necessary for vital life processes, are transported across the body and metabolic waste products are removed from the body of higher animals.
Characteristics of body fluids: The body fluids provide an extracellular environment surrounding the cells.
It consists of a fluid compartment in which molecules are dissolved, and which serves as a matrix of polysaccharides and proteins.
Interaction between the intracellular and extracellular environments occurs across the plasma membrane.
Body Fluids Types: Mainly two types of body fluids are found in complex and higher organisms.
The types of body fluids are shown in the following chart.
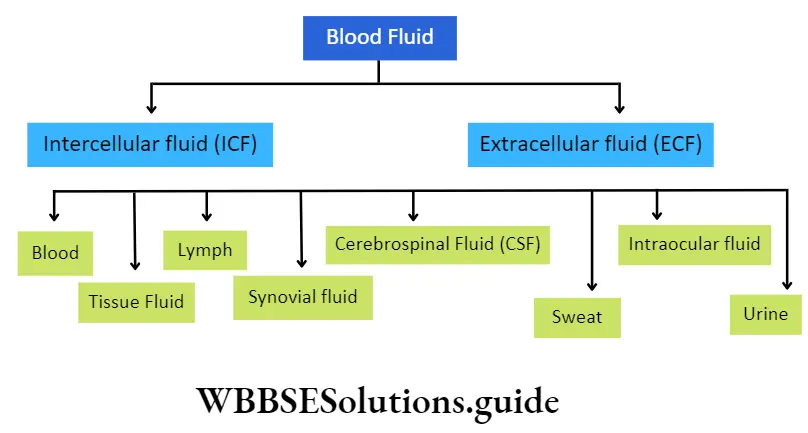
Intracellular Fluid (ICF): The fluid present within the cell is Known As Intercellular Fluid. Its Main Constituents are sodium, calcium, magnesium and chlorine ions.
Along with these ions, it also contains a certain amount of water, minerals, carbohydrates, lipids and proteins.
Extracellular fluid (EOF): The fluid present outside the cells is known as extracellular fluid. Extracellular fluid can be of different types.
They are as follows—
Blood: It is slightly alkaline, fluid connective tissue. It is the chief medium of transport of materials across our body.
Lymph: It is a straw-coloured, slightly alkaline, modified form of tissue fluid. Lymph helps to transport important substances to those areas of the body where blood cannot reach.
Interstitial or tissue fluid: This body fluid is present in between tissues, it is formed from the plasma by the process of diffusion and filtration. It contains glucose, fatty acids, minerals, etc. It provides important nutrients to the cells and takes away waste materials which are generated in them.
Definition: Blood is red-coloured, opaque, alkaline, fluid connective tissue that flows through the heart and the blood vessels.
Synovial fluid: The inner membrane of synovial joints (synovial membrane) secretes a viscous body fluid which is known as the synovial fluid. It reduces friction between the cartilage linings (articular cartilage) present at the joints, during movement.
Cerebrospinal fluid: It is a clear, colourless body fluid, present in the brain and spinal cord. It is produced from the choroid plexus (a branched network of cells) in the ventricles of the brain.
It acts as a shock absorber for the brain and spinal cord. It provides basic mechanical and immunological protection to the central nervous system. It also supplies nutrients to the cells of the brain and spinal cord.
Sweat: Sweat is a body fluid secreted by sweat glands. It contains about 99.5% of water. It also contains several ions such as sodium, potassium, chloride, etc.
Along with these ions, sweat also contains excretory products such as urea, uric acid, etc. It helps to regulate body temperature, acid-base balance in the body, excretion, etc.
Intraocular fluid: The fluid present in the eyeballs is known as intraocular fluid. It is of two types— aqueous humour and vitreous humour.
Urine: It is an acidic, pale, yellow-coloured body fluid found in vertebrates. It contains excretory products of the body.
Amount of body fluids in the body: The human body is composed of about 65-70% of water Approximately 67% of the total water content of our body is contained within the intracellular compartments of cells.
The remaining 33% of the total water content of the body is found outside the cells, in the extracellular compartments.
About 20% of this extracellular water is contained in the body fluids flowing through the vessels of the cardiovascular system. The remaining 80% of the extracellular water is present outside the vascular system and forms interstitial or tissue fluid.
Blood And Its Components
Blood is the chief medium of transport of essential metabolic substances and metabolic wastes, in the human body. This has been broadly discussed below.
Blood
Blood Definition: Blood is red-coloured, opaque, alkaline, fluid connective tissue that flows through the heart and the blood vessels.
Characteristics of human blood:
- Blood is a fluid connective tissue.
- Blood consists of white blood cells, red blood cells, and platelets, all suspended in a protein-rich complex solution, called plasma.
- Blood is red in colour due to the presence of an iron-containing pigment, haemoglobin.
- Blood is saline in nature due to the presence of high levels of NaC
- Blood is slightly alkaline (average pH is 7.4).
- At a temperature of about 15°C, the average specific gravity of blood in an adult male is 1.057 and in an adult female is 1.053.
- Blood is viscous and opaque.
Blood is known as a special type of fluid connective tissue. Why?
- Blood is produced from embryonic mesoderm tissue. 0 In blood, the amount of intercellular matrix (plasma) [55%] is more than that of the cellular components [45%].
- Blood connects different organs of the body.
- Human blood plasma contains 91%-92% water.
Amount of blood in the human body
- Blood circulates through blood vessels and the heart in the human body. Some amount of blood also remains stored in organs like the liver, spleen, etc.
- Blood covers 8-9% of the total weight of the human body. The amount of blood in normal adult males is about 5L and in females is about 4.5L.
- The amount of blood differs on the basis of age and health condition of the person.
Composition Of Blood
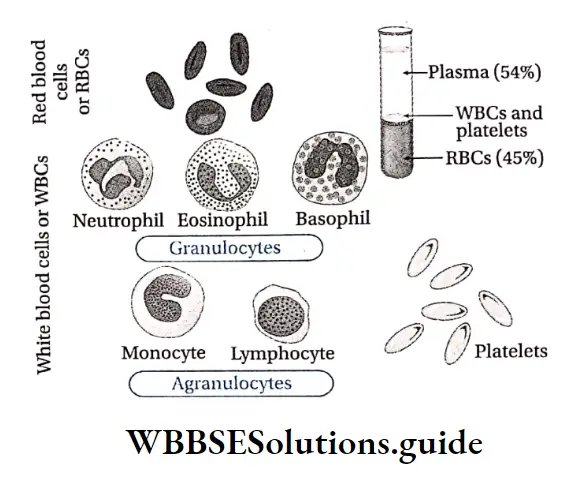
Blood contains a cellular portion known as formed elements, and a fluid portion, known as the plasma. The formed elements constitute approximately 45% of the total blood volume and the plasma accounts for the remaining 55%.
Red blood cells comprise most of the formed elements. The percentage of red blood cell volume to total blood volume in a centrifuged blood sample (a measurement called the haematocrit) is 36% to 46% in women and 41% to 53% in men.
Plasma and blood corpuscles are discussed under separate heads.
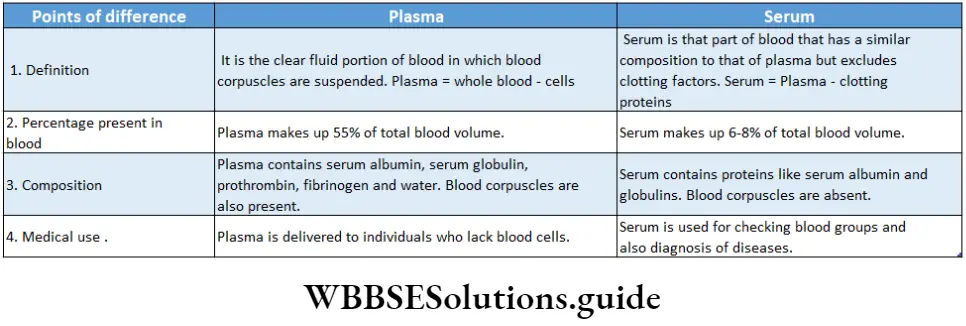
Plasma
Plasma Definition: Plasma is the straw-coloured, viscous fluid which occupies 55% of the total blood volume.
Characteristics of plasma: It contains ions, inorganic and organic molecules that are in transit to various parts of the body or which aid in the transport of other substances. Normal plasma volume is about 5% of body weight, or roughly 2.7- 3.2L in an adult human.
Plasma Colour: Plasma is a straw-coloured fluid. This is because plasma contains small amounts of pigments such as bilirubin and biliverdin, etc.
Different components and their functions:
Plasma is composed mostly of water (93%) with various dissolved solutes including carbohydrates, proteins, lipids, vitamins, minerals, hormones, etc.
The details of these components are as follows—
Water: Water acts as a solvent and transports different nutrients and other substances in a dissolved state. It also controls the blood pressure and amount of blood in the body.
Plasma protein: Human blood consists of four types of plasma proteins.
These are as follows—
Serum albumin: It regulates the osmotic pressure of blood plasma. This helps plasma to retain its water content. It also helps in the transport of hormones, amino acids, enzymes, phospholipids, calcium, etc.
Serum globulin: It helps to transport thyroxine and insulin hormones and fat-soluble vitamins. It also provides immunological protection in the form of antibodies.
Prothrombin: Helps in blood coagulation.
Fibrinogen: Helps in blood coagulation.
Mineral ions: Maintain osmotic balance, carry CO2, maintain pH of the body (buffering), help in blood clotting, conduct nerve impulses, regulate membrane permeability, etc.
Sugar: Sugar (primarily glucose) is present at specific concentrations in blood plasma and helps in metabolism.
Lipid: Cholesterol is the main lipid content of blood plasma. It is involved in the synthesis of biomembrane, vitamin D, steroid hormones and bile salts.
Enzymes: Enzymes such as protease, lipase, etc., are present in plasma and help in metabolism.
Hormones: Hormones such as insulin, thyroxine, glucagon, etc., are present in plasma. Insulin and glucagon regulate the glucose level in the body and thyroxine maintains the BMR.
Pigment materials: Pigments such as bilirubin and biliverdin are present in the blood. They give the yellow colour to the urine and faeces.
Functions of plasma: Various functions of the plasma are discussed below.
Transportation: Plasma is involved in the transportation of various substances such as—
Transportation of digested food: Digested food materials such as glucose, amino acids, etc., from the small intestine are carried by the blood capillaries and transported to the tissues through the blood plasma.
Transportation of vitamins, water and mineral salts: Plasma proteins can combine easily with many substances and play an essential role in their transport.
The names of some of these substances and the plasma proteins that help in their transportation are as follows thyroxine (by alpha globulin); cortisol (by transcortin); vitamins A, D, and E (by high and low-density lipoprotein); vitamin B12 (by transcobalamin); various drugs (by albumin); copper (ceruloplasmin); bilirubin (by albumin and alpha globulin); calcium present in the plasma partly (about 50%) bound to the plasma proteins for transport.
Transportation of hormones: In vertebrates, hormones secreted by the endocrine glands move to their target site through plasma.
Transportation of O2-CO2: Carbon dioxide from the tissues is collected by plasma and carried to the lungs for its elimination. A small amount of oxygen (about 3%) is transported through the blood plasma.
Transportation of excretory products: Waste products are taken up by plasma from the liver and other organs and are transported to the kidneys for removal from the body.
Regulatory functions: The regulatory functions of plasma are as follows—
Regulates acid-base balance (maintaining pH): Plasma proteins, electrolytes (phosphates, bicarbonates) and organic acids act as buffers to maintain constant blood pH.
Regulates viscosity: Plasma proteins maintain an important role in maintaining the blood viscosity owing to their size and shape.
Regulates blood pressure: Plasma proteins help to maintain a constant blood pressure in vertebrates.
Regulates osmotic pressure: Plasma proteins regulate the water balance in the body. Blood plasma can retain water and thus maintains the osmotic potential of blood.
Regulates body temperature: Plasma proteins help to regulate body temperature. They help in the distribution of heat to maintain a constant body temperature.
Defensive functions: The defensive functions of plasma are as follows—
Disease prevention: Gamma globulins are antibodies which provide natural immunity against pathogens.
Role in blood clotting and coagulation: Fibrinogen, prothrombin and other coagulation proteins along with platelet cells present in plasma, play an important role in the coagulation- of blood.
Coagulation stops bleeding from the wound and acts as a life-saving mechanism.
Other functions: Besides the above-mentioned functions, plasma also performs the following functions—
Moistening of tissue: Plasma helps to keep the tissue moist for better functioning.
Acts as protein store: Plasma proteins serve as protein stores and are utilised by the body tissues during fasting or inadequate protein intake and during excessive breakdown of body protein.
Nourishment of tissues: Plasma proteins are utilised by the leucocytes to produce telephones, which are essential substances for the nourishment of tissues.
Imparting genetic information: Plasma proteins can be used as important marker tools for studying population genetics as it show polymorphism (the condition of occurring in different forms).
Blood Corpuscles Or Formed Elements Of Blood
Different cellular components present in the blood are termed as the formed elements of the blood.
These include three types of blood corpuscles—leukocytes or white blood cells, erythrocytes or red blood cells, and thrombocytes or platelets.
Red Blood Corpuscle Or RBC Or Erythrocyte
Erythrocyte Definition: The blood corpuscles which contain the oxygen-carrying pigment called haemoglobin and are involved in the transport of respiratory gases, are known as red blood cells. Red blood cells are also known as erythrocytes (Greek, erythroid-xed; kytes-cell)
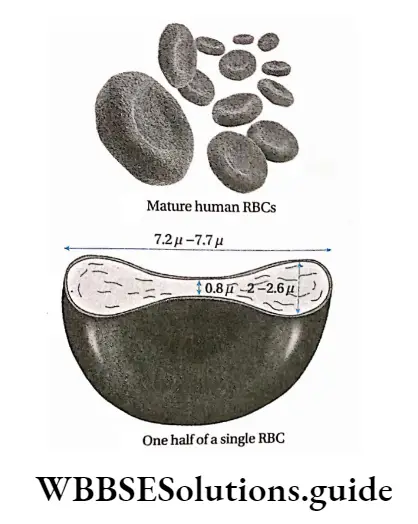
Erythrocyte Structural characteristics:
RBCs are biconcave, disc-shaped structures that are manufactured in the bone marrow of mammals.
On maturation, RBCs lose their nuclei before entering into the circulation.
In humans, mature RBCs lack cell organelles. RBCs in human beings are surrounded by a selectively permeable plasma membrane. The membrane is made up of lipids and proteins.
The activity of mature RBC in human beings increases due to the absence of a nucleus, endoplasmic reticulum (ER) and mitochondria
Erythrocyte Absence of nucleus: Due to the absence of; a nucleus, RBCs are biconcave. This increases the surface area of the cell, which in turn increases the absorption of O2.
But RBCs of some animals such as camel, elephant, etc., are nucleated.
Absence of ER: Due to the absence of ER, contraction of RBC increases and they can easily pass through the capillaries.
Absence of mitochondria: Due to the absence of mitochondria, the TCA cycle, terminal respiration and P -oxidation of fatty add do not take place in the RBCs.
So, the oxygen present in RBC is transported to different organs via haemoglobin, instead of being Used By The Cell Itself.
Erythrocyte Shape: Shape Of The RBC Optimizes Its Surface Area and Increases The Efficiency Of Gaseous Exchange.
It maintains its shape by virtue of its complex membrane the skeleton which consists of an insoluble mesh of fibrous Proteins Attacxhed To The Inside Of The Plasma membarane.
Erythrocyte Size: Each human red blood cell is about 7.5 pm in diameter, and 2.2 pm thick. It has 120 pm2 surface area and 87 pm3 volume.
Erythrocyte Number: RBC count varies according to the age and gender of a person. Normally, the total RBC count is 4.8 million per cubic millimetre of blood for women and 5.4 million per cubic millimetre of blood for men.
Erythrocyte Lifespan: The average lifespan of human RBC is 120 days.
Origin of RBC: The process of RBC formation of production is called erythropoiesis.
RBCs are formed from precursor blast cells in the bone marrow. In human embryo, RBC is formed in the liver and spleen. After birth, it is formed almost exclusively in the red bone marrow
The red bone marrow of all bones produces RBCs from birth to about 5 years of age. Between 5 to 20 years of age, the long bones gradually lose their ability to produce RBCs.
This is because the red bone marrow is converted to yellow bone marrow after the age of 20.
After 20 years of age, most RBCs are produced primarily in the marrow of the sternum, the ribs, and the pelvis.
These bones contain red bone marrow throughout our life. Vitamin B12 and folic acid are essential for the production of RBCs.
Main Functions Of Blood
Blood performs various functions such as transportation of nutrients, gases, etc., protection against various diseases regulation of body temperature, ionic balance, etc.
These functions are as follows—
Transportation: Blood helps in the transportation of several substances within the body, such as nutrients, gases, hormones, vitamins and wastes.
Transportation of nutrients: It transports nutrients derived from food in the intestine to the cells and other nutrients such as glucose, amino acids, proteins, fatty acids, lactic acid, etc., between organiser:
Transportation of gaseous substances: It transports oxygen from the lungs to different tissues of the body, and carbon dioxide from the tissues to the lungs
Transportation of hormones and vitamins: It also carries hormones from endocrine glands to the cells of their target organiser
Transportation of wastes: It carries metabolic wastes from the body cells to the liver and kidneys for elimination from the body through bile and urine, respectively.
Defensive mechanism: Immunoglobulins or antibodies found in it, protect the body against infection.
Role in blood coagulation: Fibrinogen, prothrombin and other coagulation proteins present in plasma play an important role in the coagulation of blood. Coagulation stops bleeding from injured sites. It is a life-saving mechanism.
Regulation of body temperature: Blood helps to maintain a constant body temperature by distributing heat evenly from metabolically active organs such as the liver and working muscles to the rest of the body.
Regulation of acid-base balance: It contains many ions and proteins that act as a buffer by neutralising any excess acid or alkali, Thus, it helps the body to maintain a constant pH.
Regulation of ionic balance: It helps to maintain the ionic balance of the body. Site of storage: Plasma serves as the site of protein storage.
These proteins are utilised by the body tissues during inadequate protein intake, excessive breakdown of body protein or during fasting.
The platelets store several protein molecules especially those involved in blood coagulation.
Regulation of water balance in the body: Blood transports excess water to the excretory system and maintains the water balance of the body.
Various Disorders Related To Blood
- Oligocythemia or anaemia: A defect in the number of red blood corpuscles or in the amount of haemoglobin is generally termed anaemia or oligocythemia. Anaemia can be of different types such as normocytic anaemia, microcytic anaemia, spherocytic anaemia, pernicious anaemia etc.
- Polycythemia: Polycythemia is defined as an increase in the proportion of blood volume that is occupied by RBCs.
- Leucocytosis: Leukocytosis is defined as the abnormal increase in white blood cell count [greater than 11,000 per mm3 (11 x 109 per L)].
- Leucopenia: A decrease in the number of white blood cells is referred to as leucopenia.
- Leukaemia: It refers to cancer of the blood or bone marrow which results in an abnormal increase in the number of leucocytes.
- Thrombocytosis: It is a disorder characterised by the presence of an excessive number of platelets in the blood.
- Purpura: Purpura may occur when the platelet count of the blood is lower than normal.
- Cyanosis or blue baby syndrome: Cyanosis refers to the bluish-purple appearance of the skin, particularly in the regions of lips, mouth, earlobes and fingernails. This condition occurs due to a higher percentage of deoxyhaemoglobin (>5g/dL) in blood. Cyanosis may be caused due to disorders in the lungs, heart and central nervous system.
- Haemoglobinopathy: It is a genetic disorder. This results in the synthesis of abnormal haemoglobin due to alteration in one of the globin chains.
Blood Groups
- Prior to the 20th century, it was thought that all blood was identical. This notion led to frequently fatal transfusions of animal blood into humans and hazardous transfusions of blood between people.
- The nature of blood varies from person to person. Like other cells of the body, red blood cells carry some marker molecules on their membranes. These are called antigens.
- An antigen is a substance to which the immune system responds and produces antibodies, a type of defence molecule.
- On the RBC membrane, there are millions of antigens which are generally ignored by the immune system.
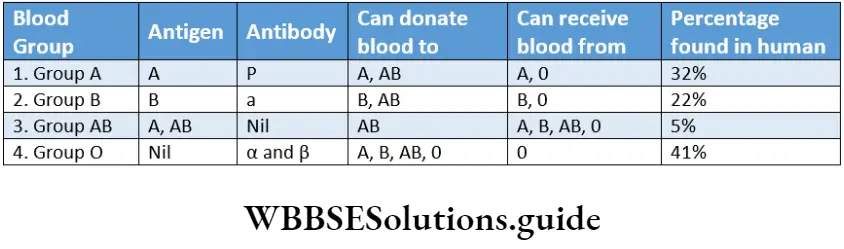
- Antigens are mainly of two types—A and B antigens. On the basis of these antigens, blood has been classified into different groups, called blood groups.
- The antigens are also termed as agglutinogens and antibodies against the antigens are termed as agglutinins.
- There are two types of antibodies present in plasma—anti-A antibody and anti-B antibody. There are several systems by which blood grouping has been done. Two such widely used systems for blood grouping are— the ABO and Rh groupings.
ABO Blood Group System
Definition: The classification of blood into A, B, AB and 0 groups, depending on the presence and absence of A and B types of antigens on RBCs and anti-A and anti-B types of antibodies in the plasma, is known as the ABO blood group system.
The most well-known and medically important blood types are in the ABO blood group.
Discovery: This was discovered in 1900 at the University of Vienna by Karl Landsteiner.
Basis of blood grouping: There are four principal blood types: A, B, AB and O. There are two agglutinogens (A and B) and two agglutinins; anti-A and anti-B (α). Agglutinins are gamma globulin proteins.
All humans and many other primates can be typed for the ABO blood group
Type A individuals have A antigens on the surface of their red blood cells and only 3 antibodies in plasma.
Type B individuals have B antigens on the surface of their red blood cells, and only antibodies in plasma. Type AB individuals have no antibodies but both A and B antigens. Type O individuals have both a and 3 antibodies but no antigens.
Importance of ABO blood grouping: At the time of blood transfusion, blood groups of both the donor and recipient should be known. If unknown blood is given to a person, then there may be a chance of clotting or agglutination. It may even cause the death of the recipient.
Universal blood donor
It is known that antigens present in the donor’s blood react with the antibodies present in the blood of the recipient. In blood group 0, there is no such antigen present in the cell membrane of RBCs.
So, an individual with 0 blood group can donate blood to individuals of other blood groups (A, B, AB, 0). Therefore, people with blood group 0 are known as universal donors.
Universal Blood Recipient
Due to the absence of agglutinin in the blood plasma, individuals with the AB blood group can accept blood from all the other groups (A, B, AB, 0).
So, individuals with AB blood groups are known as universal recipients. According to modern views, this concept of universal donor and acceptor is not accurate.
This is because these concepts are based only on the ABO blood group but the Rh blood group should also be considered.
Rh Blood Group System
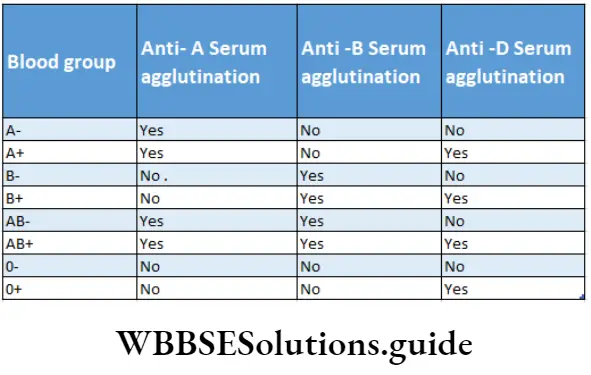
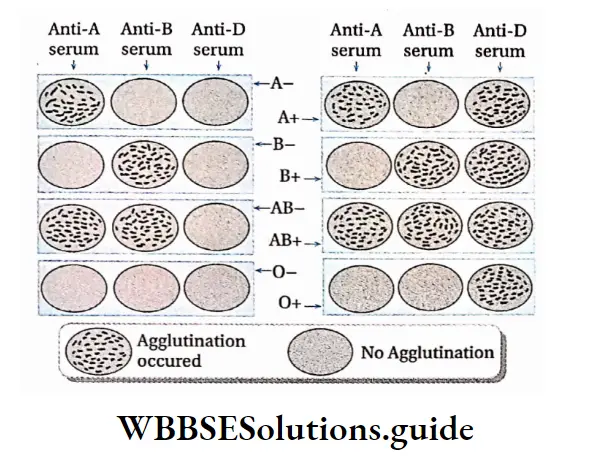
Definition: The classification of human blood depending on the presence and absence of Rh factor on the RBC, into Rh positive (Rh+) and Rh negative (Rh-) groups, is known as the Rh blood group system.
Discovery: Rh blood groups were discovered in 1940 by Karl Landsteiner and Alexander Wiener. They discovered this blood group in the Macaco mulatto (common name: Rhesus Monkey).
Types of Rh antigen: In this blood group system an individual either has or does not have the ‘Rh factor’, (named for the rhesus monkey because it was first studied using the blood of this animal).
This system primarily consists of C, D and E antigens, although it actually contains many more.
The most antigenic component of the Rh blood group system is the D antigen. The antibody in this system is called anti-D-antibody and is produced only when the Rh- Rh-individual receives the D antigen.
Basis of grouping: Those who have D antigen are classified as Rh positive (Rh+) and those who do not have D antigen are Rh negative (Rh-). Based on the presence and absence of Rh factor, each group of the ABO blood group system has two subtypes ‘+’ Hence, an individual with an A+ blood group means he contains blood group A and D antigen (Rh+).
Significance of Rh factor: If blood from an Rh+ individual is donated to Rh- individual, then anti-Rh factor or anti-Rh antibodies will form after 10-12 days. It will cause agglutination of blood and ultimately death of the individual. Hence, it is necessary to test the Rh factor before blood transfusion.
Rh incompatibility during pregnancy
Incompatibility of Rh blood groups between pregnant mother and foetus leads to a condition called erythroblastosis foetalis.
Erythroblastosis foetal:
- If an Rh-woman conceives an Rh+ baby for her first pregnancy, the Rh agglutinogen from the Rh+ blood of the foetus may pass into the maternal circulation.
- In such cases, the mother starts preparing anti-Rh factor against the Rh antigen in her blood.
- This antibody may remain in the mother’s blood for several months even years. Since the total amount of this Rh antigen in the foetus is very small, so total amount of antibodies formed in the mother will be less and may not cause any harm to the first baby.
- The mother becomes sensitive to the Rh factor. In future, if she gets a transfusion of otherwise compatible but Rh+ blood, agglutination will occur.
- During the next pregnancy, the anti-Rh antibodies accumulated in the mother’s blood will pass to the Rh+ foetus via the placenta. This causes haemolysis and various forms of haemolytic disease of the new bom (HDN).
- If the baby survives, the newborn may suffer from life-threatening anaemia and lack of oxygen in the blood.
- The baby may also suffer from jaundice, fever, enlarged liver and spleen. This condition is called erythroblastosis foetalis. If severe haemolysis occurs in the foetus, the infant may die in the uterus.
- It can be avoided by introducing anti-Rh antibodies into the mother’s body after the delivery of the first baby. This will inhibit active antibody formation by the mother against the Rh+ antigen. In this way, this disorder can be controlled in the case of the second baby.
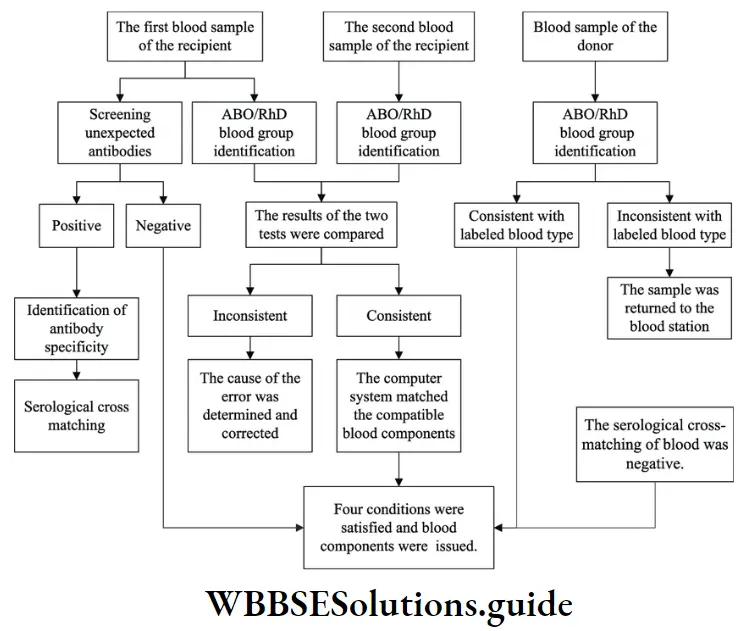
Blood Transfusion
- Blood transfusion is the process of transferring blood or blood-based products from one person (donor) to another (recipient) through a vein, i.e., intravenously.
- Several precautions must be undertaken for the procedure, like, the selection of a proper donor, fresh transfusion substances, proper sterilization of the equipment, determination of amount and rate of transfusion and ability of the recipient to receive.
- Blood transfusion can be used during life-threatening situations, to treat severe diseases, during life-saving surgeries, etc. In past, there was only a transfusion of blood.
- But, in modern medical practice both blood and components of blood, can be used for transfusion. Dangerous haemolytic transfusion reactions occur when blood is transfused into a patient with an incompatible blood type.
Blood Clotting Or Coagulation
Blood Clotting Definition: The process of transformation of blood into a gel-like substance, outside the blood vessels, is known as blood coagulation or clotting.
Normally, within blood the remains of blood vessels are in its liquid If it is form drawn as out long of a s their vessels, it becomes thick and forms a gel. Gradually, the gel separates from the liquid.
The remaining straw-coloured liquid is called serum and the gel-like substance is called a clot.
The clot consists of a network of insoluble protein fibres, called fibrin, in which the formed elements of blood are trapped.
Importance of blood coagulation or clotting
- Blood coagulation helps to avoid haemorrhage and blood loss by the process of haemostasis.
- The chances of infections are very less due to the formation of a clot at the wounded site.
- It regulates the transportation of important substances in the body by maintaining blood pressure during any injury.
Normal Blood Coagulation
In normal conditions, blood coagulates within minutes, at the injured site. The time required for blood coagulation depends on certain factors such as the number of platelets, and concentration of coagulation proteins, such as thrombin and fibrinogen. in the blood plasma, etc.
Blood coagulation time is calculated during the detection of the disease and before surgery. There are two time periods related to bleeding and blood clotting— bleeding time and coagulation time.
Bleeding time (BT) and coagulation time (CT) Bleeding time is the time taken for bleeding to stop from the site of injury.
It measures the time between the onset of injury and temporary haemostasis (platelet plug or clot formation).
Duke and Ivy methods are the two methods for calculating bleeding time. Coagulation time is the time taken by blood to coagulate after it has been shed. It depends on many factors involved in the coagulation process.
There are various methods for calculating coagulation time, such as the capillary tube method and the Lee-White method.
Blood Coagulation Factors
Blood coagulation depends on various substances or clotting factors, present in the plasma. 13 blood clotting factors have been identified till now. They are represented by Roman numerals.
They are as follows—
- Fibrinogen (Factor 1),
- Prothrombin (Factor 2),
- Thromboplastin (Factor 3),
- Calcium ions (Factor 4),
- Labile factor or proaccelerin (Factor 5),
- Proconvertin (Factor 7),
- Antihaemophilic factor or AHF (Factor 8),
- Christmas factor (Factor 9),
- Stuart-Prower factor (Factor 10),
- Plasma thromboplastin antecedent (Factor 11),
- Hageman factor (Factor 12),
- Fibrin stabilizing factor (Factor 13)
Factor 6 has been rejected recently, as it is nothing but the active form of factor 5.
Process Of Blood Coagulation
The process Of Congulations Is A very Complex Biochemical Process. Primary And Modern Concepts of Blood Coagulation.
Primary Concept Of Blood Coagulation
The primary concept of blood coagulation is the preliminary or basic concept behind the blood coagulation process.
According to this concept, the process of blood coagulation involves four steps, which are as Follows
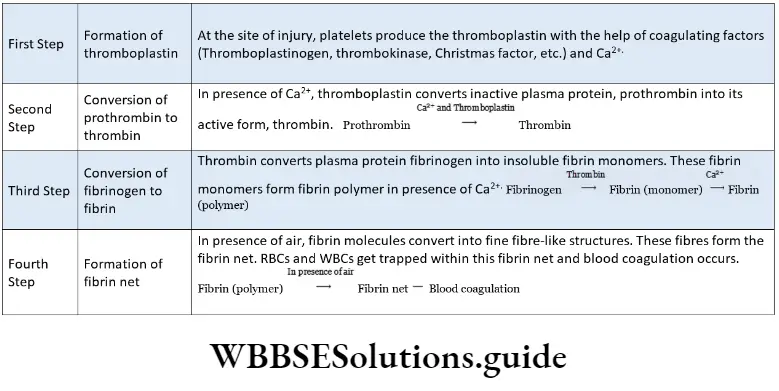
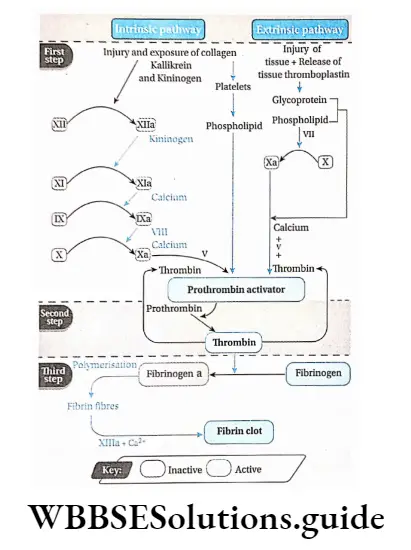
The Modern Concept of Blood Coagulation
In 1965, scientists Davie and Ratnoff named the modern concept of coagulation as the waterfall sequence theory’. This theory is also termed as ‘cascade theory’ by MacFarlane.
Scientists found that the process of blood coagulation includes a sequence of enzyme activity.
Activation of an enzyme or factor occurs in each step of this process. The activated enzyme of one step activates another enzyme or factor in the next step. According to this concept, there are three steps of blood coagulation.
First step: It includes two pathways—
Intrinsic pathway:
- This process begins with trauma to the blood vessels. The initial reaction in this pathway is the conversion of inactive factor 12 to active factor 12 (factor 12a).
- Factor 12a now activates factor XI which in turn activates factor 9 to factor IXa.
- This factor 9a forms a complex with active factor 8.
- The complex of 9a & Villa activates factor 10.
Factor 10a then forms a complex with factor Va, phospholipid and calcium ion, called prothrombin activator (which previously was called thromboplastin).
Extrinsic pathway:
- When there is trauma to the tissues, this pathway is initiated by the release of tissue thromboplastin (TPL), a protein phospholipid mixture that activates factor VII.
- Factor Vila with Ca2+, TPL and phospholipid (PL) together activate factors IX and X.
- Ultimately, activated factor 10 in the presence of PL, calcium ion and factor 5, catalyzes the formation of a prothrombin activator as in the intrinsic pathway.
Second step: Prothrombin activator formed by both the intrinsic and extrinsic pathways, catalyzes the conversion of prothrombin to thrombin in the presence of calcium ions.
Third step: 1 The fundamental reaction in blood clotting is the conversion of soluble plasma protein fibrinogen to insoluble fibrin, catalyzed by thrombin. Thrombin is a serine protease which also activates platelets, factors 5, 8, 9 and 7.
This process involves the release of two pairs of polypeptides from each fibrinogen molecule. The remaining portion, fibrin monomer, then polymerizes with other monomers to form fibrin threads.
Fibrin is initially a loose mesh of interlacing strands which make a dense meshwork. Platelets are entrapped in this meshwork to form blood clots. The latter reaction is termed as stabilization that requires factor 13a and Ca2+.
Fibrinolysis
The normal breakdown of blood clots by the action of enzymes is known as fibrinolysis. It is the first step involved in the repairing of blood vessels. This process occurs through the breakdown of fibrils into soluble substances.
Diseases related to defective blood clotting
Thrombosis or intravascular dotting: The formation of clots inside blood vessels is called thrombosis or intravascular clotting.
Haemophilia: It is a rare, inherited and life-threatening bleeding disorder in which the blood does not clot properly.
It is usually of three types— Haemophilia A or classical haemophilia (due to factor VIII deficiency) and Haemophilia B or Christmas disease (due to factor 9 or plasma thromboplastin component (PTC) deficiency), Haemophilia C (Due to factor 11 deficiency.
Anticoagulants
Anticoagulants (commonly known as ‘blood thinners’) are substances that are used to prevent clot formation or to prevent a clot from enlarging, by blocking the action of clotting factors or platelets. E.g., heparin, plasminogen (natural anticoagulants) sodium citrate, sodium or potassium oxalate (artificial anticoagulants).
Anticoagulants Used In Blood Banks
Generally, sodium citrate is used as an anticoagulant in blood banks. Sodium citrate removes calcium from the blood by forming calcium citrate. Blood does not coagulate in the absence of Ca2+ Hence, blood coagulation does not occur.
Serum
Serum Definition: The clear yellowish fluid obtained upon removing the clot after the whole blood has been allowed to clot, is called serum.
Blood Vessels
Blood Vessels Definition: The tube-like structures involved in the circulatory system, through which blood flows to the tissues from the heart and returns from the tissues to the heart are known as blood vessels.
Types Of Blood Vessels
There are mainly three types of blood vessels—arteries, veins and capillaries. The structure of each type is closely related to its function.
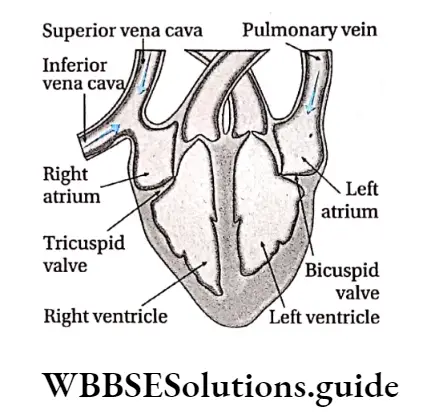
As the heart contracts, it forces blood into the large arteries from the ventricles.
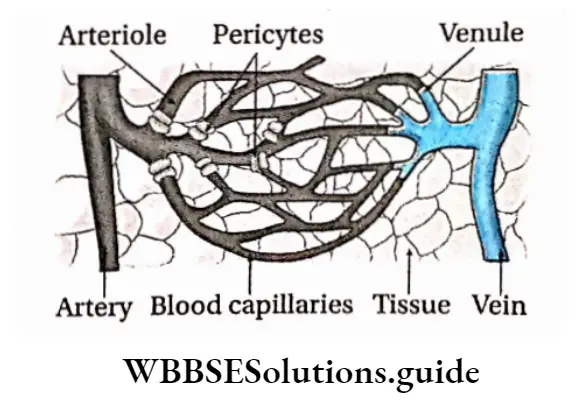
The blood drains into successively smaller arteries and finally, the blood reaches the smaller branches, the arterioles (little arteries). These arterioles feed the capillary beds of tissues and body organiser
Blood drains from the capillaries into venules (the smallest veins), and then into larger veins that merge to form the large veins. Finally, these veins empty into the heart.
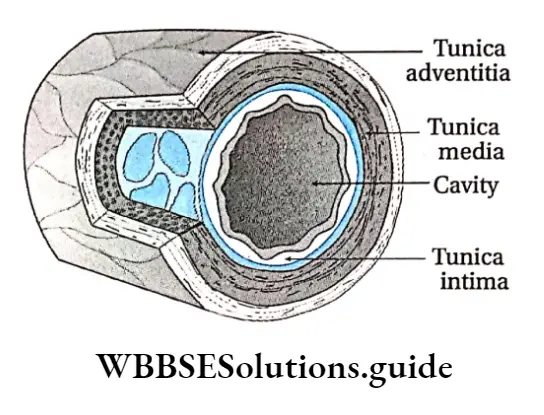
Arteries: The blood vessels that carry oxygen-rich blood away from the heart towards other organs of the body, are called arteries.
Cellular structure: The layers of the artery are—
Tunica adventitia: This layer is the outermost layer of the artery. It is formed of fibrous connective tissue. Some amount of elastic fibres are also found in this layer of arteries.
It is comparatively thinner than the external layer of the vein. Sometimes blood vessels are also found in this layer of some arteries, known as vasa vasorum.
Tunica media: This is the middle layer of the artery composed of elastin. This layer has a uniform diameter. It is comparatively thicker than that of veins and contains more elastic fibres.
Tunica intima: It is very thin and is made of a single layer of endothelial cells. This layer is also known as endothelium. It surrounds the inner cavity of the artery.
Veins: The veins are the blood vessels that carry blood from different tissues of the body towards the heart.
Cellular structure: The layers of a vein are—
Tunica adventitia: This layer is very thick and contains a very low amount of elastic tissues. Vasa vasorum is absent here.
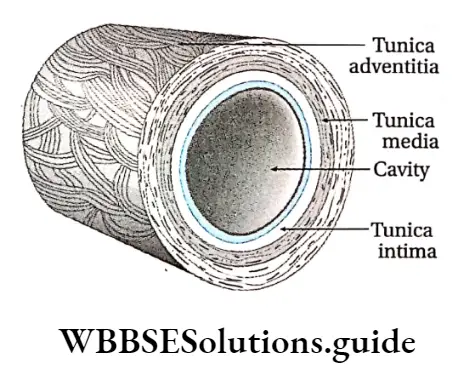
Tunica media: It is the middle layer and comparatively thinner than the outermost layer. It lacks elastic fibres and membranes.
Tunica intima: It is the innermost layer lining the lumen of veins. The inner lining of this layer contains valves. These valves prevent the backflow of blood from veins to capillaries. So, blood flows towards the heart from the capillaries in the tissues through the veins.
Systemic veins
Veins which originate from a set of capillaries and directly reach the heart without passing through any other set of capillaries are called systemic veins.
Example: The pulmonary vein arises from capillaries present in the lungs and directly transports the oxygenated blood to the left atrium of the heart.
Portal veins
Veins originate from a set of capillaries and divide into another set of capillaries into some organs, before reaching the heart.
Example: Hepatic portal veins in human beings originate from the capillaries present in the small intestine and spread into the liver where they redivide into capillaries.
Vasa vasorum
- Some tiny, fine vessels found in the walls of large arteries and veins, are known as vasa vasorum (vessel of the vessel).
- In the case of larger vessels, the layers are too thick to be nourished solely by diffusion from the blood in the lumen.
- These small, fine vessels provide metabolites by means of diffusion from the blood that circulates in the lumen of the vessels to the adventitia and the media of the large vessels.
- These are not present in the inner layer or tunica intima. Vasa vasorum is more frequent in veins than in arteries.
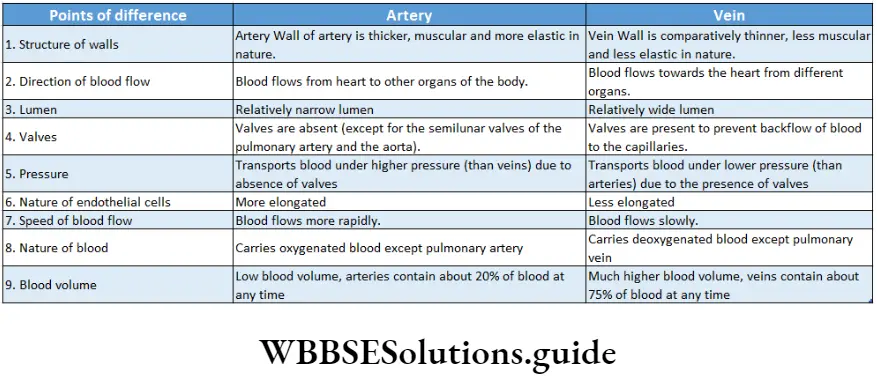
Blood capillaries: These are the smallest blood vessels that connect arterioles and venules.
Cellular structure: Blood passes from the arterioles into the capillaries. They are 4- 10 pm in diameter. The capillary wall does not contain tunica media or tunica adventitia.
Their walls, consisting only of endothelial cells, are permeable to water and dissolved substances.
These endothelial cells are lined externally by a basal lamina and wrapped around by branching perivascular cells called pericytes.
The entrance to each capillary is guarded by a band of smooth muscle called a precapillary sphincter. Blood flows slowly through capillaries (less than 1 mm per second).
Capillaries are the only blood vessels whose walls permit exchange between the blood and the surrounding interstitial fluids. This is because they have thin walls and diffusion distances are also less which facilitates rapid exchange.
In addition, blood flows through capillaries relatively slowly, allowing sufficient time for the diffusion or active transport of materials across the capillary walls.
Functions of blood vessels
The respective functions of arteries, veins and capillaries are discussed under separate heads.
Functions of arteries:
- Arteries transport oxygenated blood away from the heart (except the pulmonary artery).
- Arteries transport blood to capillaries.
- Arterioles, tiny branches of arteries, are the pulmonary main regulators of artery transports of blood deoxygenated low and pressure blood from the right ventricle to the Capillaries of the lungs.
Functions of veins:
- Veins transport deoxygenated blood towards the heart (except the pulmonary vein).
- Venules, the minute vessels, drain blood into veins from capillaries.
- The pulmonary vein transports oxygenated blood from the capillaries of the lungs to the heart.
Functions of capillaries:
- They supply blood to all the tissues of the body and also remove wastes from the surrounding cells.
- They mediate the exchange of oxygen, water, carbon dioxide, salts, etc., between the blood and the surrounding tissues.
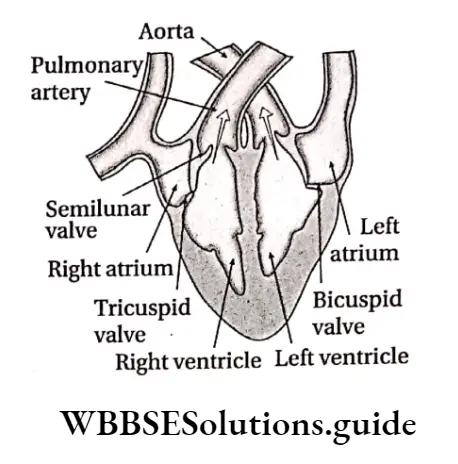
Cardiac Cycle
Definition: The cardiac cycle refers to the sequence of events which takes place during the completion of one heartbeat.
It involves alternate contraction (systole) and relaxation (diastole) of the heart muscles.
The time required to complete one cardiac cycle is known as the duration of cardiac cycle. If the normal heart rate of a person is 75 beats/min, then the duration of the cardiac cycle for that person is 60/75=0.8 seconds. Under normal conditions, this duration is about 0.8 seconds.
Changes Or Events During Each Cardiac Cycle
Changes or events during each cardiac cycle are divided into four parts—
- Atrial systole,
- Atrial diastole,
- Ventricular systole,
- Ventricular diastole
Atrial systole (Duration is 0.1 second)
In this phase, the atria begin to contract. The SA node gets stimulated with the filling of blood in the atria.
As a result, it sends impulses to the walls of both the atria. As the SA node is present in the wall of the right atrium and the left atrium is situated away from the SA node, it is believed that the left atrium contracts after the contraction of the right atrium.
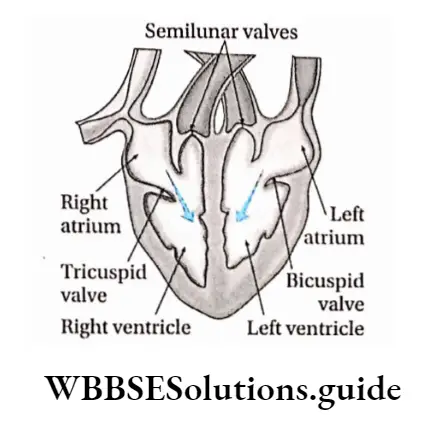
Blood pressure within the atrial chambers increases, which forces the blood to flow across the open AV (i.e., bicuspid and tricuspid) valves, leading to a rapid flow of blood into the ventricles.
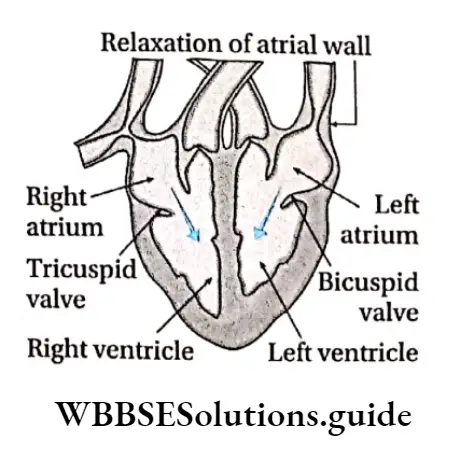
Atrial diastole (Duration is 0.7 second)
After the atrial systole, occurs atrial diastole. During this time, the atrial muscles relax. Gradual filling of the right atrium occurs due to continuous venous return.
The filling of the left atrium also occurs as it receives oxygenated blood from pulmonary veins. In this period, both the atria begin to expand and the AV valves remain closed.
Ventricular systole (Duration is 0.3 seconds)
When the ventricles are filled up during atrial systole, the pulse generated by the SA node gets transmitted to the AV node.
From the AV node, the impulse is transmitted to all parts of both the ventricles through AV bundles and bundle branches. Receiving the stimulus, the two ventricles undergo simultaneous contraction or systole.
This event is divided into two parts —
Isovolumetric contraction (Duration is 0.05 second): Semilunar valves do not open immediately after the closure of AV valves.
It takes 0.05 seconds to open. In this stage, both the AV valves and semilunar valves remain closed.
As a result, ventricles become blood-filled closed chambers and blood pressure increases inside the ventricles. Ventricular volume does not change because all valves are closed during this phase.
This type of contraction is, therefore, said to be “isovolumic” or “isovolumetric”.
Ventricular ejection (Duration is 0.25 seconds): After the isovolumetric contraction, semilunar valves open and the ejection phase begins.
Ventricular ejection is divided into two phases—
Rapid ejection phase (0.11 second): This phase represents the initial and rapid ejection of blood into the aorta and pulmonary arteries from the left and right ventricles respectively. Ejection begins when the intraventricular pressure exceeds the pressures within the aorta and pulmonary artery. This causes the aortic and pulmonary valves to open.
Reduced ejection phase (0.14 second): At the end of the ejection phase, the rate of flow of blood from the ventricles to the aorta and pulmonary artery reduces. This happens due to a reduced amount of blood in the ventricles.
Ventricular diastole (Duration is 0.5 seconds): Ventricular diastole occurs after the contraction of the ventricles. During this phase, the ventricles receive blood from the respective atria.
This phase is divided into three events—
Protodiastole or protodiastolic period: When the ventricular systole ends, the ventricles start relaxing and intraventricular pressure falls rapidly. It lasts for 0.04 seconds.
During this phase, the elevated pressure in the distended arteries (aorta and pulmonary artery) immediately starts to push back the blood towards the ventricles which causes the semilunar valves to close.
Isovolumetric relaxation: The period between the closure of the semilunar valves and the opening of the AV valves is termed isovolumetric relaxation.
It lasts for 0.08 seconds. A precipitous fall in ventricular pressure without a change in ventricular volume occurs here.
Filling phase: After the opening of AV valves, blood enters the respective ventricles from the atria. This is known as the filling phase and it lasts for 0.38 seconds.
This phase is divided into three parts—
First rapid filling phase: As the ventricles continue to relax at the end of isovolumetric relaxation, the intraventricular pressures will at some point fall below their respective atrial pressures. When this occurs, the AV valves rapidly open and ventricular filling begins. It lasts for 0.113 seconds.
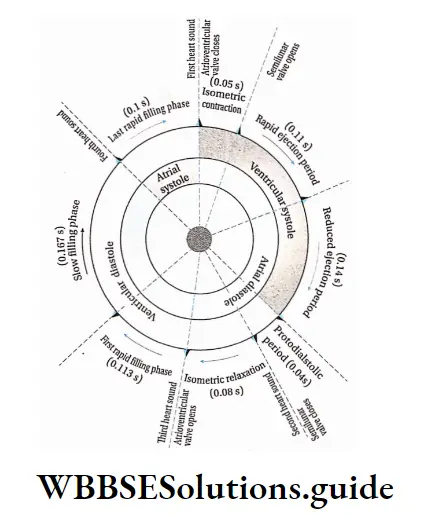
Slow filling phase or diastasis: In this stage, the rate of filling of ventricles slows down as a large amount of blood moves to the ventricles in the rapid filling phase. It lasts for 0.167 seconds.
Last rapid filling phase: As the ventricles continue to fill with blood and expand, they become less compliant and the intraventricular pressures rise.
This reduces the pressure gradient across the AV valves so that the rate of filling falls. Aortic pressure and pulmonary arterial pressure continue to fall during this period. This phase lasts for 0.1 seconds
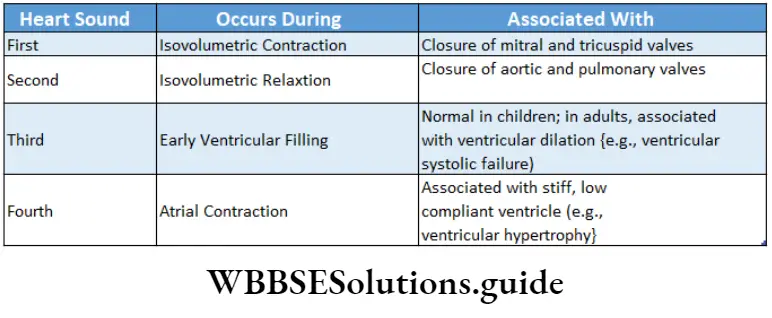
Heart Sounds
Heart Sounds Definition: The sounds occurring during the cardiac cycle are known as heart sounds.
Heart Sounds Types: There are four basic heart sounds that can be heard. These sounds are normally heard with the help of a stethoscope placed on the chest.
The first heart sound (LUBB or LUB) is prolonged. It is caused by the vibrations caused by the closure of the mitral and tricuspid valves at the beginning of isovolumetric ventricular contraction.
It can be heard most clearly by placing the stethoscope over the apex of the heart.
Its duration is 0.10-0.17 seconds. The second heart sound (DUPP or DUP) is short and sharp.
It arises due to the vibrations caused by the closure of the aortic and pulmonary valves just after the end of ventricular systole.
The second heart sound is physiologically split because aortic valve closure normally precedes pulmonary valve closure.
This splitting is not of fixed duration and may range from 30 to 60 milliseconds. It lasts for 0.10-0.12 seconds.
The third heart sound is a low-pitched, soft sound which occurs early in ventricular filling.
It may be generated due to nervous tension in the chordae tendineae and the atrioventricular ring, which is the connective tissue supporting the AV valve leaflets.
It lasts for 0.04 seconds. The fourth heart sound is sharp and short, caused by vibration of the ventricular wall during atrial contraction.
It is usually associated with a stiffened ventricle and is heard in patients with ventricular hypertrophy, myocardial ischemia, or in elderly people. It lasts for 0.1 seconds.
Coronary Artery Disease (CAD)
Other names given to this disease are—ischemic heart disease and atherosclerosis plaque.
Cause: Intake of excessive high-fat foods, sedentary lifestyle, obesity, etc., can cause this disease.
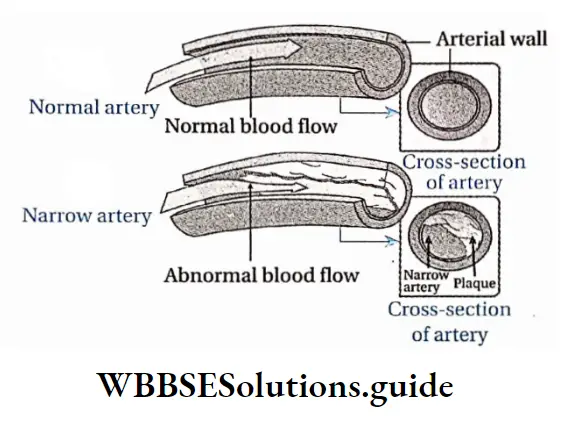
Symptoms: Individuals with coronary artery disease have suffered from myocardial infarctions (commonly known as a heart attack), coronary ischemia and flash pulmonary oedema.
Types: These are as follows—
Angina pectoris: Angina Pectoris is the feeling Of Sudden Pain Or Discomfort in the Chest due To Low oxygen supply in the heart muscles. Details about this is
discussed in the next topic.
Cause: Intake of excessive high-fat foods, sedentary lifestyle, obesity, etc., can cause this disease to oxygen supply in the heart muscles.
Ml or myocardial infarction: Myocardial infarction (Ml), is commonly known as a heart attack. It occurs when blood flow is hampered to the heart muscles due
to blockage of the coronary artery.
Cause: The common cause of an Ml is a blood clot (thrombosis) that forms inside the coronary artery or one of its branches and blocks the blood flow to the
heart muscles.
Symptoms: The main symptom is severe chest pain. The pain may also travel up to the jaw, and down the left arm, or both arms. A person may also sweat excessively, feel sick and even faint.
The pain may be similar to angina, but it is usually more severe and lasts longer. Angina usually goes off after a few minutes. Ml pain usually lasts for more than 15 minutes, sometimes several hours.
Prevention and treatment: The therapy in Ml includes the restoration of normal coronary blood flow and the maximum recovery of functional myocardium.
These goals can be met by a number of medical interventions and adjunctive therapies.
The primary obstacles to achieving these goals are the patient’s failure to recognize Ml symptoms quickly and the delay in seeking. medical attention.
Treatment options for CAD include the use of antiplatelet drugs, aspirin, nitroglycerine, pain relief drugs, beta blockers and use of heparin, and angioplasty.
Angina pectoris
Angina pectoris is chest pain or discomfort, caused by an imbalance between myocardial blood supply and oxygen demand.
Cause: Angina pectoris usually occurs during exertion, severe emotional stress or after a heavy meal, when the heart muscle demands more oxygen than the narrowed coronary arteries can deliver.
Symptoms: Angina is usually felt as—
A squeezing pressure, heaviness, burning across the chest. This pain often spreads to the neck, jaw, arms, shoulders, throat and back.
Patients may also experience indigestion, sweating, nausea, cramping, and shortness of breath. Angina typically lasts from 1 to 15 minutes.
Prevention and treatment:
This can be prevented by avoiding intake of high-fat food, smoking and consumption of alcohol. Regular exercise may also Angina pectoris; Angina pectoris is the feeling of reducing the risk of this disease.
This can be treated by sudden pain or discomfort in the chest due to low j angioplasty.
Heart Failure
It is a serious condition caused by the inability of the heart to maintain the circulation of blood around the body.
Cause: Heart failure does not often have a single cause.
There are a number of factors including hypertension, atherosclerosis, heart muscle weakness (cardiomyopathy) and congenital conditions that may increase the chances of heart failure.
Symptoms:
Heart failure is typically a chronic, or ongoing condition that develops slowly over time. Some people with heart failure experience fatigue and difficulty in completing daily activities.
Others may notice swelling (also called oedema) in the legs, feet, and abdomen. This congestion (heart failure) occurs because blood flows slowly from the heart, and therefore, blood returning to the heart accumulates there. As a result, fluid builds up in the tissues of the body, usually first noticed in the feet and legs.
Other symptoms include rapid pulse, cough, loss of appetite, increase in the size of the abdomen, and frequent urination. Less common symptoms include nausea, vomiting and alertness.
Types: There are two main types of heart failure—chronic heart failure and acute heart failure.
Chronic heart failure: Chronic heart failure is a more common form. Symptoms appear slowly over time and worsen gradually in chronic heart failure.
Acute heart failure: Acute heart failure develops suddenly and symptoms are initially severe. It is mainly caused by lack of blood circulation in the myocardium, sudden arrest of pulmonary circulation, acute cardiac arrhythmia (irregular, too fast or too slow heartbeat), etc.
Compensatory Mechanism In Heart Failure
The body utilizes the following mechanisms to compensate for heart failure.
Ventricular hypertrophy (enlargement of the muscular walls of the ventricles) is an important compensatory mechanism in heart failure.
Initially, the thickened heart muscles can contract more forcefully. However, the thickened heart walls eventually become stiff, causing or worsening diastolic dysfunction.
During heart failure, the body’s first response is to release epinephrine (adrenaline) and norepinephrine (noradrenaline).
These hormones cause the heart to pump faster and more forcefully, thereby increasing cardiac output.
This mechanism initially helps to compensate for the heart’s impaired pumping ability.
In people with chronic heart failure, this sustained response increases demands on an already damaged heart. Over time, the increased demands lead to further deterioration of heart function.
Reduced blood flow is another important compensatory mechanism in heart failure.
This is to increase salt and water retention by the kidneys, which increases the blood volume and helps to maintain blood pressure.
However, heart muscle stretches more due to large blood volume enlarging the heart chambers, particularly the ventricles.
At first, the more the heart muscle is stretched, the more forcefully it contracts, which improves heart function.
But, after a certain amount of stretching, this no longer helps but instead weakens the heart’s contractions. Consequently, heart failure worsens.
Prevention and treatment: It can be prevented by changing lifestyle (no smoking, control of high blood pressure and diabetes, more physical activity, healthy food habits, management of daily stress, optimum daily salt intake, etc.) and taking appropriate medicines. Heart failure patients need multiple medications. Each medicine treats a symptom or contributing factor.
Body Fluids And Circulation Notes
- Cytokines: A group of proteins made by the immune system that act as chemical messengers. Some examples are interleukin, interferon, growth factors, etc.
- Depolarisation: The loss of the difference in charge between the inside and outside of the plasma membrane of a muscle or nerve cell due to a change in permeability and migration of sodium ions to the interior of the cell.
- Immune system: The system in human beings which protects them from different diseases and pathogenic organisms. By the production of antibodies or other cellular proteins, this system protects us.
- Immunosuppression: The partial or complete suppression of the immune response of an individual. It is induced to help the survival of a transplanted organ such as bone marrow, transplanted in a cancer patient.
- Macrophages: The large specialised cells that recognise, engulf and destroy target cells. They take part in the immunological responses of the body.
- Mast cells: The cells filled with basophilic granules, release histamine and other substances during inflammatory and allergic reactions.
- Neutral stain: A salt formed by the interaction of an acid dye (e.g., eosin) and a basic dye (e.g., methylene blue) used for staining neutrophils.
- Pseudopodia: The temporary protrusions of the surface of an amoeboid cell, used for movement and feeding.
- Red bone marrow: The semisolid, soft neurovascular tissue inside large bones, where blood cells are formed.
Points To Remember
- Blood is a liquid connective tissue, composed of cells which are suspended in a fluid matrix called plasma.
- The blood plasma transports a variety of solutes, including ions, metabolites, proteins, and hormones throughout the body.
- The blood cells include erythrocytes or RBCs, which transport oxygen, leukocytes or WBCs, which provide defence against harmful agents for the body and thrombocytes or platelets, which play an important role in blood clotting or coagulation.
- Erythrocytes contain haemoglobin that takes part in oxygen and carbon dioxide transport.
- Granular leukocytes include neutrophils, eosinophils, and basophils. Agranular leukocytes include monocytes and lymphocytes. All these cells have specialised functions that serve to protect the body from invading pathogens.
- There are four principal blood groups in humans. They are designated as—O, A, B, and AB. This method of grouping of blood is called the ABO system of blood group.
- There are Rh (Rhesus factor-positive and Rh-negative blood groups).
- Individuals with O blood group are categorised as universal donors.
- Individuals with AB blood group are categorised as universal recipients.
- Dangerous hemolytic transfusion reactions take place when blood is transfused into an individual with an incompatible blood type.
- Haemostasis is the process in which haemorrhage caused by vascular injury is arrested.
- Coagulation is a process by which the body prevents blood loss. Coagulation involves the formation of a blood clot (thrombus) that prevents further blood loss from damaged blood vessels tissues or organisers
- A human cardiovascular system or circulatory system consists of a heart that pumps blood through a closed system of blood vessels.
- The cardiovascular system mainly helps in the transportation of nutrients, water, gases, wastes, and chemical signals to and from all the tissues of the body.
- The pulmonary circulation of the cardiovascular system consists of those vessels that carry blood from the heart to the lungs and back to the heart.
- The systemic circulation of the cardiovascular system consists of those blood vessels that carry blood from the heart to all other parts of the body (except the lungs) and back again to the heart.
- The SA (sino-atrial) node is a small mass of specialized muscle tissue just beneath the epicardium. These self-excited fibres initiate impulses that spread to the myocardium and stimulate the muscle fibres to contract.
- The AV (atrioventricular) node is located in the inferior portion of the septum and just beneath the endocardium. This node provides the only normal conduction pathway between the atrial and ventricular syncytia.
- There are two atrioventricular valves (A-V valves). The tricuspid valve is situated between the right atrium and the right ventricle. The bicuspid (mitral) valve is located between the left atrium and left ventricle.
- There are two semilunar valves. The pulmonary semilunar valve is found between the pulmonary artery and the right ventricle. The aortic semilunar valve is found between the aorta and the left ventricle.
- Arteries carry blood away from the heart under high pressure. The smaller and finer branches of an artery are arterioles.
- Capillaries are the smallest blood vessels. They connect the smallest arterioles to the smallest venules.
- Veins are blood vessels that carry blood back to the heart. A venule is a microscopic vessel that continues from the capillaries and merges with other venules to form veins.
- Heart rate (HR) is the number of times the heart beats in one minute, averaging 75 beats per minute (bpm) in adults at rest.
- Stroke volume (SV) is the amount of blood pumped by each ventricle with each heartbeat. The average stroke volume is 70 ml per beat in adults at rest.
- Heart rate is increased by sympathetic nerve activity and epinephrine. Whereas parasympathetic nerve activity decreases heart rate.
- The first heart sound (lubb) occurs during ventricular contraction. At this point, the closing of the tricuspid and bicuspid valves occurs.
- The second heart sound (dup) occurs during ventricular relaxation when the pulmonary and aortic semilunar valves close.
- A normal ECG pattern is composed of a P wave, a QRS complex, and a T wave.
- The pressure which is exerted on the walls of the arteries during the relaxation phase (diastole) of the heart is called diastolic pressure.
- The pressure exerted on the walls of the arteries during the contraction phase (systole) of the heart is called systolic pressure.