Chemical Coordination Introduction
Chemical Coordination
So far you have studied the different organ systems of the human body. Different organs constituting these systems, carry out different functions.
All these functions are in turn controlled and coordinated by two I organ systems. One of them is the nervous system.
The other one about which you shall learn in this chapter is the 1 endocrine system.
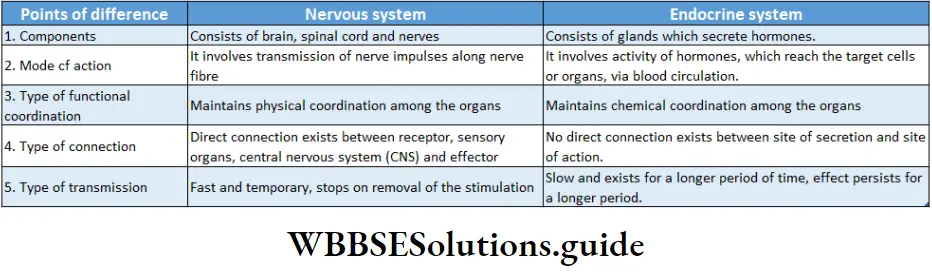
The two systems mentioned above, though similar, show some differences as well. Differences between these two systems (on the basis of their process of coordination) have been discussed below.
All organisms have the ability to coordinate their activities with constant changes in the environment. In doing so, organisms use a number of pathways that receive and process different signals.
Read and Learn More: WBCHSE Notes for Class 11 Biology
These signals originate from cells within the organism, as well as from the external environment.
This maintains a balance between the various metabolic activities of the body, This is the functional coordination of the body which is necessary for maintaining homeostasis within the body, The Endocrine system involves different glands that contain several specialized cells.
Chemical coordination and integration notes for NEET PDF
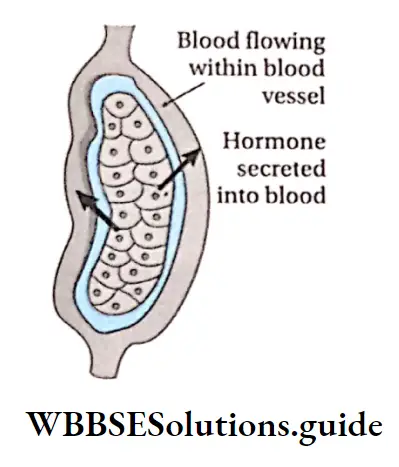
These cells synthesize and secrete some specific biochemical substances, called hormones. Hormones are released directly into the bloodstream by these glands. They act as chemical messengers in the body and flow with the blood to reach the target organs, upon which they act.
Endocrine System
Endocrine Glands
The ductless gland that secretes specific chemical substances and releases them directly into the blood or lymph is called an endocrine gland
The characteristics of endocrine glands are—
- These glands are mostly present in humans and higher groups of vertebrates. They do not contain ducts, hence called ‘ductless’.
- They synthesize and secrete hormones.
- As their secretions are carried by the blood and lymph, these glands are surrounded by a network of blood capillaries.
Examples: Pituitary gland, thyroid gland, etc.
- The glands which release their secretions within or outside the body through ducts are called exocrine glands.
- The products of these glands are of different types, e.g., enzymes, saliva, mucus, bile, sweat, sebum, milk, etc.
Examples: Salivary glands, mammary glands, sweat glands, sebaceous glands, etc.
Mixocrine Or Heterocrine Or Mixed Glands
The glands which are both exocrine and endocrine in nature are called merocrine glands.
These glands contain both exocrine and endocrine cells. Examples: Pancreas, testes, ovary, etc.

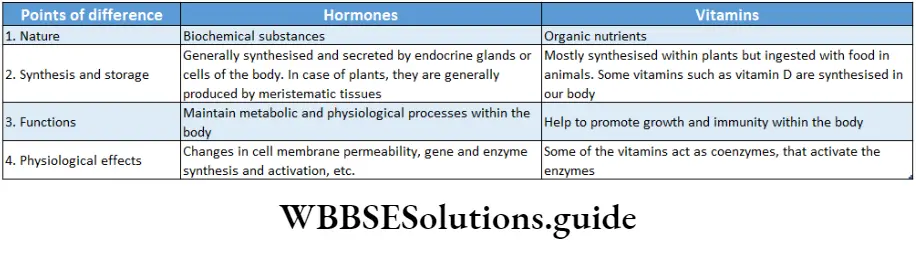
Hormones
Hormones Definition: The biochemical substances synthesized and secreted by endocrine glands or specialized cells, are called hormones.
In 1902, M. Bayliss and Ernest H. Starling isolated a specific substance from the mucous cells of the duodenum.
This specific substance was actually a secretin hormone that stimulates the secretion of pancreatic juice.
In 1905, Starling named this specific substance a hormone. The term ‘hormone’ has been derived from a Greek word, ‘harakiri, which means ‘to excite or to set in motion’.
Hormones Characteristics: Important characteristics of hormones are as follows—
Nature: Biochemically hormones are protein or polypeptide, lipoprotein, glycoprotein, steroid, etc.
Site of secretion: They are mainly synthesized and secreted by endocrine glands. But organs that contain endocrine cells, like testes, ovaries, etc., can also produce hormones.
Storage: They can be stored only in the cells they are secreted from.
| Class 11 Biology | Class 11 Chemistry |
| Class 11 Chemistry | Class 11 Physics |
| Class 11 Biology MCQs | Class 11 Physics MCQs |
| Class 11 Biology | Class 11 Physics Notes |
Effect on target organs: Hormones often exert their influence on target organs or tissues, located at some distance from the gland. However, certain hormones like secretin, gastrin, etc., act only in the adjacent regions of its secretion. So, they are also known as local hormones.
Class 11 biology chemical coordination and integration notes with diagrams
Transportation: They are carried to the target organs by blood or lymph.
Chemical messenger: They do not initiate new functions, but only regulate already occurring cellular processes. They carry chemical messages to target organs. Hence, hormones are also called chemical messengers.
Chemical coordinators: They respond to immediate physiological requirements of the body.
They are involved in maintaining the functional coordination of the organs. Hence, the hormones are also known as chemical coordinators.
Quantity: They are very specific and influence unique cellular responses at very low concentrations.
Feedback mechanism: Hormones may trigger a cascade of amplifying mechanisms. A small amount of a hormone induces the release of a larger amount of another hormone and/or intracellular metabolites In the target cells. This mechanism is called the feedback mechanism.
Fate of hormone: Hormones can be degraded in their target cells. It occurs by internalization of the hormone-receptor complex followed by lysosomal degradation of the hormone.
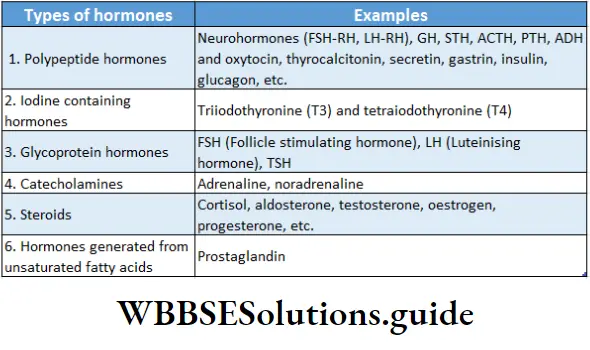
Types of Hormones
The following types of hormones are found in the body—
Harmones Functions
- Hormones affect the functioning of other glands or tissues. Hormones regulate the metabolism of cells, body growth, and development of various parts of the body.
- Hormones are also responsible for the regulation of the immune system and reproductive functions.
- The appearance of secondary sexual characteristics (external characters that distinguish sexes) is also stimulated by hormones.
- In some cases, hormones may cause permanent changes, such as sex differentiation in humans. These changes persist even when the hormone is absent.
- Hormones coordinate the responses to stress. They control blood volume and pressure by regulating the sodium and water balance. This, in turn, maintains the condition of homeostasis.
- To maintain cell membrane integrity and intracellular signaling, hormones regulate calcium and phosphate balance.
Classification Of Hormones
Based on their solubility in water and fat
- Water-soluble: Peptide hormones.
- Fat-soluble: Steroid hormones, hormones secreted by the thyroid gland.
[Based on the types of recptors]
Intracellular receptor: Steroid hormones and thyroxine.
Extracellular receptors: Insulin, glucagon, parathormone, etc.
[Based on their interaction with one another]
- Antagonistic: When a hormone produces the opposite effect of another hormone, it is antagonistic in nature, e.g., insulin and glucagon on blood glucose levels.
- Synergistic: When two or more hormones act together to produce a greater effect, they are called synergistic in nature, e.g., testosterone and FSH on sperm production.
- Permissive: When a hormone enhances the effect of another hormone secreted later, it is called permissive in nature, e.g., estrogen and progesterone in the uterine cycle.
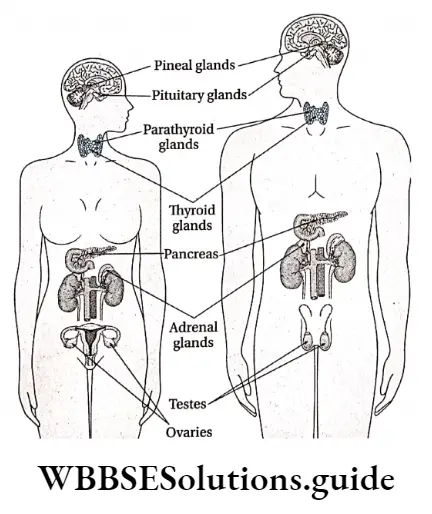
Human Endocrine System
The endocrine system is composed of a variety of different endocrine cells and glands. Endocrine cells or glands include—
The hypothalamus, pituitary glands, pineal gland, thyroid gland, parathyroid gland, adrenal glands, pancreas, reproductive organs (testes and ovary), thymus gland, and placenta.
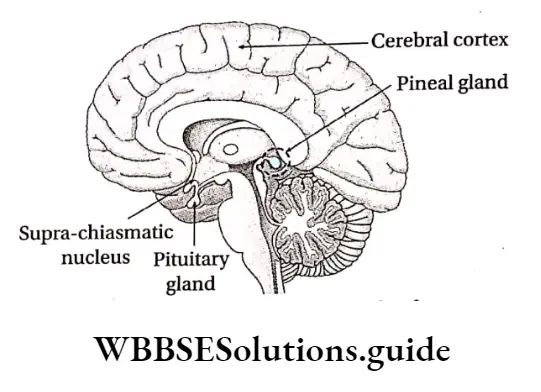
Hypothalamus
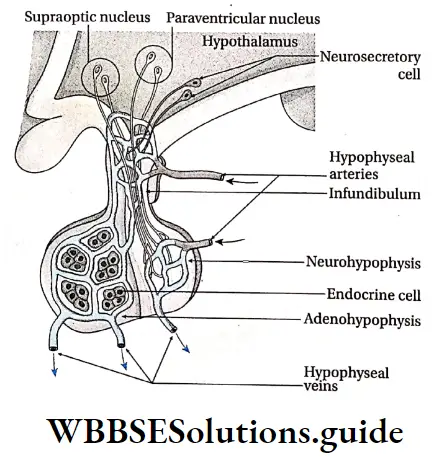
The hypothalamus of the brain contains two sets of neurosecretory cells whose hormonal secretions regulate the activity of the pituitary gland.
Hypothalamus Location: The hypothalamus is located superior to the brain stem and inferior to the thalamus.
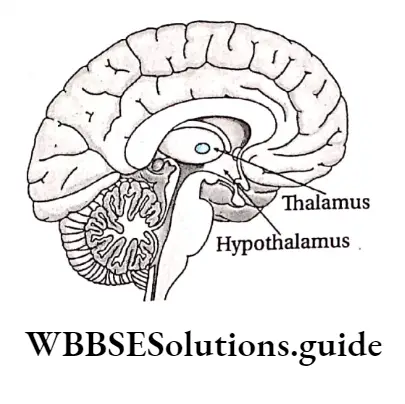
Hypothalamus Structural and functional features: Hypothalamus is composed of nervous tissue.
White matter is present in the center of the hypothalamus, with grey matter in the periphery.
The distribution of the white matter as islands in the grey matter leads to the formation of multiple nuclei. Specialized neuron clusters of the hypothalamus are called neurosecretory cells.
Secretions produced by these cells are called neurohormones. The network of capillaries extending from the hypothalamus joins to form the hypophyseal vein.
It enters the posterior lobe of the pituitary gland and again divides into capillaries. Axons of some of the neurosecretory cells extend into the pars nervosa region of the neurohypophysis.
This path between the hypothalamus and neurohypophysis is called the hypothalamo-hypophyseal tract.
Neurons Of Hypothalamus
Magnocellular neurons are predominantly located in the paraventricular and supraoptic nuclei of the hypothalamus. They produce large quantities of the neurohormones—oxytocin and antidiuretic hormone (ADH).
Parvocellular neurons have projections that terminate in the median eminence, brain stem, and spinal cord.
These neurons are located within the paraventricular nucleus. They release small amounts of neurohormones (hypophysiotropic hormones) that control anterior pituitary function.
Hormones secreted by the hypothalamus: The hormones secreted by the hypothalamus get carried by the blood to the hypophyseal portal vein. They are mainly glycoprotein in nature. The hormones include—
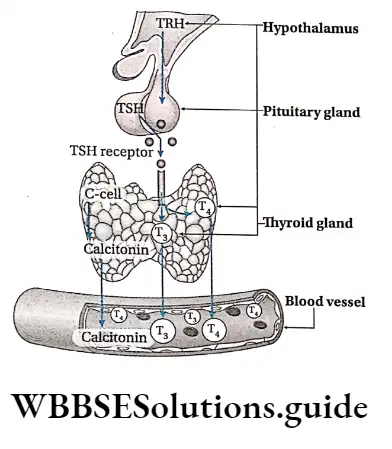
Thyrotropin-releasing hormone (TRH): TRH stimulates the anterior pituitary gland to secrete thyroid-stimulating hormone.
Growth hormone-releasing hormone (CHRH): GHRH stimulates the anterior part of the pituitary gland to secrete growth hormone.
Growth hormone-inhibiting hormone (GHIH): GHIH inhibits growth hormone secretion from the anterior pituitary.
Gonadotropin-releasing hormone (GnRH): GnRH stimulates the anterior pituitary to secrete follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
Short notes on chemical coordination and integration for quick revision
Corticotropin-releasing hormone (CRH): CRH stimulates the anterior pituitary to secrete adrenocorticotropic hormone (ACTH).
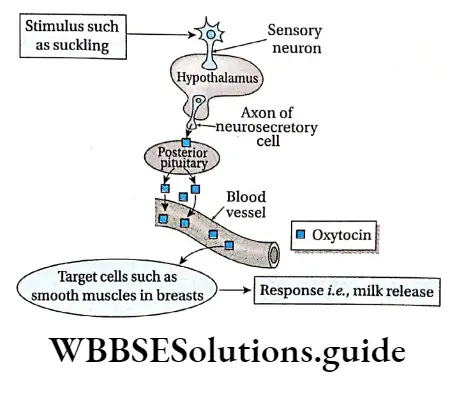
Oxytocin and antidiuretic hormone (ADH): Oxytocin and ADH produced by the hypothalamus are transported to the posterior pituitary where they are stored.
Prolactin-releasing hormone (PRH): PRH stimulates the secretion of prolactin from the anterior pituitary.
Prolactin-inhibiting hormone (PIH): PIH inhibits the secretion of prolactin from the anterior part of the pituitary gland.
MSH-releasing hormone: MSH-RH stimulates the intermediate lobe of the pituitary gland which secretes melanocyte-stimulating hormone.
MSH-inhibiting hormone: MSH-IH inhibits the secretion of melanocyte-stimulating hormone from the intermediate lobe of the pituitary gland.
Pituitary Gland
The Pituitary Gland is also called hypophysis. The name is derived from the Greek words hypo-under and physis-to grow.
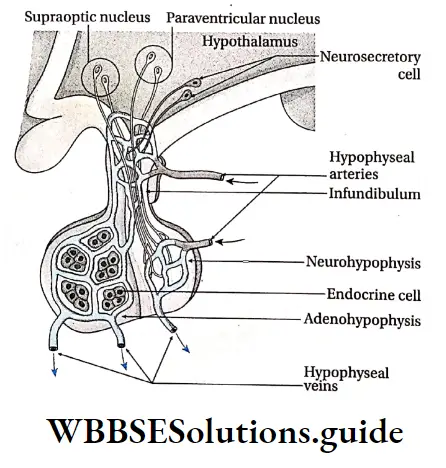
Pituitary Gland Location: It is located in a depression in the sphenoid bone, called sella turcica. It is connected below the hypothalamus by the infundibulum (a stalk-like structure).
Tropic hormones
Hormones that are carried to target organs far off from their secretory cells and affect the secretion of other hormones are called tropic hormones. E.g., FSH, LH.
Tropic hormones Structure: The pituitary gland is small in size. It weighs about 0.5-0.6 g in adult males. It is slightly bigger in the case of adult females. In females, it weighs about 0.6-0.7 g.
The pituitary gland is divided into two regions— the posterior pituitary (neurohypophysis) and the anterior pituitary (adenohypophysis).
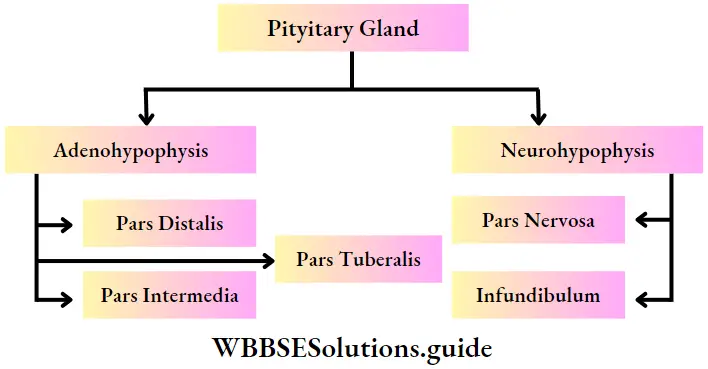
Adenohypophysis (Anterior pituitary)
Adenophysis is the anterior part of the pituitary gland which secretes hormones like GH, TSH, etc.
Parts of the Adenohypophysis: It is divided into three parts—
Parts of the adenohypophysis: It is divided into three parts—
Pars distaiis: It appear as clusters or cords of cells.
Pars tuberalis: It surrounds the infundibulum of the neurohypophysis.
Pars intermedia: In the human fetus it appears as a lobe between the anterior and posterior pituitary but is reduced in adults.
Hormones Secreted by Anterior Pituitary:
The anterior pituitary releases four important hormones that act as tropic hormones.
Following are the types of hormones secreted by the anterior pituitary—
Thyroid-stimulating hormone (TSH)
Source: TSH is synthesized and secreted from basophilic cells, called thyrotrophs, of the pars distaiis region of the anterior pituitary gland.
Chemical nature: TSH is a glycoprotein in nature.
Target organs: As its name suggests, it is a tropic hormone responsible for the stimulation of the thyroid gland. Hence, the thyroid gland is the target organ.
Hormones Physiological functions:
It stimulates the secretion of thyroid hormones such as thyroxine or tetraiodothyronine (T4) and triiodothyronine (T3), from the thyroid gland,
It is an important regulator of metabolic activity in the body,
In addition, it acts as a growth factor for the thyroid gland.
Adrenocorticotropic Hormone (ACTH)
Source: It is produced by the basophilic corticotroph cells of the pars distalis region of the anterior pituitary.
Chemical nature: It is a polypeptide, made up of 39 amino acid residues.
Target organs: It acts upon the cortex region of the adrenal or suprarenal glands located at the top of each kidney.
Hormone Physiological Functions
The release of ACTH stimulates the growth of the cortex region of adrenal glands,
ACTH stimulates the hormone secretion from the adrenal cortex. ACTH stimulates the production and release of glucocorticoids (cortisol), mineralocorticoids (aldosterone), and sex corticoids or sex steroids from the adrenal cortex.
Gonadotropic Hormone (GTH)
Gonadotropic Hormone (GTH) Source: In response to stimulation by gonadotropin-releasing hormone (GnRH), GTHs (both FSH and LH) are synthesized. These hormones are secreted by basophilic cells. FSH and LH are secreted from cells called gonadotrophs. These cells are located at the pars distalis region of the anterior pituitary.
Chemical nature: Both FSH and LH are glycoproteins in nature.
Target organs: FSH and LH have major effects on the human reproductive organs—testes (in males) and ovaries (in females).
Gonadotropic Hormone Physiological functions:
- Both GTHs (FSH and LH) are important for the growth and development of gonads,
- FSH stimulates the growth and maturation of the ovarian follicles. It promotes estrogen synthesis and secretion in adult females
- FSH along with LH stimulates spermatogenesis (sperm production) in males,
- In females, LH is responsible for ovulation (release of a secondary oocyte from the Graafian follicle) and luteinization (formation of corpus luteum). It also regulates estrogen and progesterone hormone levels in adult females,
- LH in adult males stimulates interstitial cells (in the testes) to synthesize and secrete testosterone hormone. In males, LH is termed as interstitial cell-stimulating hormone (ICSH).
Growth hormone (GH) or somatotropic hormone (STH)
Growth Hormone Source: GH is synthesized and secreted from the acidophilic cells, called somatotrophs. These are present in the pars distalis region of the anterior pituitary.
Growth Hormone Chemical nature: GH is a 191 amino acid containing a single-chain peptide hormone.
Growth Hormone Target organs: It is not effective over any specific target organ, rather it affects all the tissues.
Growth Hormone Physiological Functions:
- Human growth hormone (HGH) affects different organs by stimulating their growth and development,
- This hormone plays an important role in the metabolism of carbohydrates, fats, and proteins.
- It also induces cell division in the body. lt also induces calcium retention in the intestine. It also maintains the level of potassium, phosphorus, and calcium in the body.
Prolactin (PRL)
Prolactin (PRL) Source: Prolactin is synthesized and secreted by acidophilic cells, called lactotrophs. These cells are located in the pars distalis region of the anterior pituitary gland.
Prolactin (PRL) Chemical nature: Prolactin is a type of polypeptide.
Prolactin (PRL) Target organs: Alveolar cells of the mammary glands.
Prolactin (PRL) Physiological functions:
- Prolactin stimulates the growth and development of the mammary gland. It also stimulates the synthesis and secretion of milk.
- Prolactin increases glucose and amino acid uptake. It stimulates the synthesis of the milk proteins, 8 casein, and ar-lactalbumin, the milk sugar (lactose), and milk fats from the mammary epithelial cells,
- Prolactin inhibits GnRH release, progesterone biosynthesis, and growth of luteal cells during pregnancy.
Melanocyte-stimulating Hormone (MSH)
Source: MSH is produced mainly in the pars intermedia of the pituitary gland by the proteolytic cleavage of POMC (Pro-opiomelanocortin).
Melanocyte-stimulating Hormone Function:
- Specialized skin cells called melanocytes produce a pigment called melanin. This pigment is responsible for the pigmentation found in the skin, hair and eyes,
- Melanin protects cells from DNA damage which may lead to skin cancer (melanoma).
- Neurohypophysis (Posteriorpituitary) Neurohypophysis is the posterior part of the pituitary gland in which the axons of the neurosecretory cells are present.
Parts of neurohypophysis: Neurohypophysis is divided into pars nervosa and infundibulum.
Pars nervosa: It is composed principally of nerve cell processes, glial cells, and capillaries.
Infundibulum: It is a stalk-like structure that attaches the pituitary gland to the bottom of the hypothalamus.
Hormones secreted by posterior pituitary:
The hormones secreted by the posterior pituitary are as follows—
Oxytocin
Oxytocin Source: The neuropeptide, oxytocin, is secreted by non-myelinated neurons of the paraventricular nucleus of the hypothalamus. It is stored in the pars nervosa region of the neurohypophysis and released in the blood from there.
Oxytocin Chemical nature: It is a peptide hormone, composed of 9 amino acids.
Oxytocin Target organs: Lactating mammary glands and the uterus (during pregnancy).
Oxytocin Physiological Functions:
- Oxytocin stimulates milk ejection by controlling the contraction of the myoepithelial cells (present in glandular epithelium). These myoepithelial cells line the alveoli and ducts in the mammary gland.
- Oxytocin produces rhythmic contractions of uterine smooth muscles during childbirth. It promotes regression of the uterus following the delivery of the baby.
- It induces contractions in internal organs such as the gall bladder, small intestine, urinary bladder, etc.
- It helps in the movement of sperm through the female genital tract.
Antidiuretic hormone (ADH)
Antidiuretic Hormone (ADH) Source: ADH is secreted by the non-myelinated neurons (neurosecretory cells) of the supraoptic nucleus of the hypothalamus. It remains stored within the pars nervosa of the neurohypophysis and is secreted when required.
Antidiuretic Hormone Chemical nature: ADH, also known as arginine vasopressin (AVP), is a peptide containing 9 amino acids.
Antidiuretic Hormone Target organs: Mainly Kidneys.
Antidiuretic Hormone Physiological Functions:
Certain neurons in the hypothalamus are sensitive to the salt-water balance of the blood. When the blood becomes concentrated, these cells send signals to the pituitary gland.
As a result, antidiuretic hormone (ADH) is released from the posterior pituitary. Upon reaching the kidneys, ADH enhances the permeability of the walls of the distal convoluted tubule (DCT) and the collecting duct of a nephron, to water.
This causes excess absorption of water into kidney capillaries from DCT and the collecting duct of the nephron.
As a result, the normal concentration of blood is restored and concentrated urine is produced,
ADH causes constriction of blood vessels, increasing the pressure within them. Hence, it is also known as vasopressin,
ADH helps the smooth muscles to contract and thereby helps in the contraction of the stomach, urinary bladder, etc.
Master Gland
The pituitary gland is known as the master gland. This is because the hormones secreted by the pituitary gland influence the synthesis and secretion of various hormones from other major endocrine glands.
Pineal Gland Or Epiphysis Cerebri
The pineal gland is a small endocrine gland located below the epithalamus of the diencephalon region of the brain.
Pineal Gland Location: The pineal gland or epiphysis is attached to the roof of the third ventricle by its stalk. This gland is located in the diencephalon region of the forebrain in humans.
Pineal Gland Structure: The shape of the pineal gland is like a pine cone. It is about 5-8 mm in length and 3-5 mm in breadth. It is attached to the epithalamus on the roof of the third ventricle of the brain by a short and hollow stalk. It is generally made up of modified nerve cells, called pinealocytes.
The pinealocytes are also called chief cells or parenchymal cells. The pineal gland also contains interstitial cells along with pinealocytes. They are also called glial cells.
Hormones secreted by pineal gland: The hormones of the pineal gland are as follows—
Melatonin
Melatonin Source: Melatonin is secreted by the pineal gland.
Melatonin Chemical nature: Melatonin is an indolamine hormone. It is produced, from the amino acid, tryptophan. Chemically, it is N-acetyl-5- methoxytrypsin.
Melatonin Physiological functions:
- Melatonin regulates circadian and circannual rhythms,
- It also helps to regulate the growth of reproductive organs,
- Its antioxidant properties play a role in immune function and cell proliferation,
- It helps to prevent pigmentation of the skin,
- Melatonin increases the growth and activity of other endocrine glands.
Serotonin
Serotonin Source: Serotonin is synthesized and secreted by the pineal gland.
Serotonin Chemical nature: Serotonin belongs to the tryptamine family. Chemically, it is 5-hydroxytryptamine.
Synthesis of serotonin and melatonin After the synthesis of serotonin, N-acetyl serotonin is formed under the influence of the N-acetylating enzyme.
This N-acetyl serotonin produces melatonin, under the influence of hydroxy indol-O-methyl transferase (HIOMT).
Serotonin Physiological Functions:
- Serotonin acts as a neurotransmitter and helps in the conduction of nerve impulses,
- It also helps in constriction of blood vessels, thereby reducing their diameter.
Thyroid Glands
The thyroid gland is a bilobed endocrine gland that is situated in the upper part of the trachea in the neck region.
Thyroid Glands Location: The thyroid gland is located at the upper part of the trachea, slightly inferior to the thyroid cartilage. It surrounds the larynx.
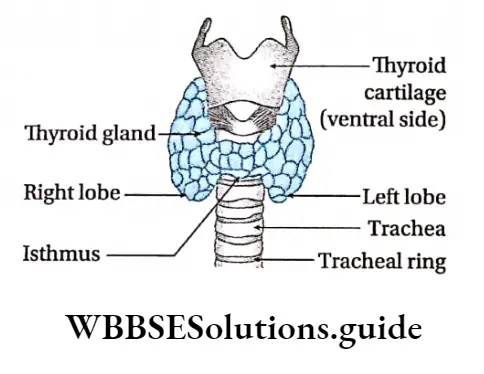
Thyroid Glands Structure: The thyroid gland generally consists of two lateral lobes connected by an isthmus.
This isthmus is present anterior to the 2nd, 3rd, and 4th tracheal rings. Each lobe of the gland extends from the middle of the thyroid cartilage to the 7th or 8th tracheal ring.
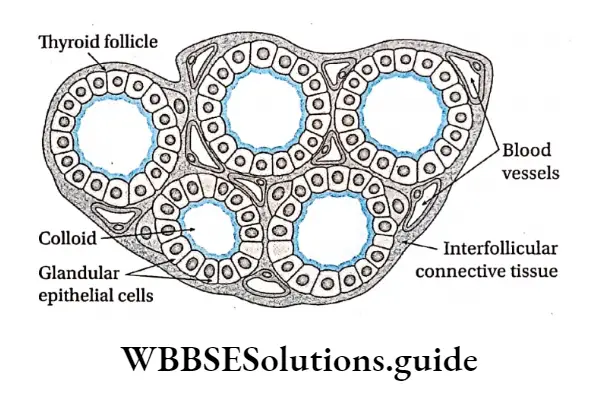
Each of the lobes measures about 5 cm in length, 2 cm in breadth, and 2 cm in height. The thyroid glands generally weigh 20-25g. Thyroid follicles are the structural and functional units of the gland.
Within these follicles, a fibrous connective tissue layer is present, that is rich in blood vessels.
This gland is located near the thyroid cartilage, so it is known as the thyroid gland.
This gland is formed of two types of cells—follicular cells and parafollicular cells.
Follicular cells and parafollicular cells Follicular cells are the principal cells of the thyroid.
They form the continuous epithelial lining of the follicles. Typically, they are cuboidal in shape, with spherical nuclei.
Parafollicular cells or C cells are also associated with the follicles. However, these cells are completely separated from the colloid by follicular cells.
Most parafollicular cells synthesize and secrete the hormone, calcitonin. Therefore, they are frequently referred to as clear cells or C cells.
Hormones secreted by the thyroid gland: The different hormones secreted by the thyroid gland have been discussed below.
Thyroxine or tetraiodothyronine (T4) and triiodothyronine (T3)
Thyroxine Source: The follicular cells of the thyroid gland secrete thyroxine and triiodothyronine.
Thyroxine Chemical nature: Both T3 and T4 are formed by the combination of iodine atoms with the amino acid tyrosine. T4 contains 4 atoms of iodine while T3 contains 3 atoms of iodine.
Role of iodine in T3 & T4 synthesis
Iodine is required to synthesize the thyroid hormones. It is obtained from water, iodized salt, leafy vegetables, fruits, etc.
It is absorbed by the thyroid follicles from the blood. Inside the follicles, the iodine molecules combine with tyrosine (an amino acid), present in thyroglobulin, to synthesize T3 and T4 hormones.
Thyroxine Physiological functions:
- Carbohydrate metabolism by T3 and T4 produces energy. So, they are called calorigenic hormones. They also increase the absorption of 02 into the cells,
- Thyroxine increases basal metabolic rate (BMR) by stimulating different metabolic activities in most tissues,
- Thyroxine stimulates the absorption of glucose in the small intestine. Gluconeogenesis and glycogenolysis are also stimulated by thyroxine,
- Thyroid hormones increase the synthesis of proteins and RNA in the cells.
- T4 and T3 help in the synthesis of cholesterol and other lipids. Thyroxine also increases the concentration of fatty acids by increasing fat mobilization.
- Oxidation of fatty acids in many tissues is also enhanced by thyroid hormone,
- These hormones help in the overall growth of the body,
- Thyroxine affects the heart by causing an increase in heart rate, cardiac contractility, and cardiac output,
- Thyroxine increases milk production and concentration of fats in the milk.
Calcitonin Or Thyrocalcitonin
Calcitonin Or Thyrocalcitonin Source: Calcitonin is secreted by the parafollicular cells of the thyroid gland.
Calcitonin Or Thyrocalcitonin Chemical nature: Calcitonin is a peptide hormone, composed of 32 amino acids.
Calcitonin Physiological functions:
Calcitonin helps in the absorption of calcium into the matrix of bones and thereby, reduces the concentration of calcium ions in the blood.
Calcitonin is known to slow the breakdown of bone by inhibiting osteoclast function. This function is opposite to that of T3 and T4 hormones. Hence, calcitonin is antagonistic to T3 and T4.
Calcitonin also regulates the transport and metabolism of phosphates in the body,
It regulates the concentration of alkaline phosphatase in the blood.
Parathyroid Gland
Parathyroid glands are four, small, oval-shaped, yellowish-brown glands that secrete parathyroid hormone (PTH).
Parathyroid Gland Location: The parathyroid glands are located at the upper and lower portions of the posterior borders of the lateral lobes of the thyroid gland.
Parathyroid Gland Structure: The parathyroid glands consist of four separate glands. Each of these glands is small and oval-shaped. They measure about 6 mm in length, 3 mm in breadth, and 2 mm in height.
Generally, each weighs about 140 mg. These glands are richly supplied with blood capillaries. Parathyroid glands are composed of chief cells and oxyphil cells.
Hormones secreted by parathyroid glands:
PTH or parathyroid hormone is the primary hormone of the parathyroid gland. It is discussed below.
Parathyroid Hormone (PTH)
Parathyroid hormone (PTH) Source: PTH is produced by the chief cells of the parathyroid glands.
J. B. Collip was the first scientist to isolate this hormone. Hence, it is also known as Collip’s hormone.
Parathyroid Hormone Chemical nature: It is a polypeptide, made up of 84 amino acid residues.
Parathyroid Hormone Physiological functions:
- The antagonistic actions of calcitonin and parathyroid hormone maintain the blood calcium level within normal limits,
- PTH indirectly stimulates osteoclasts to reabsorb calcium from the bone matrix, which then enters into the circulation. In addition, PTH also increases renal excretion of phosphate. Due to this, osteoclasts degrade by the process of osteolysis.
- PTH prevents P043-, Na+, and HC03- ion reabsorption in the PCT of a nephron.
- It increases the reabsorption of Ca2+ in the ascending and descending limbs of the loop of Henle.
- PTH stimulates the synthesis of vitamin D or calciferol. It also converts vitamin D into an active hormone. This activated vitamin D helps to absorb calcium in the intestine.
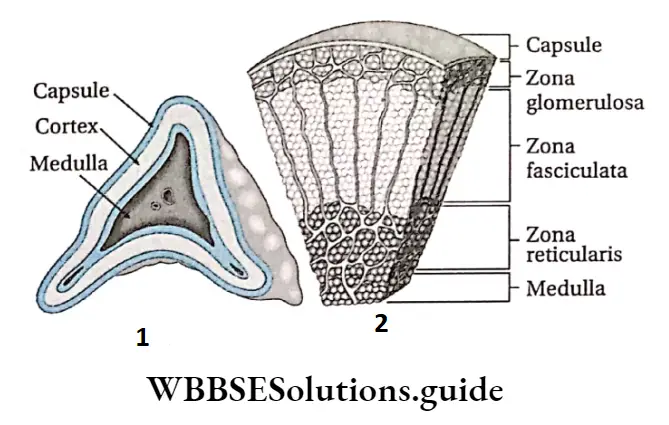
Adrenal Gland
Adrenal Glands are a pair of triangular-shaped endocrine glands. Each gland is present at the apex of each kidney.
Adrenal Gland Location: The right adrenal gland looks like a small pyramid. It is present at the apex of the right kidney and next to the vena cava. The left adrenal gland looks more like a crescent.
It is present at the apex of the left kidney and next to the aorta, colon, stomach, and spleen.
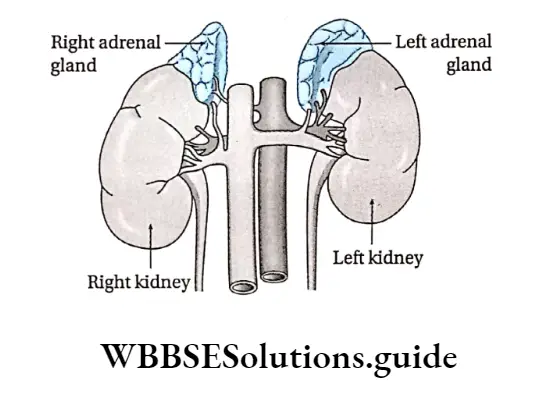
Adrenal Gland Structure: The adrenal glands (or suprarenal glands) are paired glands, each about 4-6 cm in length and 3-4 cm in breadth. The glands are covered by a layer of fibrous connective tissue, called a capsule.
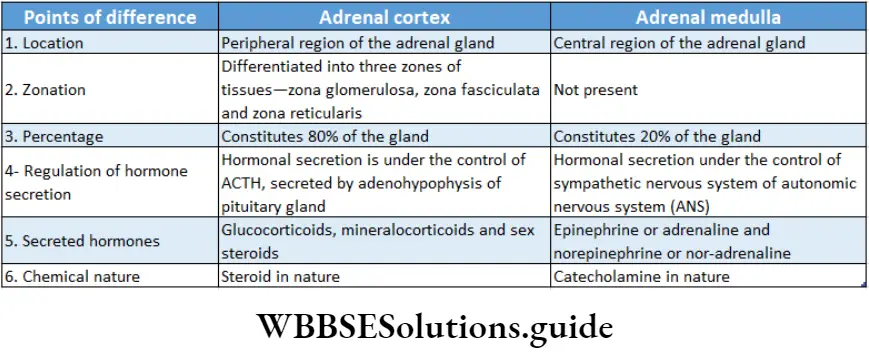
There are several glandular cells within the adrenal glands. Each adrenal gland consists of an inner portion called the adrenal medulla and an outer portion called the adrenal cortex.
However, these portions do not have any physiological connection with one another. The adrenal glands are richly supplied with blood vessels. Different parts of the adrenal glands have been discussed below under separate heads.
Adrenal Cortex
The peripheral region of the adrenal gland constitutes the adrenal cortex.
Adrenal Cortex Structure: It extends between the capsule and the medullary region of the gland. It is richly supplied with blood capillaries, ft consists of glandular epithelial cells.
The cells of the cortex are arranged in three particular zones. They are—Zona glomerulosa, Zona fasciculata, Zona reticularis.
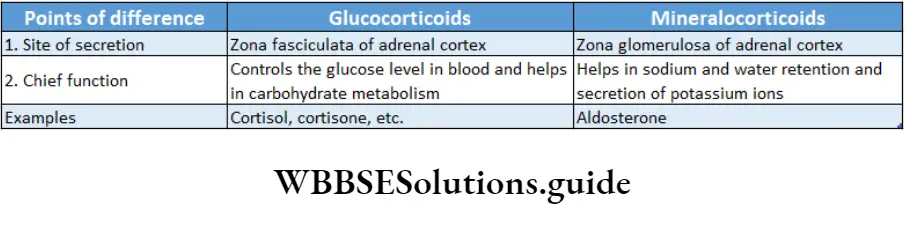
Hormones secreted by the adrenal cortex: Mainly glucocorticoids, mineralocorticoids, and sex steroids are secreted by the adrenal cortex. All these hormones are steroid in nature.
Their physiological functions are described below.
Glucocorticoids
Glucocorticoids Source: Glucocorticoids are secreted by zona fasciculata of the adrenal cortex.
Adrenal Gland Chemical nature: Chemically these are steroid hormones with 21 carbon atoms.
Adrenal Gland Physiological Functions: Cortisol is the main glucocorticoid secreted by the adrenal cortex. Other than this, it secretes cortisone and corticosterone.
We shall study the physiological functions of cortisol, mainly—
Carbohydrate metabolism:
- Cortisol stimulates gluconeogenesis (or neoglucogenesis) in the body. This leads to the production of carbohydrates from non-carbohydrate molecules,
- It promotes glycogenesis in the liver and muscles. This leads to increased synthesis of glycogen,
- It also stimulates the production of enzymes required in gluconeogenesis.
- It increases glucose absorption in the small intestine
Protein metabolism:
- Cortisol stimulates the breakdown of proteins into amino acids,
- It helps the amino acids to be transported to the liver, where they are transformed into glucose,
- The reduced synthesis and enhanced depletion of proteins result in a decrease in stored protein content in cells,
Lipid metabolism:
- Cortisol increases the absorption of lipids in the small intestine,
- It promotes the breakdown of adipose tissues into fatty acids,
- It declines the rate of synthesis of fats from carbohydrates,
- It stimulates the transport of fatty acids to plasma where they are used up as a source of energy,
- This hormone increases the oxidation of fatty acids in cells,
Anti-inflammatory effect:
- Cortisol raises the level of production of anti-inflammatory proteins,
- It also counteracts the inflammatory function of the leucocytes, thereby preventing phagocytosis, chemotaxis (movement of a cell in response to a chemical stimulus), etc.
- It also decreases the secretion of inflammatory chemicals like interleukin 1 (IL-1), prostaglandins, leukotrienes, etc., by injured or infected cells. This prevents heat generation during infections,
- This hormone reduces the production of antibodies, the number of leukocytes, and the amount of lymphoid tissue. All these actions result in immunosuppression of the body.
Mineralocorticoids
Mineralocorticoids Source: The cells of zona glomerulosa secrete mineralocorticoid hormones.
Mineralocorticoids Chemical nature: These are steroid compounds with 21 carbon atoms.
Mineralocorticoids Physiological functions: Aldosterone is the main mineralocorticoid in humans.
Its physiological functions are as follows—
- Aldosterone maintains the concentration of NaCI and water in blood and tissue fluid. It stimulates the absorption of Na+ and cr in kidney tubules,
- Aldosterone increases sodium and water reabsorption in the DCT of nephrons,
- It stimulates the excretion of potassium and phosphate through urine,
- It influences the salt and water balance of the extracellular fluid.
Mineralocorticoids Sex steroids: Sex steroids produced by the adrenal cortex include androgens—dehydroepiandrosterone (DHEA), DHEA sulfate (DHEAS), some amount of estrogen, and progesterone.
These hormones are also known as sex corticoids or gonadocorticoids.
Mineralocorticoids Source: These hormones are produced by zona fasciculata of the adrenal cortex. Zona reticulata also produces androgens.
Mineralocorticoids Chemical nature: These hormones are steroid in nature. The main androgen produced here is DHEA, which is a 19-carbon compound.
Mineralocorticoids Physiological functions:
Androgens control the growth and development of reproductive organs in males. Estrogen and progesterone control the functioning of the female reproductive system,
The sex steroids also regulate the appearance Of male or female secondary sexual characteristics.
Adrenal Medulla
The inner portion of the adrenal gland constitutes the adrenal medulla.
Adrenal Medulla Structure: This region is supplied with blood capillaries and glandular cells. Based on histological staining reaction, adrenal medullary cells are known as chromaffin cells.
These cells are named such because they can be stained with chromium-based dye. These
cells are columnar in shape and contain granular cytoplasm.
Chromaffin cells are of two types—
- E-cells have homogeneous small granules.
- NE cells have larger granules. These granules contain hormones secreted by these cells
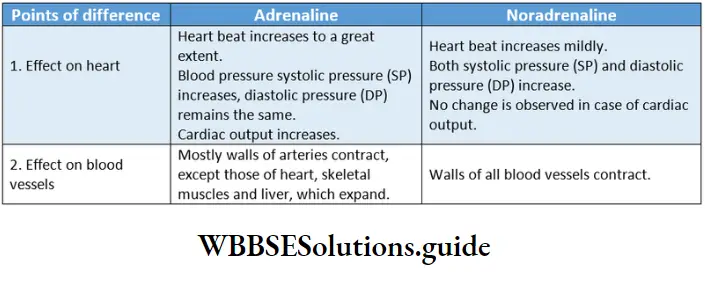
Hormones secreted by adrenal medulla:
The adrenal medulla secretes two catecholamine hormones—epinephrine (E) and norepinephrine (NE). These are also called adrenaline and noradrenaline respectively.
Epinephrine or Adrenaline
Source: The E-type chromaffin cells produce this hormone.
Adrenal Medulla Chemical nature: This hormone is a catecholamine.
Physiological functions:
- This hormone alters the blood flow by constricting some blood vessels while dilating others.
- It decreases the lumen of blood vessels by contracting their smooth muscles. This increases the blood pressure within the blood vessels,
- Adrenaline increases the blood supply to cardiac and skeletal muscles due to dilation of
arterial vessels supplying them, - Adrenaline increases the rate of heartbeat which in turn increases cardiac output,
- It dilates the trachea and thus, increases the rate of respiration,
- It regulates BMR (Basal Metabolic Rate), by inducing glycogenolysis and neo-glucogenesis.
- It plays an important role as a neurotransmitter in the transmission of impulses in the synapse region,
- It dilates the pupil and stimulates the secretion of tears,
- It relaxes the smooth muscles of the stomach, urinary bladder, etc. But in the case of ureters, gall bladder, etc., it contracts the smooth muscles.
Adrenaline As The Emergency Hormone
When the body is under any emergency conditions or emotional stress like anger, fear, etc., secretion of this hormone increases.
Hypersecretion of adrenaline regulates the physiological and metabolic functions according to the state of the body. So, it is also known as an emergency hormone.
Norepinephrine Or Noradrenaline
1. Source: The NE-type chromaffin cells produce this hormone.
Chemical nature: This hormone is also a catecholamine.
Adrenal Medulla Physiological functions:
- This hormone acts as a vasoconstrictor (constricts blood vessels). This results in an increase in blood pressure inside the blood vessels,
- It increases cardiac output. It also acts as a bronchodilator. Hence, it increases respiratory rate,
- It increases blood glucose levels and enhances lipid metabolism to produce fatty acids.
- Norepinephrine also acts as a neurotransmitter. It helps to transmit nerve impulses in the synapse region.
Difference Between Neurotransmitter And Hormone
The difference between a neurotransmitter and a hormone does not lie in the chemical nature of the regulatory molecule.
The difference lies in the way it is transported to its target cells and its distance from the target cells.
A chemical regulator called norepinephrine, for example, is released as a neurotransmitter by sympathetic nerve endings and is also secreted by the adrenal medulla as a hormone.
Pancreas
Pancreas Location: The pancreas is located just below the stomach, adjacent to the spleen. It is connected to the duodenum of the small intestine by the pancreatic duct.
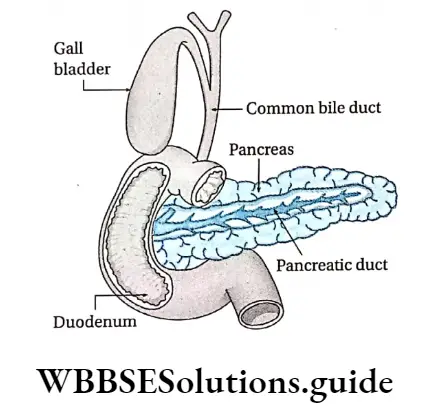
Pancreas Structure: The pancreas has both exocrine and endocrine regions. Therefore, it is a mixed gland.
Exocrine region of the pancreas: The exocrine cells form clusters called acini or alveolar structures.
Endocrine region of the pancreas: The endocrine part of the pancreas consists of isolated islands of cells called islets of Langerhans. These cells are endocrine in nature and remain embedded within the pancreatic acini. These cells are highly vascular.
Around 1-2 million Islets of Langerhans are present in the pancreas. The cells of the islets are polygonal and are closely spaced with sinusoidal capillary networks.
Mainly Two Types Of Cells are found in the islets: or and cells. 6 cells and PP cells are also present in the islets, but A and cells are the primary ones.
Hormones secreted by the pancreas:
The hormones secreted by the pancreas are as follows—
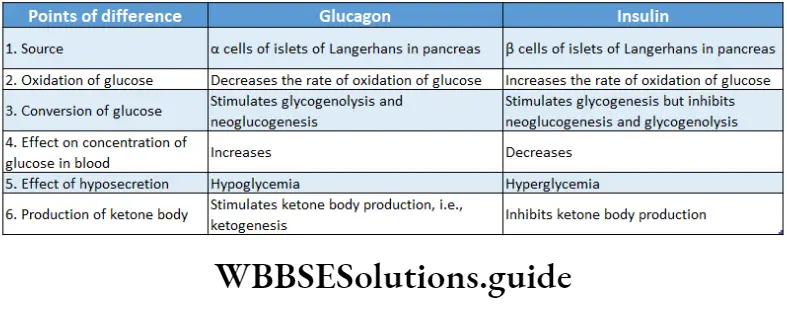
Insulin
- Source: It is produced by beta cells of islets of Langerhans.
- Chemical nature: It is a polypeptide hormone and is produced from proinsulin. It is made up of two peptide chains—A chain and B chain.
- Physiological Functions:
Carbohydrate metabolism:
- Insulin lowers elevated blood glucose levels after a meal,
- Insulin activates the glucose transporters and helps the target cells to take up excess glucose circulating in the blood.
- Insulin promotes glycogenesis. Thus, excess glucose is stored as glycogen in the liver and skeletal muscles,
- Insulin prevents glycogenolysis (conversion of glycogen into glucose), (e) Insulin also prevents gluconeogenesis (conversion of proteins and fats into glucose).
- These actions lower the concentration of glucose in the blood. Hence, insulin is also called Hypoglycemic Hormone
Lipid metabolism:
- Insulin induces the synthesis of fats from glucose and fatty acids, within the adipose tissues,
- It is known as an anabolic hormone because it prevents the oxidation of fats.
- It prevents the production of ketone bodies, thus, known as an antiketogenic hormone,
Protein metabolism:
- Insulin induces more reabsorption of amino acids, leading to more protein synthesis.
- It prevents the catabolic breakdown of proteins and the removal of amino acids.
Glucagon
Source: It is secreted by a -cells of the islets of Langerhans.
Glucagon Chemical nature: It is a polypeptide of 29 amino acid residues. Glucagon is synthesized from proglucagon.
Glucagon Physiological functions:
- Glucagon stimulates glycogen breakdown by glycogenolysis.
- It prevents the conversion of glucose into glycogen. Hence, it increases the glucose concentration in the blood,
- It also prevents the oxidation of glucose in the tissue fluid. Hence, glucagon is known as the ‘hyperglycemic hormone’.
- Glucagon acts as an antagonist to insulin,
- In the adipocytes, glucagon activates hormone-sensitive lipase. This enzyme then breaks down triglycerides (stored fat) into diacylglycerol and free fatty acids. It also helps to release them into the circulation.
Somatostatin
Somatostatin Source: Somatostatin is released from the 5 cells of the islets of the pancreas. It is also secreted by the hypothalamus and the mucous lining of the small intestine.
Somatostatin Chemical nature: Somatostatin is a 14 amino acid-containing peptide hormone.
Somatostatin Physiological functions:
Somatostatin has a generalized inhibitory effect on pancreatic exocrine and endocrine functions. It inhibits the secretion of both glucagon and insulin. Therefore, it acts as a local hormone (acts on the organ from where it is produced).
Outside the pancreas, it decreases the digestive activity of the digestive tract. It slows down the absorption of nutrients,
A very small amount of somatostatin is also produced in the hypothalamus which is transported to the anterior pituitary. Here it acts as a neurohormone to inhibit the release of growth hormone and thyrotropin,
It slows down the secretion of gastrointestinal hormones as well as the contractions of the stomach and duodenum.
Chemical coordination and integration chapter summary with important points
Pancreatic Polypeptide
Pancreatic polypeptide Source: Pancreatic polypeptide is secreted from PP cells of pancreatic islets.
Pancreatic polypeptide Chemical nature: It is a peptide hormone containing 36 amino acids.
Pancreatic polypeptide Physiological functions: It is responsible for the inhibition of pancreatic exocrine secretion, gall bladder contraction, modulation of gastric acid secretion, and gastrointestinal motility.
Gonads
Gonads are mixed organs that produce male and female gametes as well as hormones in males and females respectively.
The female gonad is the ovary and the male gonad is the testis. They are responsible for producing sex hormones in humans. These hormones regulate the formation of gametes.
They also determine the secondary sexual characteristics of adult males and females.
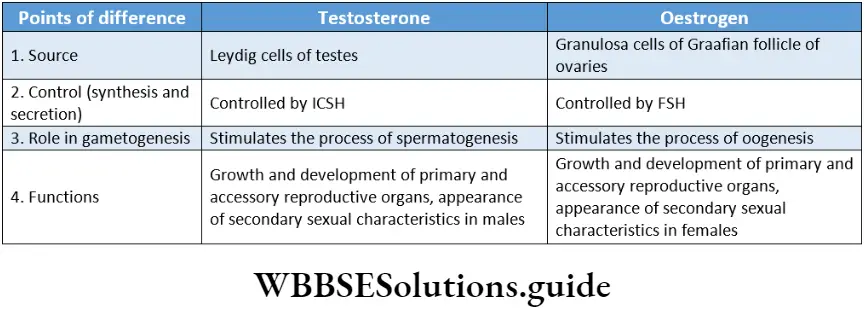
Gonads Testes
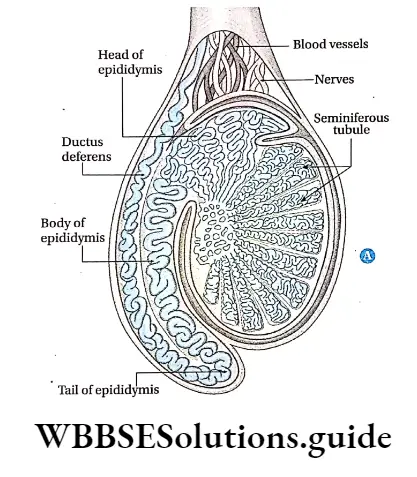
The testis (plural: testes) is the primary reproductive organ in males and is responsible for the production of male gametes or sperms.
Gonads Location: The testes are located inside the scrotum, outside the pelvic cavity, between the two legs.
Gonads Structure: The testis consists of numerous lobules. Each lobule is made of convoluted tubes, called seminiferous tubules.
The Leydig cells or interstitial cells, present in the connective tissue between the sperm-producing seminiferous tubules, are the endocrine cells. These cells are responsible for the production of testosterone, the principal male hormone.
Handwritten notes on chemical coordination and integration PDF download
Hormones secreted by testes: The hormones secreted by testes are called androgens or male sex hormones. The principal androgen is testosterone.
Testosterone
Testosterone Source: Testosterone is synthesized and secreted by the interstitial cells of the testes under the influence of interstitial cell-stimulating hormone (ICSH) or luteinizing hormone (LH).
The ICSH is secreted from the anterior pituitary gland. Some amount of testosterone is also secreted by the adrenal glands.
Testosterone Chemical nature: Chemically testosterone is a 19-carbon steroid.
Testosterone Physiological functions:
- Testosterone helps in the development of primary reproductive organs and accessory reproductive organs such as the epididymis, prostate gland, etc.
- Testosterone regulates the appearance of secondary sexual characteristics in males such as pubic hair, axillary hair, facial hair, etc.
- During adulthood, testosterone regulates normal sperm development.
- It increases energy metabolism, thereby increasing the BMR.
Testosterone promotes the synthesis of mucoproteins and collagen. This leads to greater accumulation of calcium ions in bones, making them longer and stronger. However, they prevent the lengthening of bones after adolescence,
It also helps in the personality development of males.
Ovary
The ovary is the primary female reproductive organ that is responsible for the production of female gametes or ova.
Ovary Location: They are located in the lower abdominal cavity, on both sides of the uterus. These are attached to the inner lining of the body, by folds of the peritoneum, called mesovarium.
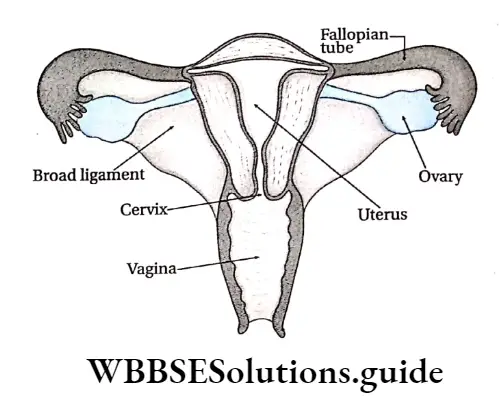
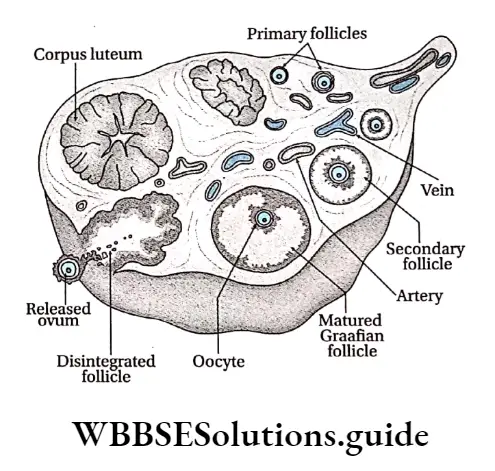
Ovary Structure: The ovary is almost oval-shaped. Its peripheral part is lined by epithelial cells. This layer is known as germinal epithelium.
This layer is followed by another layer called tunica albuginea, followed by the stroma. The stroma consists of an outer cortex layer and an inner medulla layer.
The outer cortex contains sac-like structures, called follicles of different sizes. These remain scattered in the connective tissue of the outer cortex. The inner medulla contains blood vessels, lymph vessels, etc.
The mature Graafian follicle within the ovary contains the ovum prior to ovulation (release of the ovum). Graafian follicle ruptures to release the secondary oocyte.
Under the influence of LH hormone, the disintegrated Graafian follicle is transformed into corpus luteum
Hormones secreted by ovary: Hormones secreted by the ovary have been discussed below.
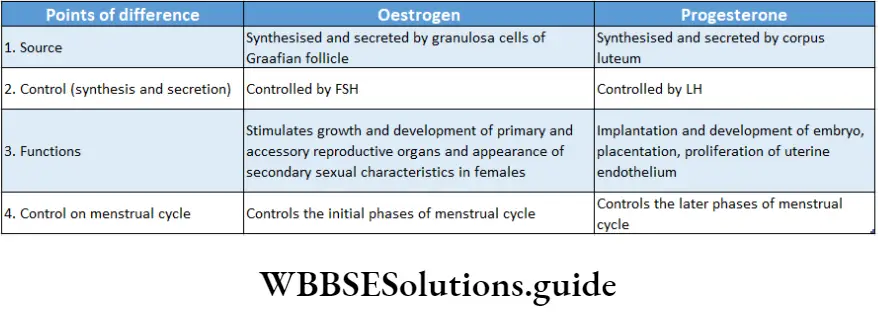
Oestrogen
Oestrogen Source: The parts of the ovary that secrete estrogen are—
Granulosa cells of Graafian follicle and corpus luteum. Secretion of this hormone is controlled by FSH, secreted from adenohypophysis of the pituitary gland.
Other than the ovaries, estrogen is also secreted by the adrenal cortex, testes (mainly Sertoli cells), and placenta (only during pregnancy).
Corpus luteum
- Graafian follicle contains the oocyte, in mammalian ovaries. After maturation, it releases the oocyte and itself degrades into an endocrine gland. This is known as the corpus luteum.
- It contains yellow-colored lutein granules. This endocrine gland secretes progesterone.
- This hormone is secreted when fertilization occurs and is necessary for preparing the uterus for the conception of the embryo.
- On the other hand, when fertilization does not take place, the corpus luteum gets degraded and progesterone is no longer secreted.
Corpus luteum Chemical nature: Oestrogen is a steroid compound.
Corpus luteum Physiological functions:
- Oestrogen is responsible for the growth and development of female reproductive organs,
- It is responsible for the onset of puberty and the appearance of secondary sexual characteristics, such as breast development, growth of pubic hair, etc., in females,
- Oestrogen stimulates the growth of the uterus and vagina during puberty. It is necessary for the maturation of the primordial follicle (primary stage of the follicle) into the Graafian follicle,
- The changes that take place within the ovaries and the uterus, during the early phases of the menstrual cycle (monthly cycle of changes that occur in the female reproductive system), are triggered by this hormone.
- Oestrogen causes the thickening of the uterine lining during the menstrual cycle in order to prepare for pregnancy,
- It maintains bone density and also the elasticity of skin and vaginal lining,
- It increases fat deposition in the subcutaneous layer under the skin.
Progesterone
Progesterone Source: Under the influence of luteinizing hormone (LH), the corpus luteum within the ovary synthesizes and secretes this hormone. Other than the ovaries adrenal cortex and placenta also secrete progesterone hormone.
Progesterone Chemical nature: Progesterone is a natural steroid.
Progesterone Physiological functions:
- Progesterone decreases contractility of the uterine smooth muscles and prepares the endometrium of the uterus for implantation of embryo,
- During the implantation of the embryo and embryonic development, progesterone helps to develop the placenta,
- Progesterone helps in the growth of the embryo throughout the gestation period (the duration of carrying an embryo or fetus inside the mother’s womb),
- It prevents the menstrual cycle as well as ovulation during pregnancy,
- It also helps in the growth of the mammary glands and the enlargement of breasts.
Relaxin
Relaxin Source: During pregnancy period, ovaries, placenta, and uterus produce this hormone.
Relaxin Chemical nature: Relaxin is a water-soluble polypeptide.
Relaxin Physiological functions: It causes the pelvic ligaments and pubic symphysis to relax. It helps in the relaxation of the cervix to facilitate the delivery of the baby.
Other hormones secreted by the ovaries
- Inhibin is secreted by the granulosa cells, present in the ovaries. This hormone inhibits the secretion of FSH from the anterior pituitary gland. Inhibins regulate LH and FSH release through endocrine feedback regulation at the anterior pituitary.
- Activin is also produced by the granulosa cells. It promotes the proliferation of granulosa cells. It also increases the number of FSH receptors on granulosa cells and modulates steroidogenesis (synthesis of steroids) in the ovarian follicles.
- Follistatin is a single-chain glycoprotein hormone found in ovarian follicular fluid. It is known to inhibit FSH release from the anterior pituitary.
Prostaglandin (PG)
The biologically active, lipid compounds that are synthesized from unsaturated fatty acids such as arachidonic acid, are called prostaglandins (PG).
It helps to carry out several physiological processes, such as—contraction and relaxation of the smooth muscles in the uterus (especially while receiving the ovum), secretion of HCl in the gastric juice, etc.
Placenta
The temporary organ present in the uterus of a pregnant woman, that maintains the mechanical and physiological connection between the mother and the developing embryo, is called the placenta.
Placenta Location: It is present within the inner walls of both the growing fetus and the mother.
Placenta Hormones secreted: There are several hormones secreted by the placenta that are involved in the maintenance of pregnancy and the growth of the embryo.
The hormones secreted by the placenta are—estrogen, progesterone, relaxin, chorionic thyrotropin, human chorionic gonadotropin, and human chorionic somatomammotropin.
Human chorionic gonadotropin (HCG)
Chemically, it is a glycoprotein in nature.
Its physiological functions are as follows—
- It helps to maintain the structure and growth of the corpus luteum. Therefore, it regulates the secretion of estrogen and progesterone.
- HCG stimulates the secretion of testosterone in the male fetus. Due to this influence, the sex organs develop and the testes descend into the scrotum, at the layer period of gestation.
- Human chorionic somatomammotropin (HCS) or Human placental lactogen (HPL)
Chemically, it is a polypeptide hormone.
Its physiological functions are as follows—
- HCS reduces the glucose concentration in the mother’s body, keeping the glucose available for the fetus.
- It also releases the fats from the fatty acids stored in the mother’s body.
- HCS increases the production of proteins and helps the fetus to grow.
Thymus gland
Thymus gland Location: This gland is located behind the sternum below the thyroid gland. It is situated partly in the neck region and partly in the thorax.
Thymus gland Hormones secreted: This gland secretes several hormones, such as thymosin, thymopoietin, thymulin, and thymic humoral factor. This gland is most active in children and adolescents. It gradually shrinks and becomes less active in adults.
Thymus gland Biological role:
- The hormones of the thymus gland regulate the development of T-lymphocytes.
- Thymosin and thymic humoral factors, increase immune responses against pathogens. The Thymus gland is called the Throne of immunity.
- Thymosin also stimulates the secretion of certain pituitary hormones (growth hormone, LH, gonadotropin-releasing hormone, ACTH, etc.)
Mechanism Of Hormone Action
- Hormones are responsible for transferring messages related to various physio-biochemical activities of the cells.
- They bind to hormone-specific receptor molecules at the target cells to form a hormone-receptor complex. This initiates a series of events that lead to the generation of second messengers within the cell (the hormone is known as the first messenger).
- The second messengers then trigger a series of molecular interactions that alter the physiological state of the cell. The entire process is called signal transduction.
Receptors
Receptors Definition: The cellular structures that recognize and bind to hormones are called receptors.
But in the current view, receptors can recognize and bind to a variety of other extracellular regulatory signaling molecules, such as growth factors and neurotransmitters.
Ligands
- Ligands are extracellular signaling molecules that bind to receptors. The receptor has the ability to specifically recognize a ligand among the different molecules present in the environment surrounding the cells.
- Ligand-receptor binding results in the activation of intracellular signaling pathways. As a result, amplification of the signal occurs which affects gene expression, i.e., synthesis of proteins according to the genetic information.
Receptors are classified into two main groups according to their location in the cells—
- Extracellular or cell surface receptors, located on the plasma membrane of the target cell (mainly for non-steroid hormones).
- Intracellular or nuclear transcription factor receptors are located inside the cell (mainly for steroid hormones).
Receptors are classified into two main groups according to their location in the cells—
- Extracellular or cell surface receptors, located on the plasma membrane of the target cell (mainly for non-steroid hormones).
- Intracellular or nuclear transcription factor receptors are located inside the cell (mainly for steroid hormones).
Extracellular Or Cell Surface Receptors
The hormones that are protein or polypeptide in nature (e.g., oxytocin, relaxin, etc.) are insoluble in lipids. Hence, they cannot move directly across the cell membrane of the target cell.
These hormones bind to specific receptor molecules located on the surface of the cell membrane.
These cell surface receptors are usually glycoproteins with three defined structural and functional domains—
- Extracellular domain: It contains the ligand binding site of the receptor and is hydrophilic in nature.
- Transmembrane domain: It anchors the receptor into the plasma membrane
- Intracellular domain: It contains amino acids, which are targets for phosphorylating enzymes that regulate receptor activity.
The hormone-receptor complex has two mechanisms of hormone action—
By cAMP formation, by changing the permeability of the plasma membrane.
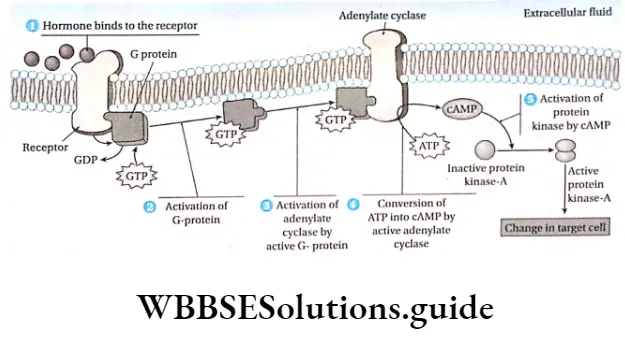
Mechanism Of Hormone Action By cAMP Formation
- When the hormone binds to the receptor, a conformational change occurs in the cytoplasmic domain of the receptor.
- This leads to the stimulation of an intracellular signaling pathway of guanosine nucleotide binding protein called G-protein. G-protein activates adenylyl cyclase.
- cAMP is synthesized from ATP by the action of adenylyl cyclase. This cAMP, after synthesis, triggers the activation of other enzymes and stimulates the metabolic processes in the cells. Here hormone acts as the first messenger and cAMP as the second.
Example:
- The action of epinephrine on liver cells may serve as an example where cAMP acts as a second messenger. It converts glycogen stored in the liver into glucose.
- The binding of the hormone to the receptor brings about changes in the receptor. As a result, GTP binds to G-protein at the intracellular domain of the receptor.
- One of the G-protein subunits dissociates, which is called active G-protein. This active G-protein then interacts with adenylyl cyclase.
- When activated by the G-protein subunit, adenylyl cyclase catalyzes the
formation of cAMP from ATP. - The cAMP formed at the inner surface of the plasma membrane diffuses within the cytoplasm.
- Then it binds to and activates protein kinase-A. This enzyme, in the presence of Mg2+ and ATP, activates inactive phosphorylase kinase.
- Active phosphorylase kinase converts inactive glycogen phosphorylase-b into active glycogen phosphorylase-a.
- Active glycogen phosphorylase-a converts glycogen into glucose-l-phosphate, which is further converted into glucose-6-phosphate.
- Finally, after the release of the phosphate group, it is converted to glucose.
Mechanism of hormone action by changing the permeability of plasma membrane
- In this case, the hormone-receptor complex changes the permeability of the cell membrane of the target cell.
- This allows the metabolic substance to enter the target cell which increases cellular metabolism.
Example:
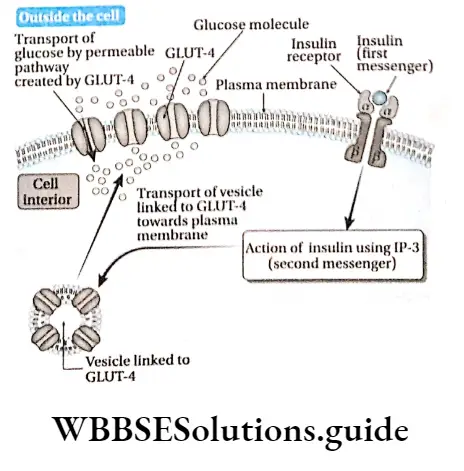
- Insulin changes the permeability of the sarcolemma of muscle cells or muscle fibers. Due to this, glucose molecules can easily enter the muscle cell or fiber, from circulation.
- The receptor for insulin, present in the cell membrane, has two -subunits and two -subunits. Insulin binds to the binding sites of outer a-subunits, to form the hormone-receptor complex.
- This changes the conformation of the subunits. As a result, activated subunits change into active tyrosine kinase, which further activates G-proteins present in the cell membrane.
- Active G-proteins further activate the phosphodiesterase enzyme. It converts phosphatidylinositol 4,5-biphosphate (PIP2), into inositol triphosphate (IP3)
and diacylglycerol (DAG). These compounds function as second messengers - Glucose Transporter like GLUt-4 can flow through the cytoplasm, with the help of IP3, towards the cell membrane.
- It binds to the cell membrane protein, changing its permeability. Thus the channels produced in the cell membrane, allow glucose to pass into the muscle cells.
Nuclear Receptors Or Intracellular Receptors
Nuclear or intracellular receptors are the receptors of steroid hormones. These are present in the cell cytoplasm. These receptors have binding sites for both hormones (ligands) and DNA. These receptors are transcription factors regulated by ligand binding.
Members of this family include the receptors for—
- Progesterone and estrogen,
- Glucocorticoids and mineralocorticoids,
- Vitamin D and thyroid hormone,
- Retinoic acid and 9-cis-retinoic acid,
- Orphan receptors (a group of receptors with unknown ligands).
Mechanism of hormone action involving intracellular receptors
This mechanism is described as follows—
- Steroid hormones and the active steroid derivative of vitamin D are lipid-soluble and hydrophobic. Therefore, they cross the plasma membrane to bind to intracellular hormone receptors. This forms a hormone-receptor complex.
- The binding of hormones to the receptor produces a conformational change in the structure of the receptor. It allows the hormone-receptor complex to enter the nucleus and bind to specific DNA sequences.
- This results in either activation or repression of gene transcription.
- Within the nucleus, the synthesis of mRNA (transpiration) increases. The mRNA is translated into Proteins in the Production Of Enzymes, Stimulating Metabolic Activities within the Cell.
Hormones As Chemical Messengers
- Hormones serve as chemical messengers in the body and help to maintain the internal chemical balance i.e., homeostasis of the body.
- Hormones regulate and coordinate physiological and metabolic functions by acting on receptors located on or inside target cells.
- They act on receptors of target cells located far away from the secretory cells or glands. They are carried to their target cells by plasma or lymph. These hormones stimulate the metabolic reactions within the target cells.
Example:
- Adenohypophysis of the pituitary gland secretes TSH hormone. It diffuses into the network of blood capillaries.
- It is carried to the location of the thyroid glands. It stimulates the thyroid glands to secrete the hormones T3 and T4. Thus, the hormone TSH acts as a chemical messenger.
Hormones As Regulators
- Hormones regulate the concentration of different components within the body fluids.
- They also regulate different metabolic processes in the body. This maintains the internal chemical balance.
Example:
- The islets of Langerhans of the pancreas, secrete hormones like insulin and glucagon.
- Both the hormones regulate the glucose concentration in the blood. When the concentration of glucose rises in the blood, insulin converts excess glucose into glycogen which gets stored in the liver.
- This lowers the blood glucose level. Glucagon, on the other hand, acts when the blood glucose level falls below normal.
- It converts glycogen proteins and fats into glucose. This increases the glucose concentration in the blood.
Role Of Hormomes In Maintaining Homeostasis
- Hormones are secreted by the endocrine glands. They are carried to their target cells by blood. They maintain equilibrium inside the cells.
- To maintain internal equilibrium, the secretion of hormones needs to be regulated according to the need.
- The decline or rise in the secretion of a hormone depends on its concentration in the blood. This mechanism is called feedback control.
This is of two types—
- Negative and
- Positive feedback control.
Negative Feedback Control
In this type of control mechanism, the synthesis of a hormone is reduced or entirely stopped when its amount in the blood is above normal.
Example:
- The normal concentration of T4 in human blood or serum is about 4-12 pg/lOOmL and that of T3 is about 80-200 ng/lOOmL.
- When the concentrations of these two hormones rise in the blood, a negative signal is generated and sent to the hypothalamus.
- This prevents the synthesis and secretion of TSH-RH from the neurosecretory cells of the hypothalamus. As a result, secretion of TSH from the thyrotroph cells of the adenohypophysis also decreases.
Positive Feedback Control
In this system, the synthesis of a hormone increases if its amount in the blood is below normal.
Example: When The Concentrations of these two hormones— T4 and T3 decrease in blood, a positive signal is generated and sent to the hypothalamus.
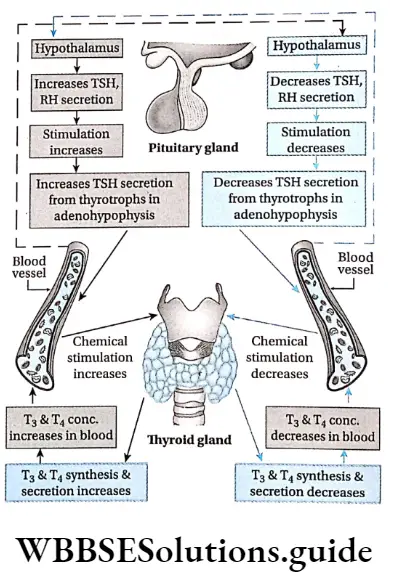
- This induces the synthesis and secretion of TSH-RH from the neurosecretory cells of the hypothalamus.
- Secretion of TSH-RH further stimulates the thyrotroph cells leading to increased secretion of TSH.
- Uterine contraction at the onset of labor in pregnant women releases oxytocin hormone from the posterior pituitary.
- The presence of this hormone intensifies the contractions. Increased uterine contraction causes more oxytocin to be released and the cycle goes on until the baby is born.
- The birth halts the release of this hormone, thus, ending positive feedback control.
Disorders Related To Endocrine Glands
- Various factors affect the secretion of hormones, causing several disorders diseases, or syndromes in the body.
- Oversecretion of the hormones is called hypersecretion, while less secretion of the hormones is called hyposecretion. Some of the disorders caused by hyper and hyposecretion of hormones have been discussed below.
Endocrine system and hormones notes for NEET and Class 11
Disorders Related To Pituitary Gland
The disorders related to the pituitary gland are as follows—
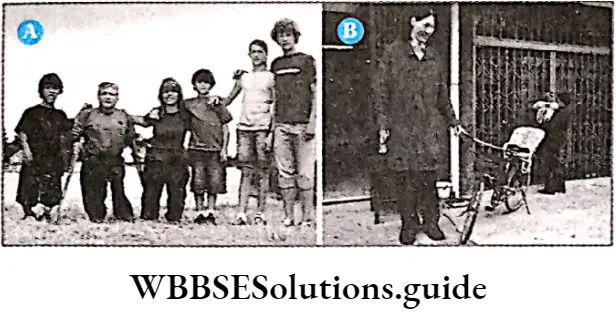
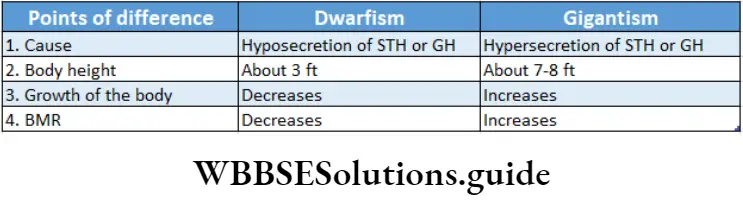
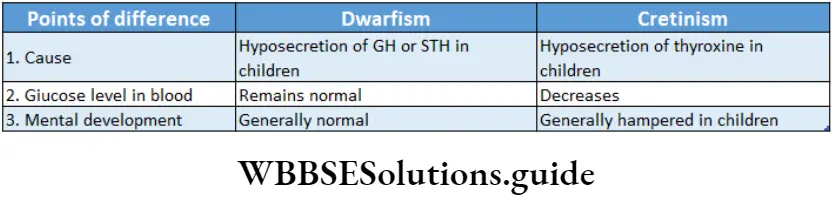
Dwarfism
Dwarfism is a disorder characterized by shorter-than-normal skeletal growth.
Dwarfism Causes: Two major causes of this disorder are achondroplasia and growth hormone deficiency (hyposecretion)
Achondroplasia: It is a disorder caused due to the presence of a defective allele in the human genome. It accounts for 70% of dwarfism cases. It often leads to increased spinal curvature and distortion of skull growth.
Growth Hormone Deficiency: It is a medical condition in which the body produces insufficient growth hormone. It may result in mutations of specific genes, damaged pituitary gland, Turner’s Syndrome (a disorder due to the absence of an X chromosome in females), poor nutrition, or even stress.
Growth Hormone Deficiency Symptoms:
- Children with growth hormone deficiency have a slow growth rate and have a short body build. The height may range up to 3 feet.
- More severe forms of dwarfism are associated with abnormal functioning of other organs, such as the brain or liver.
- Bones also get affected due to this disorder. Early degenerative joint disease, lordosis, or scoliosis (curvature in the vertebral column) can cause pain and disability.
- Improper growth and development of the; primary sex organs occur, leading to infertility, The Appearance of secondary sexual characteristics may also get delayed.
Growth Hormone Deficiency Treatment:
- Early diagnosis and treatment can prevent some of the problems associated with dwarfism.
- People with dwarfism due to growth hormone deficiency can be treated with growth hormone.
- However, the treatment should begin before adolescence. After adolescence, the treatment will become ineffective.
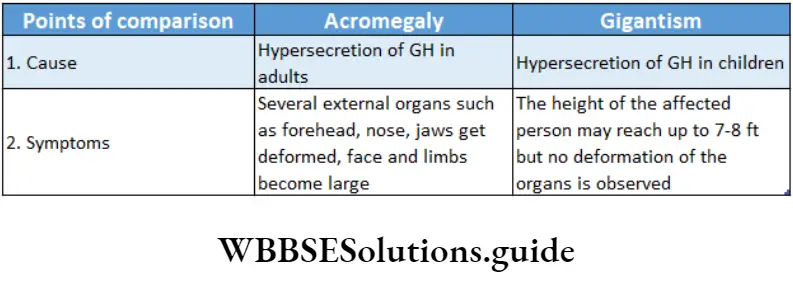
Gigantism
Gigantism is the condition of abnormal growth in height and elongation of long bones in childhood.
Gigantism Causes: Gigantism may result due to—
- Hypersecretion of STH or GH in childhood
- Tumour in the acidophilic cells or adenoma in the adenohypophysis region, before the onset of adolescence.
Gigantism Symptoms:
The skeletal system and muscles show increased growth than normal. The hands and feet become larger.
- The height of the body reaches 7-8 ft.
- Growth of the different internal organs gets stimulated.
- Basic Metabolic Rate (BMR) increases.
- The growth of different endocrine glands or endocrine cells is comparatively less. The Thymus gland increases in structure.
- The glucose concentration in the blood increases.
Gigantism Treatment: This disorder can be treated by surgery, radiotherapy, etc. However, the treatment must be started at the early stage.
Acromegaly
Acromegaly is caused by hypersecretion of growth hormone (GH) in adults, resulting in an abnormal increase in bone and soft tissue growth.
Acromegaly Causes: The causes of acromegaly are—
Hypersecretion of growth hormone in adult tumors in the acidophilic cells of the adenohypophysis of the pituitary gland.
Acromegaly Symptoms:
- Excess GH secretion leads to disproportionate skeletal growth. The appearance becomes gorilla-like with a lower jaw protruding forward and a forehead slanting forward.
- Soft tissue swelling acromegaly Acromegaly is caused by hypersecretion of growth hormone (GH) in adults, resulting in an abnormal increase in bone and soft tissue growth.

Causes: The causes of acromegaly are—
- Hypersecretion of growth hormone in adults
- Tumour in the acidophilic cells of the adenohypophysis of the pituitary gland.
Symptoms:
Excess GH secretion leads to disproportionate skeletal growth. The appearance becomes gorilla-like with the lower jaw protruding forward and the forehead slanting forward.
Soft tissue swelling kidney, etc., results in the weakening of muscles in these organs. Weak muscles around vocal cords lead to thick, deep voices and slow speech patterns.
Treatment: Current treatment options include surgery, radiotherapy, etc. Other than these, treatment with somatostatin analogs (stop GH production) and dopamine agonists like bromocriptine (reduce the size of the tumor and control GH-induced hyperglycemia) are useful.
Diabetes Insipidus
This disease is caused by the hyposecretion of ADH hormone from the posterior pituitary gland.
Disorders Related To Thyroid Gland
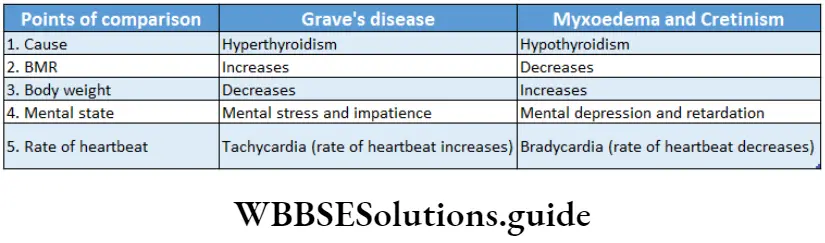
- The disorders related to the thyroid gland are as follows—:% Cretinism Cretinism is a disorder caused by to hyposecretion of thyroid hormones.
- It is characterized by stunted physical and mental growth in children. It is also known as congenital hypothyroidism.
Thyroid Gland Causes:
- Reduced secretion of thyroid hormones (hypothyroidism) is the major cause of cretinism in children.
- Deficiency of iodine in maternal nutrition may cause this disorder in the newborn.
Thyroid Gland Symptoms:
- Reduced growth of the body. The limbs are shorter than normal.
- The tongue thickens and protrudes from the mouth involuntarily. Excess saliva secretion occurs. Short and wide neck, pot belly, scanty hair, and swollen eyelids are observed.
- Glucose, iodine, and thyroxine concentrations decrease in the blood.
- The growth of primary sex organs and the appearance of secondary sexual characteristics get delayed. Treatment: Hormone therapy is the common approach for treating hypothyroidism. Daily intake of thyroxine hormone tablets can counter this disorder.
Myxoedema
Myxoedema is caused due to the deficiency of thyroxine hormone in adults. It is more common in females than in males.
Myxoedema Causes:
- Hyposecretion of thyroxine in adults causes myxoedema. This occurs due to the deficiency of iodine. Removal of the thyroid gland by surgery, use of antithyroid drugs, or ionizing radiations may cause myxoedema.
- Autoimmune thyroiditis (an inflammatory disorder of the thyroid gland) may lead to myxoedema.
- Hashimoto’s disease or autoimmune thyroiditis
- It is an autoimmune disease and occurs when our immune system attacks the thyroid tissue.
- It results in the inflammation of the thyroid gland (thyroiditis) and may cause hypothyroidism.
Myxoedema Symptoms:
- The limbs and neck become swollen. This occurs due to the accumulation of mucus
within the cells in this region. So it has been named myxoedema (edema caused by to accumulation of mucus). - Loss of memory takes place.
- Anorexia (eating disorder) is observed among the patients.
- BMR decreases.
- The rate of heartbeat decreases.
- Due to the swollen nature of the face, the eyes appear tiny.
- Levels of carbohydrates, iodine, and thyroxine in the blood, decrease.
Myxoedema Treatment: Introducing thyroxine hormone into the body, through the process of hormone therapy, may be helpful in treating myxoedema.
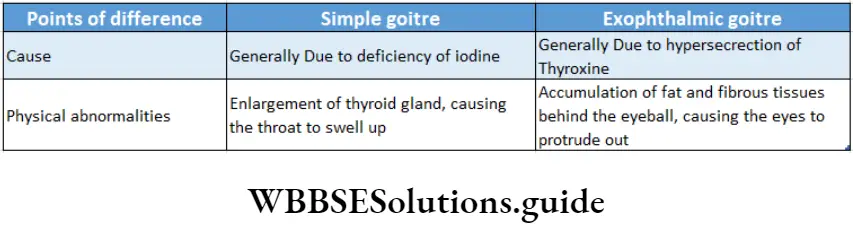
Goitre
Goitre is characterized by the enlargement of the thyroid gland. It may be caused due to hypo or hyperthyroidism.
Goitre is generally of two types—
Simple goiter: The condition of an enlarged thyroid gland, due to the hyposecretion of thyroxine is called simple goiter.
Goitre Causes:
- It is caused due to deficiency of iodine in the diet which results in low thyroxine secretion.
- In response to this, there is reduced negative feedback inhibition of TSH. The elevated TSH secretion stimulates the thyroid to enlarge.
- People living in hilly regions suffer from endemic goiter because the soil in those regions does not contain iodine.
- The secretion of T3 and T4 hormones may be less due to genetic defects.
Goitre Symptoms: This disease is characterized by the enlargement of the thyroid gland. This is manifested as a swelling of the front part of the throat. In severe cases, an enlarged thyroid can exert pressure on the trachea and esophagus.
This can lead to—
Breathing trouble which may lead to the condition of dyspnoea,
- Cough,
- Hoarseness of voice,
- Difficulty in swallowing.
Goitre Treatments: The regulated use of iodized salt allows the thyroid gland to producer the thyroid hormones and therefore helps to prevent simple goiter. It can also be treated by consuming iodine-rich food like marine fish.
Exophthalmic Goiter or Grave’s disease: The condition in which the thyroid gland becomes overactive, in the case of hyperthyroidism, is called exophthalmic goiter.
Exophthalmic Goiter Causes: Increased TSH receptor stimulation leads to thyroid hyperplasia (follicles enlarge in size), causing enlargement of the thyroid gland. This leads to hypersecretion of thyroxine hormone.
NEET chemical coordination and integration revision notes with MCQs
Exophthalmic Goiter Symptoms:
- The eyes protrude because of edema in the tissue of the eye socket. Eye muscles swell and cause less blinking of the eyelids.
- The person may not be able to close his eyes while sleeping. This causes drying up and infection of the conjunctiva.
- The patient usually becomes hyperactive, nervous, irritable, and suffers from insomnia.
- The BMR increases.
- The heartbeat also increases.
- Hypersecretion of thyroid hormones results in osteoporosis in the patients.
Exophthalmic Goiter Treatments:
Hyperthyroidism can be treated with propylthiouracil, methimazole, etc. These drugs prevent the bond formation between iodine and tyrosine.
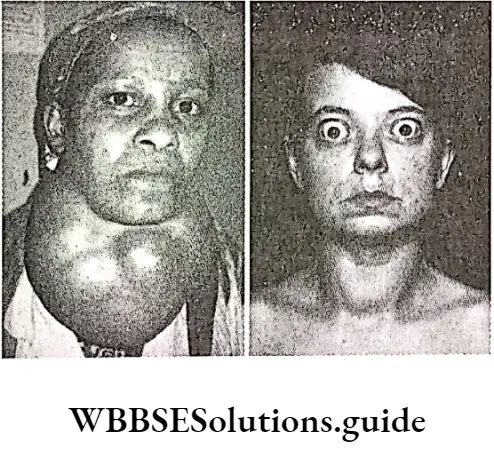
This prevents the formation of thyroxine. Removal or destruction of a portion of the thyroid by means of radioactive iodine is sometimes effective therapy in this condition.
Disorders Related To Parathyroid Gland
The disorders related to the parathyroid gland are as follows
Hypoparathyroidism
The disorder caused by to hyposecretion of parathyroid hormone from the parathyroid gland is called hypoparathyroidism.
Hypoparathyroidism Causes:
- Hypoparathyroidism is caused by the hyposecretion of parathyroid hormone (PTH).
- Hyposecretion of PTH may be due to inflammation or a tumor in the parathyroid gland.
Hypoparathyroidism Symptoms:
- The calcium level in the blood decreases, i.e., hypocalcemia occurs.
- The contraction-relaxation mechanism of the muscles decreases, and spasms occur within the muscles.
- When this condition becomes severe, hands, fingers, etc., become distorted leading to the condition of tetany.
- In the case of women, the menstrual cycle is painful.
- The skin becomes dry and nails become brittle.
- Fatigue, weakness, headache, mental depression, etc., are also some important symptoms of the disease.
Hypoparathyroidism Treatment: During the initial stages of the disease, introducing calcium and vitamin D supplements within the body, may be helpful.
Hyperparathyroidism
- The disorder caused by to hypersecretion of PTH hormone from the parathyroid gland is called hyperparathyroidism.
- Hyperparathyroidism Causes: The main cause of this disorder is excess PTH secretion. Due to the presence of a tumor in the parathyroid gland, secretion of PTH increases.
Hyperparathyroidism Symptoms:
- The concentration of calcium in the blood increases i.e., hypercalcemia is observed.
- Renal calculi may occur due to excess calcium deposition.
- The bones may become soft and distorted due to the leaching of calcium. Cysts may be found within the bone. This abnormality of bones is called osteitis fibrosa cystica or brittle bone disease.
- The muscular layer of the inner lining of the left atrium may get thickened, known as left ventricular hypertrophy. This leads to malfunctioning of the heart.
Hyperparathyroidism Treatment: The tumor containing the parathyroid gland has to be removed by surgery.
Chemical Coordination And Integration
Tetany
The disorder involves involuntary contraction of muscles or muscle spasms. It is caused by to malfunction of parathyroid glands and consequent deficiency of calcium.
Tetany Causes: The various causes of tetany are as follows— Hypocalcemia (deficiency of calcium),
- Hypoparathyroidism,
- A low level of magnesium and a higher level of phosphate in the blood,
- Deficiency of vitamin D and calcium in the diet, for a long period of time,
- Infection with Clostridium tetani.
Tetany Symptoms:
- Due to sudden contraction of the facial muscles, the nose and lips become distorted.
- Due to muscular spasms, wrists, fingers, joints, etc., become distorted. Especially the thumb bends towards the palm.
- In some cases, paresthesia may occur, and a piercing or burning sensation is felt.
- Treatment: For the treatment of tetany, Ca and vitamin D supplement is essential. This restores the calcium concentration in the blood.
Disorders Related To Pancreas
The disorders related to the pancreas are as follows—
Diabetes mellitus
Diabetes mellitus is a disorder characterized by increased blood glucose levels.
In general, there are two forms of diabetes mellitus—
Type 1 (TIDM) and Type 2 (TIIDM).
Type 1 Diabetes Mellitus: It is caused due to reduced secretion of insulin. Thus, type 1 Diabetes mellitus is also called insulin-dependent diabetes (IDDM)
Type 1 Diabetes Mellitus Cause: Low insulin secretion due to autoimmune destruction of the islet cells is the major cause of type I diabetes mellitus.
This results in impaired entry of glucose into the cells and hence, reduced accumulation of glucose in the blood.
Type 1 Diabetes Mellitus Symptoms:
- Accumulation of glucose in the blood (hyperglycemia) leads to increased plasma osmolarity (glucose concentration more than 80-120 mg/100 mL).
- This is accompanied by excess loss of water and sodium (polyuria).
- Excess glucose in blood leads to the discharge of excess glucose through urine (glycosuria).
- The resulting dehydration triggers compensatory mechanisms such as thirst (polydipsia).
- The inability of the cells to utilize glucose creates a state of cellular starvation.
- It also leads to the accumulation of ketone bodies in the blood (ketoacidosis). Diabetic ketoacidosis is an acute pathologic event characterized by elevated blood glucose levels, ketone bodies, and metabolic acidosis.
Type 1 Diabetes Mellitus Treatment: By taking proper medical advice, the glucose level in the blood can be kept under control. In severe cases, insulin therapy may be used.
Type 2 Diabetes Mellitus: Type 2 diabetes mellitus is also called Insulin-independent or non-insulin-dependent diabetes mellitus (NIDDM). It is much more common than type 1, accounting for about 90% of cases.
Type 2 Diabetes Mellitus Causes: Type 2 diabetes mellitus is caused due to a decreased responsiveness of insulin receptors in the peripheral tissues to insulin. This inhibits the action of insulin (insulin resistance) and causes a decrease in the absorption and oxidation of glucose in the cells. As a result, glucose concentration rises in the blood.
Type 2 Diabetes Mellitus Symptoms:
- Symptoms include hyperglycemia, glycosuria, dehydration, etc., which are also observed in the case of IDDM.
- Other than these, the retina may get damaged (retinopathy), which can lead to blindness.
- Diabetes mellitus is associated with increased risk factors for coronary heart disease (CHD).
- Some long-term complications include nephropathy (damage of nephrons) that leads to renal failure, and neuropathy (damage of neurons).
- Treatment: Treatment aims at the control of blood sugar, and is monitored by prevailing levels of glycosylated hemoglobin.
- Regular medical check-ups must be conducted to keep the blood glucose under control.
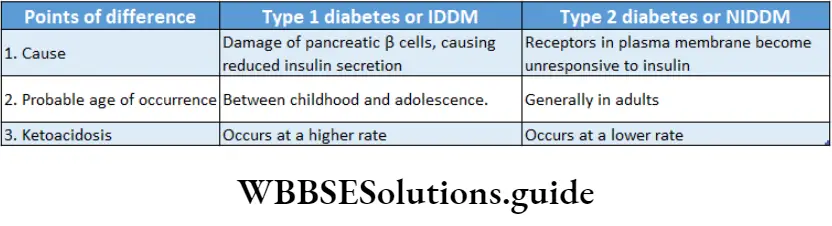
Hypoglycemia due to over-secretion of insulin
Due to the over-secretion of insulin by the beta 3 cells of islets of Langerhans, the glucose level decreases in the blood (about 50 mg/100 mL of blood). This is called hypoglycemia.
This condition leads to weakness. In severe cases, a person may suffer from muscle contractions, convulsions, and even coma.
Disorders Related To Adrenal Cortex
The disorders related to the adrenal gland are as follows—
Addison’s disease
Addison’s disease is caused by low secretion of adrenal hormones, cortisol and aldosterone also occurs due to antibodies produced against the cortical cells, and microbial infection of glands or tumors.
Addison’s Disease Symptoms:
- The main symptoms of Addison’s disease include loss of appetite, weakening of muscles, decrease in BMR, and decrease of storage of proteins in the body.
- Lack of aldosterone results in loss of sodium and water and retention of potassium. This leads to low blood pressure and possibly severe dehydration.
- Without cortisol, glucose concentration decreases in the blood, causing hypoglycemia.
- As ACTH causes a buildup of melanin deposition, hence, hyposecretion of ACTH leads to the darkening of the skin.
- Mental stress is also seen.
Addison’s Disease Treatment: Hormone replacement therapy is the standard treatment for Addison’s disease.
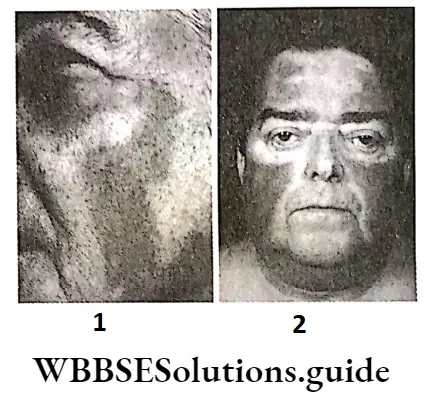
Cushing’s Syndrome
This disorder is caused by the abnormally high levels of cortisol.
Cushing’s Syndrome Causes: Cushing’s syndrome is caused by high levels of cortisol secreted from the adrenal cortex in the body.
This may occur due to a tumor in the adrenal cortex. Even tumors in the pituitary gland can lead to such diseases. Over-secretion of ACTH and prolonged ACTH therapy may cause Cushing’s syndrome.
Cushing’s Syndrome Symptoms:
- Muscle protein is metabolized, leading to muscle degeneration.
- Excess subcutaneous fat is deposited especially around the midsection of the body due to the over-secretion of cortisol. For this reason, the trunk appears obese, while the arms and legs appear thinner.
- The depletion of calcium from the bones leads to osteoporosis (brittle bones).
- An excess of aldosterone and reabsorption of sodium and water by the kidneys leads to a basic blood pH and hypertension.
- Hyperglycemia along with mental stress and depression are seen.
- The face becomes moon-shaped due to swelling. This is known as the moon face.
Cushing’s Syndrome Treatment: Treatments include surgery, radiation, chemotherapy, or the use of cortisol-inhibiting drugs.
Transsphenoidal adenomectomy (surgical removal of the tumor) is the most widely used treatment.
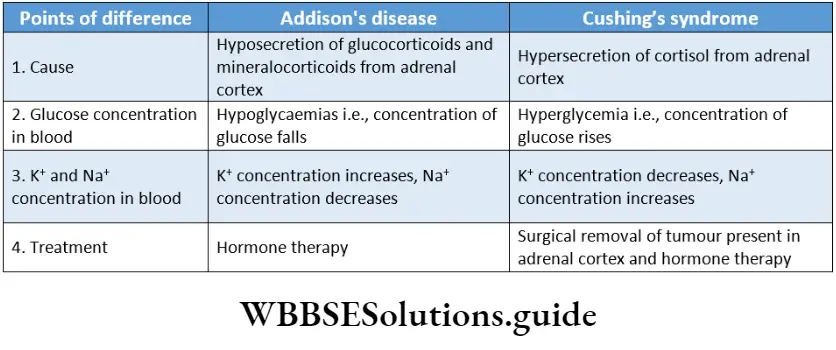
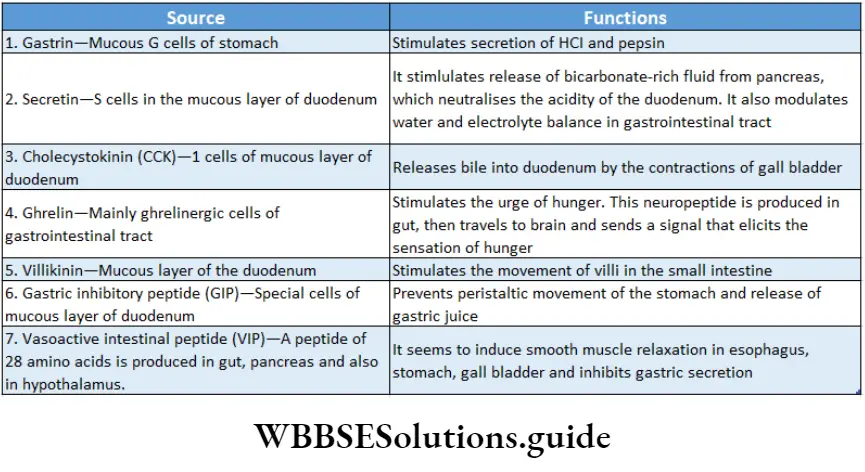
Chemical Coordination Notes
- Acinus: Cluster of cells resembling many-lobed berry.
- Anorexia: An eating disorder characterized by weight loss and or lack of appetite
- Catecholamine: Organic compounds containing catechol and a side chain amine (Collectively epinephrine non-epinephrine).
- Hyperfunctioning: Increased activity of an organ system or its parts
- Neurohormones: Hormones Released By Neurons
- Signal: Message Transmitted On Binding Of A molecule (like Hormone) To Its Receptor.
- Target Organs: The organ That Acts As The site Of a Hormone.
Points Of Remember
- The nervous system and the endocrine system both, work together, to maintain the coordination among different organs while regulating their functions.
- Glands are the most important part of the endocrine system.
- Glands may be of three types—exocrine, endocrine, and exocrine.
- Exocrine glands secrete enzymes, that are carried by ducts from the synthesizing cells to the target cells.
- Exocrine glands are of three types on the basis of their modes of secretion—merocrine, apocrine, and holocrine.
- Endocrine glands secrete hormones, that are carried by blood or lymph to the target cells situated away; from the synthesizing cells.
- Exocrine glands have both exocrine and endocrine properties.
- The study of endocrine glands, hormones, and their associated effects is called endocrinology.
- Thomas Addison is known as the ‘Father of Endocrinology1.
- Some of the endocrine glands include— the hypothalamus, pituitary, pineal gland, thyroid gland, parathyroid gland, adrenal gland, pancreas, gonads, thymus, and placenta.
- Tropic hormones regulate the functioning of the other endocrine glands.
- Neurohormones are secreted by nerve cells. These include ADH and oxytocin.
- The hypothalamus serves as the main connection between the endocrine and nervous systems.
- Herring bodies are large swellings at the terminal end of the axons at the posterior pituitary. These temporarily store ADH and oxytocin hormones.
- FSH is also known as the gametokinetic factor.
- The presence of hCG hormone in the urine of females is a determining factor, used in a pregnancy detection kit.
- Hormones bind to their specific receptors, thereby forming hormone-receptor complex.
- The receptors may be of two types—extracellular and nuclear or intracellular receptors.
- Myasthenia gravis is a disease caused by the hyposecretion of the hormone, thymosin.
- Several endocrine cells are also present in the gastrointestinal tract. These cells secrete gastrointestinal hormones, which help in digestion.
