Digestion And Absorption Introduction
Digestion And Absorption
Your body Requires Energy To Carry Out the Various metabolic processes. This energy is provided by food. It contains nutrients such as carbohydrates, fats, proteins, vitamins and minerals, that are required for overall nutrition and growth of the body.
What happens to the food after eating? But how does the body get these nutrients from food? Here, the digestive system comes into play.
The overall function of the digestive system is to convert the complex food molecules that are ingested, into smaller and simpler molecules.
These simpler molecules can be absorbed by the intestinal cells and are distributed throughout the body via the blood.
These nutrients are utilised for cellular metabolism and also as the building blocks needed for cell growth and repair. In this chapter, you shall study more about digestion and absorption of food.
Digestion and absorption notes for NEET PDF
Digestion
Digestion Definition: Digestion is a physiological process by which enzymes break down complex and insoluble organic components of food, into simpler, soluble substances that can be absorbed and assimilated easily by the cells of the body.
Digestion Can Be Of Different Types Based On—
- Site of Occurrence
- Process Of Digestion.
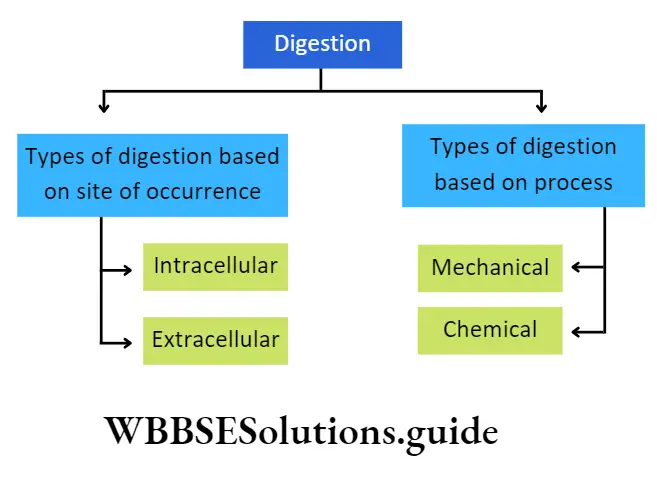
Types Of Digestion Based On Site Of Occurrence: Based on the site of occurrence, digestion can be of two types—intracellular digestion and extracellular digestion.
Intracellular Digestion: The process by which the digestion of food takes place within the cell, is called intracellular digestion. In this process, the cell engulfs the food materials and encloses those inside food vacuoles or endosomes. The cytoplasm, surrounding the food vacuoles, secrete digestive enzymes. This type of digestion is mainly found in protozoa, cnidaria, etc.
Intracellular Digestion Can Be Further Divided Into Two Types—
Heterophagic digestion involves breaking down external substances engulfed by the cell via pinocytosis or phagocytosis.
Autophagic digestion involves consuming components present within the cell.
| Class 11 Biology | Class 11 Chemistry |
| Class 11 Chemistry | Class 11 Physics |
| Class 11 Biology MCQs | Class 11 Physics MCQs |
| Class 11 Biology | Class 11 Physics Notes |
Class 11 biology digestion and absorption notes with diagrams
Extracellular Digestion: The process in which the digestion of food takes place outside the cell is called extracellular digestion.
In this process, the food materials are digested within the alimentary canal, with the help of enzymes containing digestive juices. This type of digestion is found in multicellular organisms such as human beings.
In humans, the mode of nutrition is holozoic.
This Type Of Nutrition Has Five Parts—
- Food intake or ingestion,
- Digestion of food,
- Absorption of nutrients,
- Assimilation of nutrients and
- Egestion or defecation of unabsorbed, undigested food residues.
Types Of Digestion Based On The Process: Based on the process, digestion is of two types— mechanical or physical digestion and chemical digestion.
Mechanical Or Physical Digestion: The process of breaking down larger food particles into smaller particles is called mechanical or physical digestion. This increases the surface area of the food so as to quicken further processes of digestion. It takes place within the mouth by the mastication process.
Chemical Digestion: The process of breaking large particles of food into simple and absorbable form, by the action of the digestive enzymes is called chemical digestion. It takes place in the mouth, stomach and small intestine.
Physiology Of Digestion And Absorption
Absorption
Absorption Definition: Absorption is the process by which digested products and nutrients present in the food move across the epithelium of the alimentary canal into the blood and lymph.
The absorbed nutrients then enter the blood or lymph for circulation to the tissues.
Absorption Site Of Occurrence: Absorption of digested food occurs mainly at three sites of the digestive system— The stomach (a little bit), the Small intestine, and the large intestine.
Absorption Types: The small intestine absorbs the end products of digestion, by two mechanisms of absorption—
- Active absorption,
- Passive absorption.
Absorption Active Absorption: It is an energy-requiring process by which nutrients are absorbed against a concentration gradient from the intestinal lumen by the intestinal epithelial cells.
Passive Absorption: In this process, the nutrients are absorbed along the concentration gradient from the intestinal lumen by the intestinal epithelial cell.
Short notes on digestion and absorption for quick revision
Digestive System
Digestive System Definition: The physiological system in the animal body that is responsible for ingestion and digestion of food, absorption and assimilation of nutrients and digested products and ingestion of undigested food is called the digestive system or alimentary system.
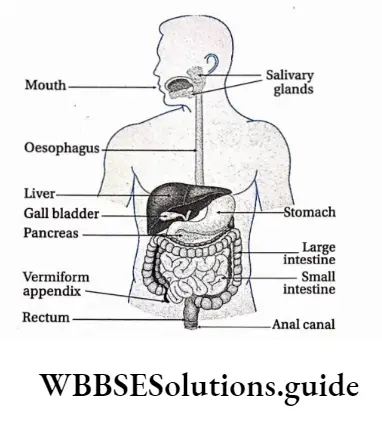
The human digestive system is divided into—
- Alimentary canal or food canal and
- Digestive glands. Different parts of the human alimentary system are given in the following chart.
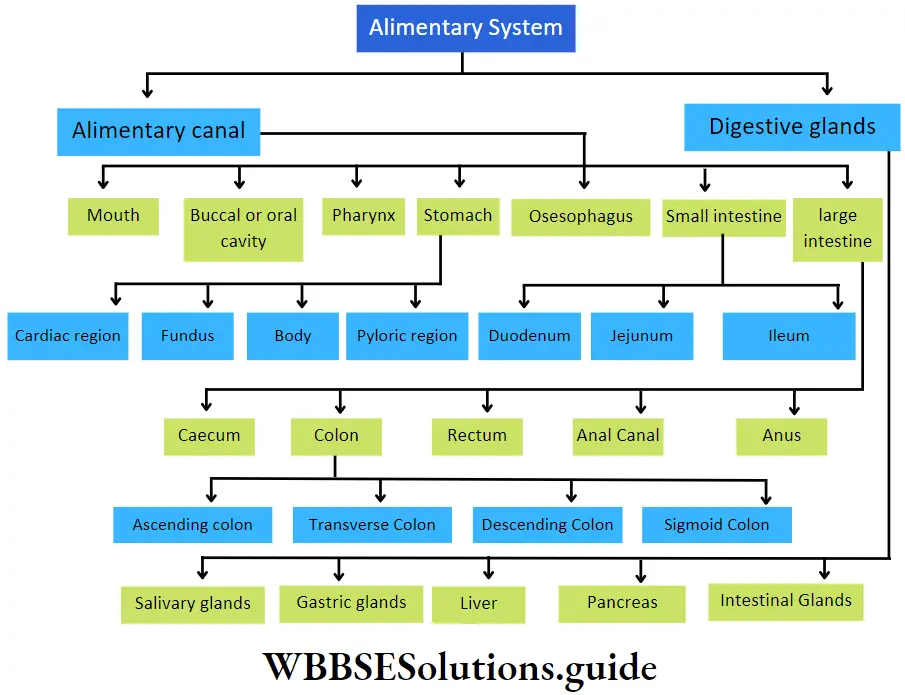
Alimentary Canal
Alimentary Canal Definition: The long, muscular tube-like structure that is part of the alimentary system through which the food passes during digestion is called the alimentary canal.
The nutrients are absorbed from the digested part of food into the blood whereas the undigested or non-essential portion is eliminated as waste. The alimentary canal is also called the digestive tract.
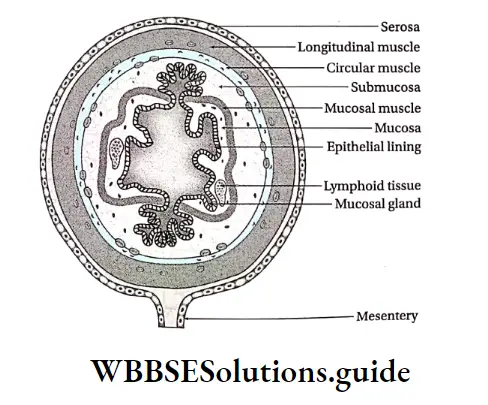
Histological structure human alimentary canal
The histological structure of the human alimentary canal consists of the following layers—
Mucous layer or tunica mucosa: It is the innermost layer of the alimentary canal. The mucus, secreted from the cells of this layer, keeps the inner wall of the alimentary canal slimy. Thus, the wall is protected from mechanical shocks and enzymatic activity of the digestive enzymes.
The glandular cells of the mucous layer secrete several hormones and digestive enzymes. This layer is thrown into circular folds or plicae circulares (or valves of Kerkring or valvulae conniventes) in the intestine.
The intestinal wall also bears numerous finger-like projections called villi. Longitudinal folds observed in an empty stomach are called rugae. The mucous layer itself is made up of three sub-layers.
Short notes on digestion and absorption for quick revision
They are as follows—
Epithelial layer: This is the innermost layer of mucosa. It remains in direct contact with the food passing through the alimentary canal. It consists of different types of cells lined on a basement membrane.
For example, the oral cavity, tongue, pharynx and oesophagus contain squamous epithelial cells. On the other hand, in the stomach, small intestine and large intestine this layer is made up of columnar epithelial cells.
Lamina propria: This is a thin layer of areolar connective tissue that lies beneath the epithelial layer.
This layer contains blood and lymph vessels. The cell population is variable in this layer and can include fibroblasts, macrophages, lymphocytes, eosinophils, etc. These cells provide immunity to the alimentary canal.
Muscularis mucosa: This is the outermost layer of mucosa, made up of smooth muscle fibres. Its contraction produces movement of the mucosa independent of the peristaltic movement of the entire wall of the digestive tract. This layer is absent in the oral cavity and at the pharynx.
Submucous layer or tunica submucosa: This layer remains surrounding the mucous layer and is made up of fibrous and areolar connective tissue. Numerous blood vessels, lymph vessels and nerve fibres are present in this layer. Parasympathetic and sympathetic nerves are present in clusters at different places, forming the submucosal plexus or Meissner’s plexus.
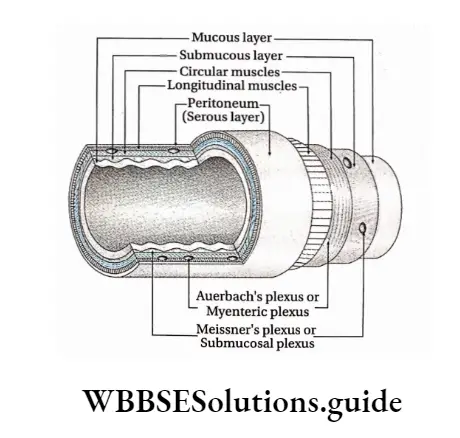
Muscular layer or muscle layer or tunica muscularis: This layer lies next to the submucous layer and is made up of smooth muscle fibres.
This layer is further subdivided into two layers—
- Inner circular
- Muscle layer and
- Outer longitudinal muscle layer.
A thin connective tissue layer containing blood vessels, lacteals and nerve fibres separates these two layers. In the stomach, another layer called the oblique layer is present between these two sub-layers.
Sympathetic and parasympathetic nerves form clusters at different parts within this layer, forming Auerbach’s plexus or myenteric plexus. The muscular layer is responsible for peristaltic contractions. The circular muscle layer forms sphincters at specific locations of the digestive tract.
Serous layer or tunica serosa: It is the outermost layer of the alimentary canal, made up of a layer of simple squamous epithelium (or mesothelium), supported by an underlying areolar connective tissue layer.
This layer is also called tunica adventitia. The parts of the alimentary canal present in the abdominal and pelvic cavity, are covered with a serous layer known as peritoneum. It contains a large number of blood vessels, lymph vessels and lymph nodes.
The peritoneum is made up of two membranes—
- Visceral peritoneum, which protects the internal organs present in the peritoneal cavity.
- Parietal peritonium, that forms the inner lining of the abdominal cavity.
Different parts of the alimentary canal have been discussed separately
Different Parts Of The Human Alimentary Canal
The different parts of the human alimentary canal have been discussed below.
Mouth
The mouth is the opening present at the beginning of the alimentary canal through which the intake of food takes place.
Mouth Location: It is present at the beginning of the alimentary system, just below our nose.
Mouth Structural features:
- The mouth is a transverse slit, bounded by two movable lips.
- The lips are covered with skin on the outer side and mucous membranes on the inner side.
- The inner wall of the mouth is covered with stratified squamous epithelium.
- The small vertical groove present in the middle region of the upper lip is called the philtrum. The philtrum extends and forms another structure called a tubercle.
Mouth Functions:
- The mouth helps in food intake. The lips help in opening and closing of the mouth. They assist in the intake of food as it passes into the mouth.
- As lips have a large number of nerve endings, they are considered tactile organs, and sensitive to touch and temperature.
- The mouth also plays an important role in communication, making sound and speech.
Buccal or oral cavity
The cavity that lies just behind the mouth where the ducts from the salivary glands open is called the buccal or oral cavity.
- Location: It is present just behind the mouth.
- Structural features: The structural features of the different parts of the buccal cavity are as follows.
Mouth Hard and soft palate:
- The concave roof of the mouth is called the palate.
- The anterior bony part of it is called the hard palate. The posterior muscular region that is continuous with the hard palate is called the soft palate.
- The hard palate is covered by a thick mucous membrane. The mucous membrane covering the floor of the nasal cavity is continuous with a soft palate.
- A small projection called the uvula or velum palati, hangs free from the posterior region of the soft palate. During the act of swallowing or deglutition, it prevents pieces of food from entering the nasal cavity.
Mouth Jaw:
- The oral cavity is lined by an upper and a lower jaw. They are hard, bony and contain teeth. The upper jaw is attached to the skull, hence immovable.
- However,- the lower jaw can be moved both sideways and down.
- The jaw bones are covered by gums or gingivae (singular: gingiva) inside the mouth. Gums surround the teeth and provide a seal around them.
Teeth:
- Both the upper and lower jaws have the teeth embedded in them.
- Human adults have 32 teeth. 16 teeth in each jaw. In humans, there are four
types of teeth—8 incisors (cuts food), 4 canines (C) (tears food), 8 premolars (PM) (grinds food) and 12 molars (M) (crushes and grinds food). - The third molar present on both sides of each jaw are together called wisdom teeth. These teeth generally grow at the age of 20-21 years.
- This set of 32 teeth is called permanent teeth. However, there is a set of 20 teeth in children. They are called milk teeth. They develop at about the age of 6 months and remain till they are 5-6 years old.
The nature of dentition and structure of teeth in humans is given below.
- Nature of dentition in human: In human 4 different types of teeth are present, hence, human has heterodont type of dentition,
- Two sets of teeth arise within a lifetime of a human, so it is called diphyodont type of dentition,
- Teeth are embedded into the jaws, so it is called the codon type of dentition.
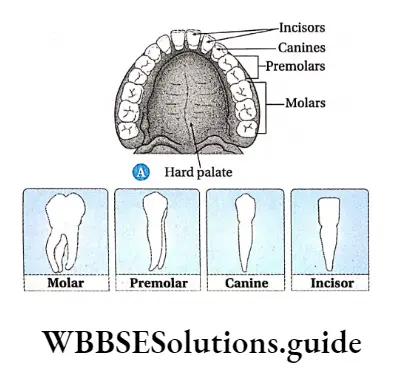
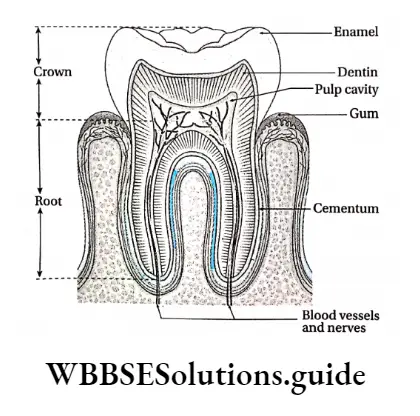
Structure of a tooth: Although the shapes of different teeth vary, they have a similar basic structure.
Its structural features are as follows—
- A tooth is formed of two parts—the exposed part or crown and the part that is embedded in the jaw bone or root.
- The crown is covered with a whitish, hard substance called enamel. It is composed of calcium salts and hydroxyapatite crystals,
- The root is formed by a mineralised matrix called dentin.
- Dentin is covered by a calcified layer called cementum. It anchors the tooth to the bone,
- The central cavity of dentine is filled with soft, gelatinous and vascular connective tissue called pulp. The cavity is called a pulp cavity,
- The portion of the pulp cavity that extends into the root is called a root canal.
Tongue: The tongue is present on the floor of the mouth.
Its structural features are as follows—
- It is a soft muscular, flattened sensory organ.
- Its anterior two-third part lies in the oral cavity which is free in movement.
- Its one-third posterior part is attached to the floor of the buccal cavity in the pharynx by a fold of the mucous membrane called the lingual frenulum.
- The oral and pharyngeal parts of the tongue are separated by a ‘V-shaped furrow, the sulcus terminalis.
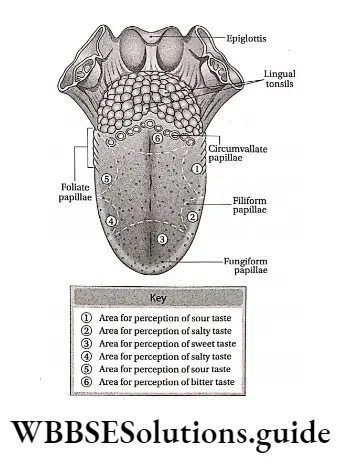
The dorsal surface of the tongue is covered with minute, round-shaped raised structures called lingual papillae.
Each papilla is surrounded by a number of taste buds. The average person has about 10,000 taste buds. Sensory receptors present within these taste buds are responsible for various tastes.
Lingual papillae are of four types—
- Circumvallate papillae are present in a V-shaped row at the posterior region of the tongue. They are 8-12 in number,
- Filiform papillae are the cone-shaped papillae that are the smallest in size. They are the most abundantly distributed at the anterior part of the tongue. They contain receptors for touch instead of taste,
- Fungiform papillae, the mushroom-shaped papillae are distributed on the tip and side of the tongue. Each papilla contains five taste buds,
- Foliate papillae are located on the posterior part of the tongue.
- The tongue has voluntary muscles, hence its movement can be controlled.
Functions: The functions of the buccal cavity—
Digestion: After ingestion, food mixes with the saliva secreted by salivary glands inside the buccal cavity. The food transforms into a soft rounded mass or bolus. The carbohydrates present in the food get metabolised by the action of the salivary enzyme, ptyalin.
Taste: The tongue which is present in the buccal cavity, helps to analyse of texture and taste (bitter, sweet, sour and salt) of the food.
Mastication and swallowing (deglutition) of food: Mechanical processing (mastication) of food occurs inside the buccal cavity with the help of teeth.
Pharynx
Pharynx is the cone-shaped musculo membranous cavity structure, leading from the mouth to the oesophagus.
Pharynx Location: It is present in the posterior region of the buccal cavity.
Pharynx Structural features:
- It is a cone-shaped, small passage where the alimentary canal and air passage cross each other. It is 12-14 cm long. It is divided into three parts.
- The upper part of the pharynx has openings of a pair of internal nares and a pair of eustachian tubes. This part of the pharynx is called the nasopharynx.
- The oropharynx lies behind the buccal cavity and acts as the passage for food bolus.
- The last part of the pharynx or laryngopharynx is connected to the larynx and the trachea (windpipe).
- An aperture called glottis in its anterior portion connects it to the trachea. The glottis is closed by a triangular flap of elastic cartilage called epiglottis. It prevents the entry of food and water into the larynx.
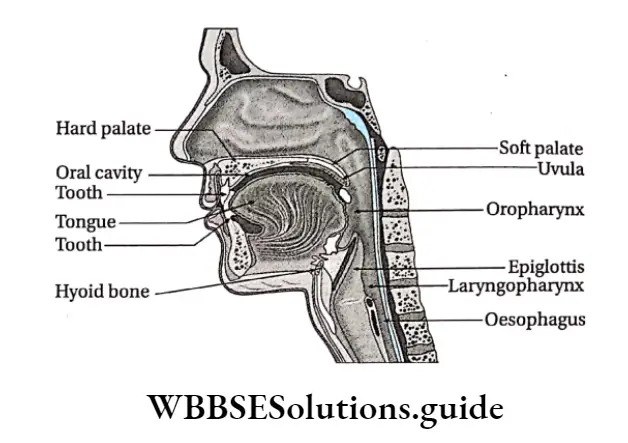
Pharynx Functions:
- The pharynx helps to transfer the food bolus from the mouth to the oesophagus (helps in Deglulition or the act of swallowing).
- The pharynx joins the nasal passage to the larynx and helps in breathing.
Oesophagus
The Oesophagus is the part of the alimentary canal that extends beyond the pharynx, upto the stomach.
Oesophagus Location: From the pharynx, it extends downwards leading to the stomach.
Oesophagus Structural features:
- The oesophagus is about 25 cm in length.
- It is a long and thin tube that enters the thoracic cavity and runs parallel to the windpipe.
- The inner lining of the oesophagus is generally smooth.
- No glands are attached to the oesophagus The oesophagus consists of four layers—the mucosa Submucosa, muscular mucosa and tunica serosa or adventitia (from inside to outwards).
Oesophagus Functions: The oesophagus helps the food bolus to travel down to the stomach, through peristalsis. No digestion of food takes place here.
Stomach
The stomach is the largest part of the alimentary system. It has a sac-like appearance. It is the part of the alimentary canal next to the oesophagus, where digestive juices and hydrochloric acid are released for further digestion of the food.
Stomach Location: It is located below the diaphragm, next to the oesophagus, with the liver on its right.
Stomach Structural features:
- The stomach is a wide, J-shaped organ.
- It is about 25 cm long, while breadth and height both is about 10 cm.
- The stomach has two curvatures. The lesser curvature makes up the right border of the stomach. It is slightly depressed. The greater curvature makes up the left border of the stomach. It is slightly elevated.
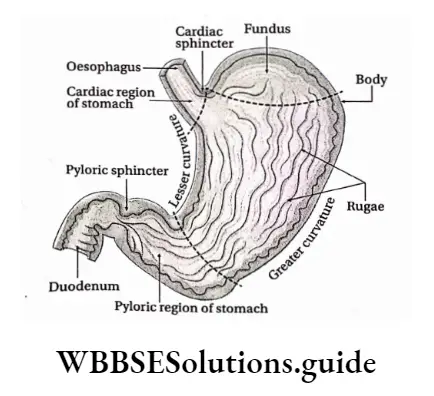
The stomach is divided into four parts—
Cardiac stomach: The part of the stomach that joins the oesophagus is called the cardiac stomach, it is called so because of its location near the heart.
Fundus: The semicircular region of the stomach, that extends a little beyond the level of the cardiac stomach, is called the fundus
Body: The part of the stomach that extends in between the fundus and the pyloric region of the stomach is called the body,
Pyloric stomach or Pylorus: The distal part of the stomach, that extends beyond the body region is called the pyloric stomach or pylorus. It is divided into two parts.
The part of the pylorus that joins the body of the stomach is called the pyloric antrum while the part which joins the duodenum is called the pyloric canal.
The stomach has two openings the cardiac orifice, through which the oesophagus opens into the stomach and the pyloric orifice, through which the stomach opens into the duodenum.
The sphincter muscle present at the junction of the oesophagus and the stomach i.e. at the cardiac orifice, is called the cardiac sphincter.
Digestion And Absorption Of Nutrients
The pyloric orifice is surrounded by a well-defined muscular sphincter, called the pyloric sphincter. It controls the movement of food out of the stomach but prevents reflux of duodenal contents into the stomach.
The stomach wall consists of mucosa, submucosa, muscular and serosa (serous) layers. The inner surface of the stomach, mainly the mucosal region, is thrown into longitudinal folds called rugae. These folds appear only when the stomach is empty.
The inner lining of the stomach has numerous microscopic glands called gastric glands which are present in groups of 2-7, which together link with the gastric lumen through the gastric pits.
Cardiac stomach Functions: The stomach performs the following functions in the human body.
- Digestion: Major enzymatic digestion is initiated in the stomach, particularly that of proteins. The gastric glands secrete digestive juices. Different enzymes are present in these digestive juices that help to digest fats and proteins. HCI creates an acidic environment within the stomach. This allows the enzymes to work properly. The stomach is responsible for the formation of chyme, which is a semi-fluid mass of partly digested food.
- Storage: The stomach acts as a storage for food until it moves into the duodenum.
- Mechanical breakdown: The vigorous contractions of smooth muscles present in the stomach help to grind food materials into smaller bits and also to mix with gastric secretions.
- Absorptive function: Small amounts of salts, water Alcohol, medicine etc get absorbed in the stomach.
- Other secretions: The stomach secretes a substance called Castle’s intrinsic factor. It is required for the absorption of vitamin B12 in the small intestine. Moreover, gastrin hormone is secreted by G cells and stimulates the glands to secrete the digestive juices.
- Protection: HCI released by the oxyntic cells can kill the microbes that enter our body along with food and provide protection against them.
Production of HCI in the stomach
CO2 present in the interstitial fluid diffuses into the parietal cells of the stomach and reacts with water to form carbonic acid (H2CO3).
This reaction is facilitated by carbonic anhydrase. This H2CO3 dissociates into H+ and HCO-3. H+ ions enter the lumen of digestive glands.
Chloride ions already present in the interstitial fluid, enter the digestive glands via the parietal cells. H+ and Cl– react to form HCI.
Small Intestine
The long, narrow and coiled part of the alimentary system that starts just below the stomach, where both digestion and absorption take place, is called the small intestine.
Cardiac stomach Location: It extends from the pyloric valve of the stomach to the large intestine.
Cardiac stomach Structural features:
- The small intestine is a narrow and extended tube-like structure. It has a length of slightly more than 5m and a diameter ranging between 3.5-4.5 cm.
- The walls of the small intestine are made up of four layers, from inside to outwards—mucosa, submucosa, muscularis externa and serosa.
- The entire mucosa layer is lined with numerous, densely packed finger-like extensions called villi.
- The submucosa layer contains Brunner’s glands at the duodenum. It secretes a slimy alkaline substance which neutralises the acidity of the chyme.
- Numerous circular or oblique folds (or folds of kicking) called plicae circulares line the inner wall of the small intestine.
- At the bases of villi, glandular areas called crypts of Lieberkuhn, are present. These contain mucus and hormone-secreting cells.
- It has the following regions—
- Duodenum: It is part of the small intestine. It forms a C-shaped arch with the stomach. Its length is around 25 cm. Its lateral walls have a slightly swollen region called the ampulla of Vater.
- The hepatopancreatic duct (the common duct formed by the pancreatic duct and bile duct) enters the duodenum through this ampulla- The internal wam contains circus folds and villi,
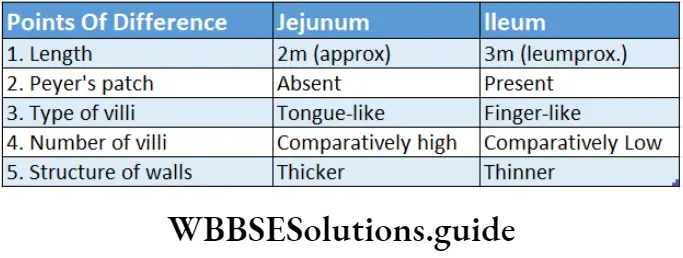
- Jejunum: It is the coiled, middle region of the small intestine. It is about 2 m long. The inner wall is thicker and contains more folds and villi than the duodenum. Glands are absent in this region.
- Ileum: It is the last part of the small intestine. It is about 3 m long. It remains in a coiled condition within the abdominal cavity. The inner wall ileum contains a lesser number of plicae and villi than the jejunum.
Small masses of lymphatic tissues called Peyer’s patches are found on the ileum wall. These tissues produce lymphocytes which prevent infection. It joins with the colon region of the large intestine.
At its junction with the colon, a valve called the ileocecal valve is present. It allows the undigested parts of the food to enter the colon but prevents the reverse.
NEET digestion and absorption revision notes with MCQs
Villi
- Villi Location: The mucosa of the small intestine.
- Villi Structure:
- A mucous layer of the small intestine folds into small finger-like projections called villi.
- Each villi is about 0.5-1 mm long and has an outermost layer of columnar epithelial cells called enterocytes. The free surface of these cells has numerous 1 pm long microvilli and form a brush-like appearance. This is called border structure,
- At the base of the villi crypts of Lieberkuhn are present which contains endocrine cells. These cells secrete intestinal juice.
- Each villus has a central lacteal,
- Several blood capillaries form a network around lacteal. The veins present at the ends of these capillaries join to form the hepatic portal vein.
- Villi Function: The villi as well as the microvilli increase the surface area for absorption in the small intestine.
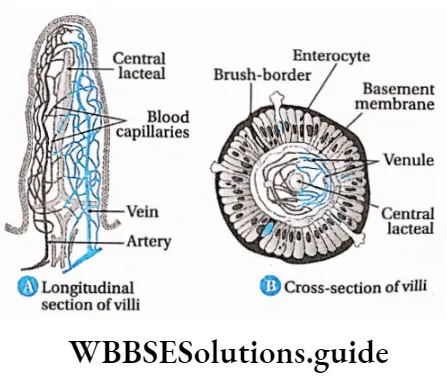
Villi Functions: Functions of the small intestine are—
Digestion
- The small intestine receives bile from the liver. Bile does not contain enzymes. It contains salts like sodium glycolate and sodium taurocholate, which emulsifies fat causing fat droplets to disperse in water.
- It also receives pancreatic juice from the pancreas and intestinal juice from intestinal glands. Both of these juices contain enzymes necessary for the digestion of proteins, carbohydrates and fats.
Absorption: The small intestine is the site for the absorption of nutrients. The circular folds, villi, and microvilli increase the surface area for absorption.
Segmentation and peristalsis: The wall of the small intestine shows two types of movements—segmentation and peristalsis. Segmentation causes small and regular, localised contractions that bring chyme in contact with digestive juices. Peristalsis of the small intestine allows undigested food to move to the large intestine.
Protection: The germs that have survived the effect of HCI in the stomach get killed by the lymphocytes produced at the lymph nodes in the small intestine.
Hormonal secretion: Hormones like cholecystokinin (CCK) and secretin are secreted within the small intestine.
Large intestine
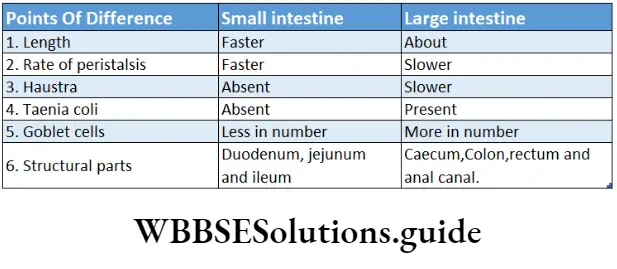
The large intestine is the part of the alimentary tube, present between the small intestine and the anus, where the undigested food remains stored for some time.
Location: The large intestine lies next to the ileum, in the abdominal cavity.
Structural features: The diameter of the large intestine is 6.5 cm and its length is about 1.5 m. The inner wall contains some semilunar folds. These are called plicae semilunaris.
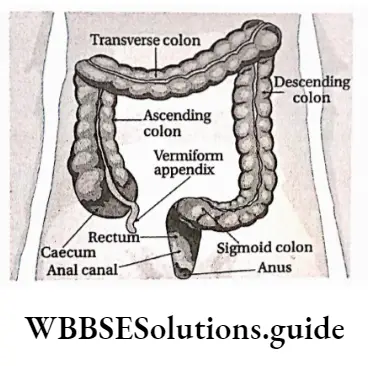
The large intestine is divided into the following parts—
Caecum: It is a small sac-like structure present below the junction of the small intestine with the large intestine.
The caecum has a small (about 8-9 cm length) finger-like blind tube called the vermiform appendix at its lower end. Infection of the vermiform appendix is known as appendicitis. In human beings, it is a vestigial organ.
Colon: It is a wide tube-like structure present between the caecum and rectum. The wall of the colon has longitudinal muscles that form three separate bands called taenia coli.
Contraction of these muscles produces a series of bulges or pouches called the haustra, in the colon. The colon is divided into four parts—ascending, transverse, descending and sigmoid colon.
Rectum: It is the enlarged structure at which the sigmoid colon opens. It is about 13 cm in length.
Anal canal and anus: The rectum opens into a short canal-like structure called the anal canal. It is generally 3.8 cm long. This canal opens outside by an orifice called the anus. Anus is guarded by two sphincter muscles called anal sphincter.
Functions: The large intestine performs the following function in human beings.
Production of faecal matter: The faeces are formed by the action of the different bacteria present in the colon region of the large intestine.
Absorption: In the large intestine, Na+, Cl– and H2O are absorbed from the undigested food matter. Some vitamins and medicines also get absorbed in this region.
Mucus secretion: The goblet cells present in the large intestine secrete mucus. The mucus softens the faecal mass and makes it slippery.
Storage of faecal matter: The faecal mass is stored in the rectum for some time before egestion.
Egestion of faecal matter: The faecal matter is removed from the body through the anus.
Digestive Glands
Digestive glands Definition: The glands related to the digestive system which secrete digestive juices containing enzymes that convert complex food substances into simpler absorbable forms are called digestive glands.
Digestive glands Types: Digestive glands in humans include salivary glands, gastric glands, intestinal glands, liver and pancreas. The different types of digestive glands, along with their secretions are discussed below.
Salivary glands
The salivary glands are present in the buccal cavity. They secrete saliva. Enzymes present in it help to break down the carbohydrate-rich food.
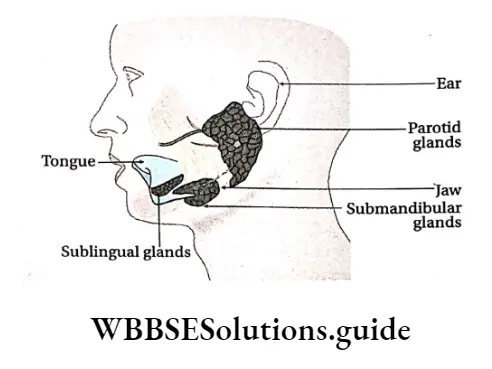
Salivary glands Types: Salivary glands are of three types—parotid, submandibular and sublingual glands.
Parotid gland: The paired parotid glands are the largest of the salivary glands and weigh about 15-30 g.
They are present just below the ears. They open inside the mouth, at the root of the second molar on both sides of the upper jaw, through Stensen’s ducts.
Mumps
- Mumps is a viral disease that affects salivary glands, mainly parotid glands. Children at the age of 5-9 years are more vulnerable to this disease.
- If mumps occurs after adolescence, then it may lead to infection in the testes. This may further lead to sterility. Sometimes pancreas may also get affected by the mumps virus. This is the risk of diabetes mellitus in the patient.
Submandibular gland: The submandibular or submaxillary gland is the second largest salivary gland. It weighs about 7-16 g. The gland is located at the angle of the lower jaw, at the junction of the lower and upper jaws. The duct, by which each submaxillary gland opens into the mouth, is called Wharton’s duct.
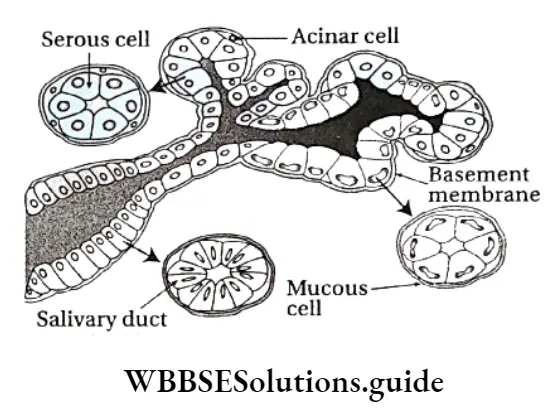
Sublingual gland: The smallest of the salivary glands is the sublingual gland, weighing about 2-4 g. It is located below the tongue. It opens into the mouth through several fine ducts called ducts of Rivinus. Structure: The anatomical and histological structures of the salivary glands are discussed below.
Anatomical structure:
- The salivary glands are divided into several lobes. The lobes are separated by interlobular septum.
- Each lobe is further divided into numerous acini (singular: acinus) or alveoli (singular: alveolus).
- Each acinus or alveolus has an outer membrane. The inner surface of the membranes has glandular cells.
- The central portion of the acinus is empty, where the secretions are stored. The ducts that arise from these cavities join to form the salivary duct.
Histological structure:
- Histologically, the salivary glands are made up of two types of cells—
- Serous cells and
- Mucous cells.
- The parotid glands are composed primarily of serous cells. The sublingual glands contain mainly mucous cells. On the other hand, the submandibular glands contain both serous and mucous cells, hence they are called mixed types of glands.
- Mucous cells release a thick secretion called mucus.
A few star-shaped contractile cells are situated in between the basement membrane and the secretory cells called myoepithelial cells which help in the expulsion of saliva from the gland.
Mumps Function: The function of the salivary glands is to secrete saliva.
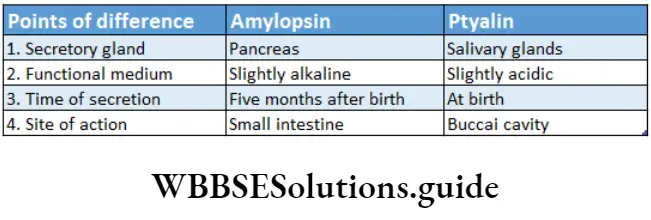
Saliva: The colourless, watery fluid secreted by the salivary glands, that contains mainly a starch-digesting enzyme called ptyalin (salivary amylase) in the buccal cavity is called saliva.
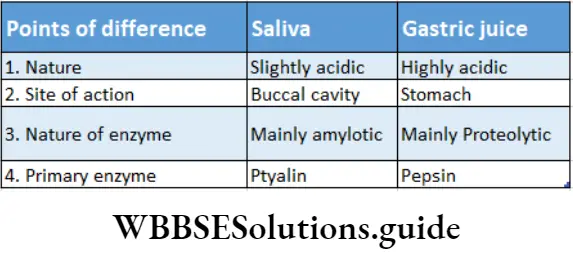
Characteristics and components: Saliva is a colourless and viscous liquid. The saliva maintains a slightly acidic pH ranging from 6.0 to 7.0. The Components of Saliva Are listed.
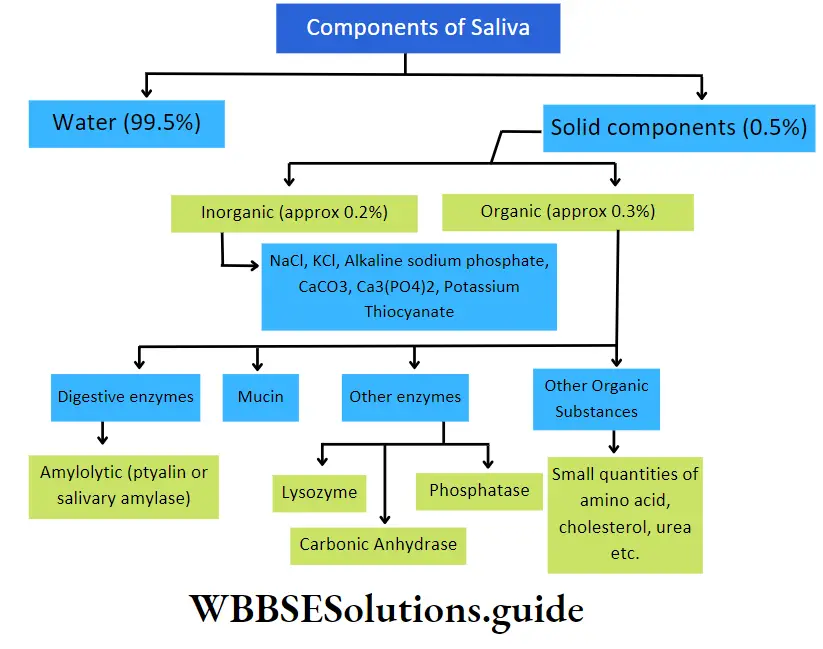
Other Components Of Saliva
- Cellular components: Saliva contains yeast cells, bacteria, parasites, protozoa, polymorphonuclear leucocytes (granulocytes), etc., as their cellular components.
- Gaseous components: Every 100 ml of human saliva contains 1 ml oxygen, 2.5 ml nitrogen and 50 ml CO2 in dissolved condition.
- Function: Saliva plays an important role in the digestion of food. it also has some other functions.
Role in digestion:
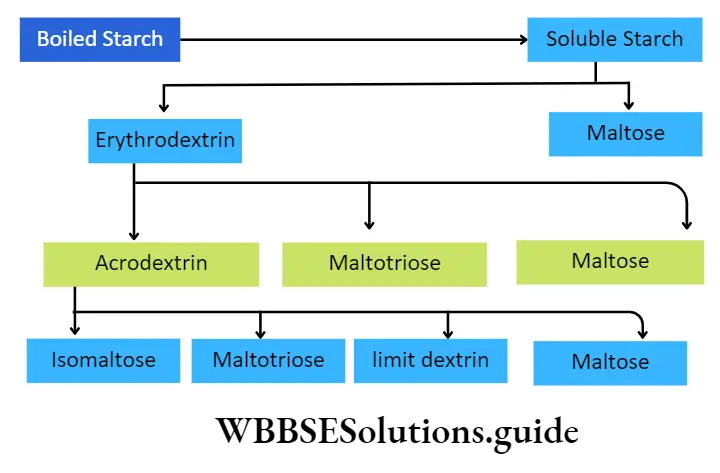
Saliva contains the enzyme ptyalin which acts in a slightly acidic medium, in the presence of chloride ions. It breaks down boiled starch, glycogen, etc., into maltose, maltotriose, limited dextrin and isomaltose,
The water present in the saliva helps to break down the protein molecules present in the food.
Non-specific immunity: Human saliva contains an enzyme called lysozyme. This enzyme helps to break down the polysaccharide units of the cell walls of bacteria like Streptococcus spv Staphylococcus sp., etc., that enter the mouth via food. This kills these bacteria and provides protection.
Role in excretion: Saliva acts as a medium to release urea, heavy metals,(Hg, Pb, Bi, As, etc.), isocyanate, excess antibiotics, etc., from the body.
Helps to taste: Saliva aids in moistening dry food. This enables us to feel its taste.
Mechanical and other functions:
- Saliva contains a glycoprotein, called mucin. It mixes with the food and makes it slippery so that swallowing becomes easier,
- It lubricates the mouth and helps in speaking,
- It softens the food and makes chewing easier,
- Saliva has a high concentration of bicarbonate ions. It acts as a buffer and protects the mucous layer inside the oral cavity and teeth from the acids produced by the microbes.
Gastric Glands
Gastric glands are the small tubular glands, present on the mucous layer of the stomach. They secrete digestive enzymes.
Types: Gastric glands are of three types—
- Cardiac gastric glands are located in the proximal part of the stomach,
- Fundic or intermediate gastric glands in the central stomach areas and
- Pyloric gastric glands in the terminal stomach portion.
- Secrete mucus that protects the stomach lining from the digestive action of gastric juice.
- Gastrin cells, also called G cells secrete a hormone, gastrin.
Gastric glands Function:
- Gastric glands secrete gastric juices that help to break down the food and digest it.
- The mucus secreted by these glands helps to protect the tissues of the stomach from the digestive juices.
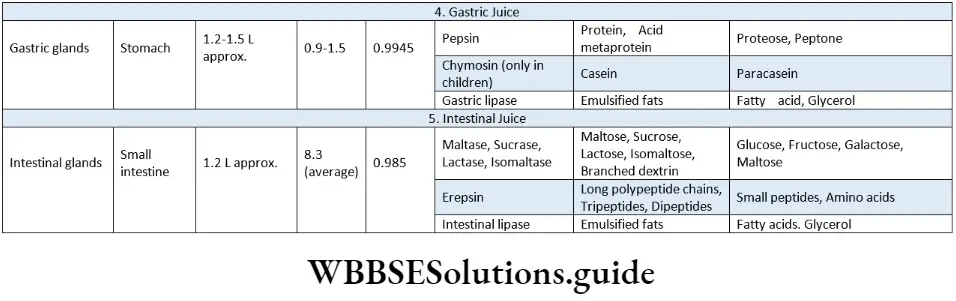
Gastric juice: The highly acidic fluid, secreted by the gastric glands, that contains digestive enzymes is called digestive juice or gastric juice.
Gastric glands Characteristics and components: The pH of gastric juice is low, ranging from 0.7 to 3.8. About 1200-1500 ml of gastric juice is produced every day. Around 500- 1000 ml is secreted after every meal. The composition of gastric juice is given in the following chart.
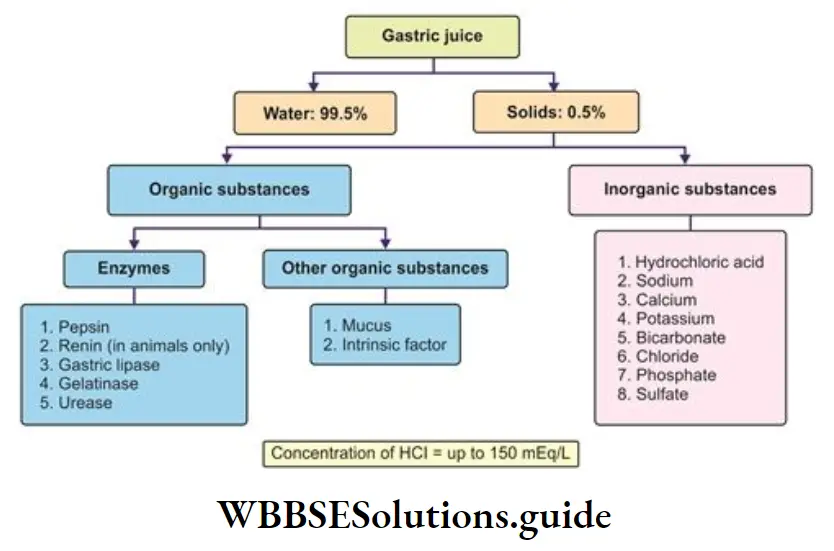
Gastric glands Function: The different components of gastric juice have the following functions—
Role of HCI:
- HCI found in gastric juice converts inactive pepsinogen, and prorennin into their active forms.
- It provides an environment with the optimal pH required for the action of pepsin,
- It converts some of the ingested proteins into acid metaproteins,
- It kills the bacteria that have entered the food.
- It also helps in hydrolysis of sucrose.
Role of mucin:
- Mucin produced by the gastric glands forms a protective barrier on the inner lining of the stomach. It prevents the HCI from damaging the cells of the stomach,
- It acts as a buffer and lowers the acidity of the stomach.
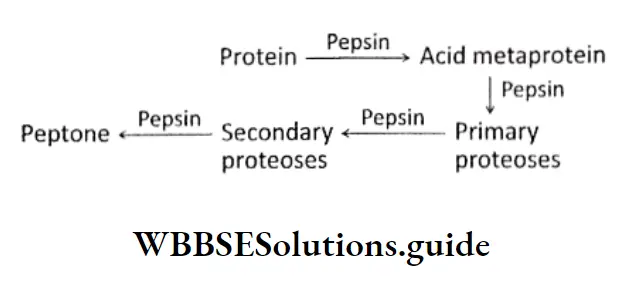
Role of pepsin: Pepsin is a protease, that is the principal enzyme in gastric juice. The precursor, pepsinogen, is converted to the enzyme pepsin when exposed to HCI. This pepsin now hydrolyses proteins, acid metaproteins, etc., into proteoses and peptones.
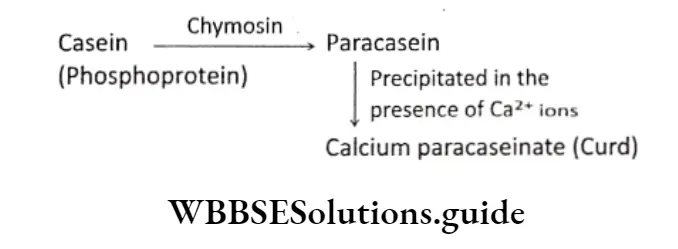
Role of chymosin: This enzyme also known as rennin is absent in the gastric juice of adults. In children, this enzyme converts milk protein, casein into paracasein, under an acidic medium.
Role of Castle’s intrinsic factor: Castle’s intrinsic factor, present in the gastric juice, helps in the absorption of vitamin B12, in the intestinal lumen. Its absence decreases vitamin B12 absorption.
Role of gastric lipase: Gastric lipase is a fat hydrolysing enzyme. It acts on emulsified fats and hydrolyses them into fatty acids and glycerol.
Role of other enzymes:
Other enzymes present in the gastric juice include—
- Lysozyme kills bacteria by breaking the polysaccharide layer of their cell membrane,
- Urease hydrolyses urea into ammonia,
- Carbonic anhydrase stimulates the oxyntic cells of the stomach to synthesise HCI.
- Gelatinase breaks down gelatin into peptones.
Liver
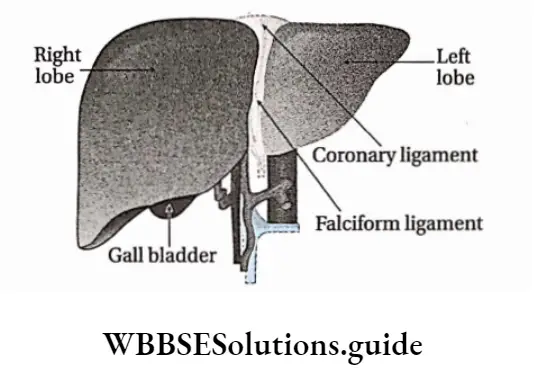
The largest gland of the body, normally weighing about 1.5 kg, which takes part in digestion and excretion is called the liver. it is present in the upper part of the abdominal cavity, just below the diaphragm, on the right side of the body.
Structure: The anatomical and histological structures of the liver are discussed below.
Anatomical structure:
- The liver is the largest gland (exocrine) in the body.
- It is reddish-brown in colour.
- It has a larger right lobe and a smaller left lobe, separated by a ligament.
- The ligament is called the falciform ligament. It is continuous with the peritoneum.
- The lower part of the liver is further divided into two lobes—quadrate lobe and caudate lobe by transverse fissures.
- The liver is covered by a connective tissue layer, called Glisson’s capsule.
- The lower part of the right lobe has a slightly depressed region, called cystic fossa. It contains a thin-walled, pyriform (pear-shaped) sac-like structure called a gall bladder.
- The duct arising from the gall bladder is called the cystic duct. Two ducts arising from the two lobes of the liver join to form the common hepatic duct.
- When the common hepatic duct joins the cystic duct, it forms the common bile duct.
- The common bile duct joins the pancreatic duct and opens into the duodenum at the ampulla of Vater.
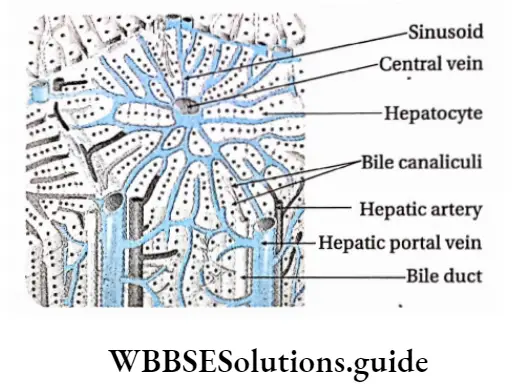
Liver Histological Structure:
- A capsule made of connective tissue surrounds the liver. This capsule invaginate the liver to divide it into numerous hepatic lobules.
- Lobules of the liver are polygonal in shape. They are separated from each other by connective tissue. Each lobule is made up of hepatocytes (hepatic cells).
- Hepatocytes are arranged as plates (hepatic plates) of one cell thickness with vascular channels (sinusoids) on either side. These plates remain surrounding a central vein like the spokes of a bicycle wheel.
- The hepatic artery, hepatic portal vein and a branch of the bile duct are present in the connective tissue, within the liver. Liver Together, they are called the hepatic or portal triad.
- Hepatocytes secrete a fluid called bile into a network of narrow channels between the opposing membranes Of adjacent liver cells. These passageways are called bile canaliculi.
- Large phagocytic cells known as Kupffer cells or Stellate cells are attached to the inner lining of hepatic sinusoids. They act as macrophages. They remove pathogens and debris that may have entered the sinusoids.
- Small spaces called perisinusoidal spaces (also known as the space of Disse) are present in between a hepatocyte and a sinusoid. Transport of proteins and other plasma components from sinusoids to hepatocytes occurs through these spaces.
Liver Function: Functions of the liver in humans are given below.
- Secretion: It produces bile, which remains stored within the gall bladder before entering the bile duct.
- Storage: It stores iron (Fe2+) and fat-soluble vitamins such as vitamins A, D, E, and K. Some quantities of fat also remain stored within the liver.
- Metabolism: The liver takes part in the metabolism of carbohydrates, proteins and lipids.
Carbohydrate metabolism: It helps in carbohydrate metabolism and maintains the concentration of glucose in the blood.
It converts glucose to glycogen by glycogenesis (under the influence of the hormone insulin). It converts glycogen into glucose by glycogenolysis (under the influence of the hormone glucagon). The liver also converts fats and proteins into carbohydrates by gluconeogenesis, when required.
Fat metabolism: The liver helps in the oxidation of fats, production of ketones, and synthesis of fats from carbohydrates and proteins. It also helps in the synthesis of phospholipids. It can also regulate the blood cholesterol level by converting some of them to bile acids. These bile acids form bile salts, which help in emulsification of fats.
Protein metabolism: It produces plasma proteins, It also synthesises urea (by ornithine cycle) and uric acid by deamination of amino acids.
Transamination: Synthesis of new amino acids by transfer of amino group from an amino acid to another compound takes place in the liver.
- Role in excretion: The liver acts as an accessory excretory organ. Ammonia produced due deamination of proteins is converted into urea in the liver. It also detoxifies blood by metabolising and eliminating poisonous substances such as toxins, metals, bacteria, etc., from the body. It also excretes bilirubin, produced by the breakdown of haemoglobin.
- Role in synthesis: The liver synthesises plasma proteins, such as prothrombin, fibrinogen, etc., from amino acids. Synthesis of anti-coagulation factor, heparin, takes place within the hepatic cells
- Immunity: It plays an important role in the immunity of the body. Kupffer cells, present in the sinusoids, engulf the bacteria that enter the liver. The liver also produces antibodies that help in the development of the immune system.
- Regulation of body temperature: The metabolic reactions taking place in the liver produce heat, that helps in the regulation of body temperature.
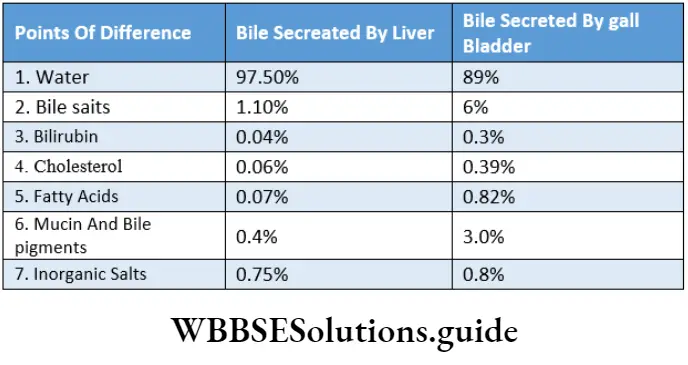
- Bile: It is the greenish-yellow (in the case of humans)coloured, non-enzymatic digestive juice secreted by the 1 hepatocytes of the liver. It enables the breakdown and absorption of fats.
- Characteristics and components: Bile is generally greenish-yellow in colour. It is alkaline in nature, with a pH of about 7.7. Sometimes, the alkalinity is slightly less (pH ranging between 7.0-7.6). An average of 500-1000 ml of bile is produced every day. The components of bile are described in the following chart
- Function: Bile take part in different functions in the human body
1. Role in digestion:
- Bile salts help in the emulsification of fats, i.e., break down fat into small droplets. It increases the surface area for the enzyme lipase to act on. Lipase breaks down the fat droplets into fatty acids and glycerol,
- Bile also contains glycocholic acid and taurocholic acid that stimulate the action of the enzyme lipase,
- Bile also acts as a medium for the reaction between fats and lipase enzymes.
2. Role in absorption:
- Bile also enhances the absorption of fats (digested or undigested), fatty acids, metal ions such as Na+, K+, Ca2+ and the fat-soluble vitamins A, D, E, and K.
3. Role in excretion:
- Bile also serves as the route of excretion for heavy metals such as Znz+ Cu, etc., bile helps in the regulation of body temperature. pigments, toxins, bacteria, cholesterol and lecithin, etc..
4. Choleretic Action:
- Bile contains bile salts that are coloured, non-enzymatic digestive juice secreted by the 1 hepatocytes of the liver. It enables the breakdown and absorption of fats.
5. Laxative action:
- Bile salts act as natural laxatives by stimulating peristaltic movements of the intestine.
6. Role as a lubricant:
- Mucin present in bile, acts as both a lubricant and a buffer.
7. Neutralisation of stomach acid:
- The sodium carbonate present in bile neutralises any excess stomach acid before the chyme enters the ileum. Besides these, bile salts also act as bactericides. They can destroy many microbes present in the food.
Pancreas
The pancreas is the organ that is present below the stomach, in j the abdominal cavity. It has both exocrine (ductal) and j endocrine (ductless) functions.
Pancreas Structure: The pancreas is a slightly pink-coloured light organ. Its length is around 12-15 cm and it weighs around 60 g. It is a slightly flattened and stretched structure.
Its ends are slightly edged. Its narrow end is free, while its broad end has a duct arising from it, called the pancreatic duct. This duct joins the ampulla of Vater, present in the duodenum.
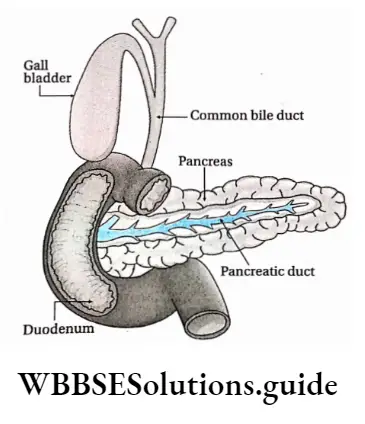
Pancreas is a mixed gland. Its exocrine and endocrine functions are discussed below
Exocrine region of the pancreas:
- The exocrine region I of the pancreas is composed of numerous small, sac-like I structures called acini. They are covered by membranes.
- Each acinus is composed of a single layer of pyramidal glandular cells. These cells are arranged in groups around a central lumen, from which several ducts (ducts of acini) arise.
- These acinar ducts together form a duct of Wirsung or the pancreatic duct. The pancreatic duct, in turn, joins the common bile duct and enters the duodenum at the ampulla of Vater.
- An accessory pancreatic duct called the duct of Santorini is found in some individuals. It rises from the main pancreatic duct and opens in the duodenum just above the common bile duct.
- The blood flow through the ampulla of Vater is regulated by a sphincter muscle called hepato-pancreatic sphincter (sphincter of Oddi).
- The enzyme-containing granules present in the exocrine region are called zymogen granules.
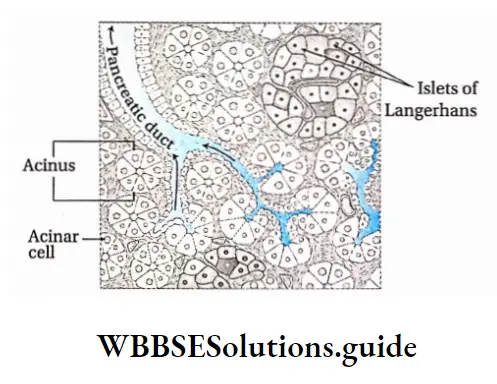
Endocrine region of the pancreas:
- The endocrine cells are arranged in groups, which are interspersed among the acini. These groups are called islets of Langerhans (named after the discoverer scientist P. Langerhans).
- There are five types of endocrine cells found in islets—alpha-beta, delta, epsilon and P-P cells.
- Different hormones (from a, (3, 5, e cells) and pancreatic polypeptide (P-P cells) are secreted by this region. The islets are surrounded by networks of blood capillaries.
- The hormones, that are secreted, enter the blood capillaries and get transported to the target organs.
The pancreas is one of the main digestive glands in humans. It performs the following functions.
- Digestive juice secretion: The enzymes, secreted by the exocrine region of the pancreas, break down. carbohydrates, fats, proteins, and acids in the duodenum.
- Secretion of bicarbonate ions: The exocrine tissue also secretes bicarbonate ions that neutralise the stomach acid in the duodenum.
- Hormone secretion: Insulin, glucagon, and gastrin hormones are secreted by the endocrine region of the pancreas. P-P cells secrete pancreatic polypeptides that regulate the secretory activity of pancreatic cells carbohydrates, fats, proteins, and acids in the duodenum.
- Secretion of bicarbonate ions: The exocrine tissue also secretes bicarbonate ions that neutralise the stomach acid in the duodenum.
- Hormone secretion: Insulin, glucagon, and gastrin hormones are secreted by the endocrine region of the pancreas. P-P cells secrete pancreatic polypeptides that regulate the secretory activity of pancreatic cells.
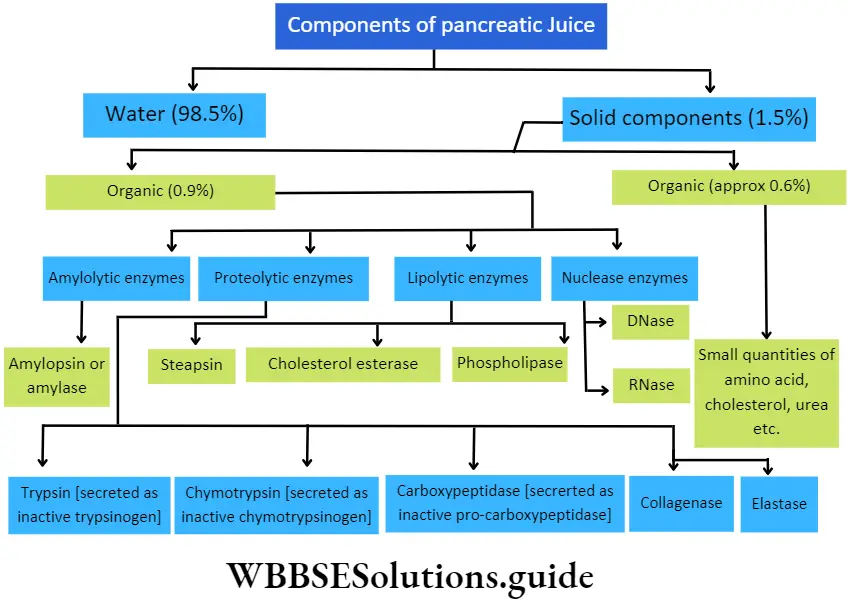
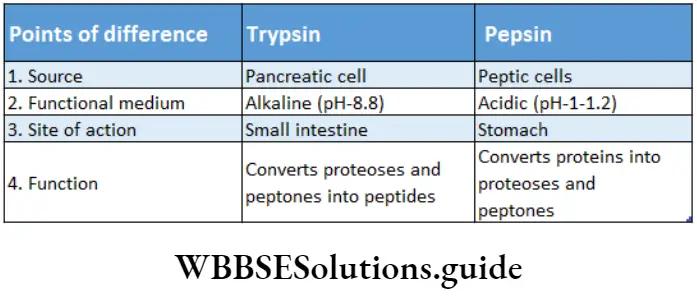
Function: The digestive functions of the pancreatic juice are given below.
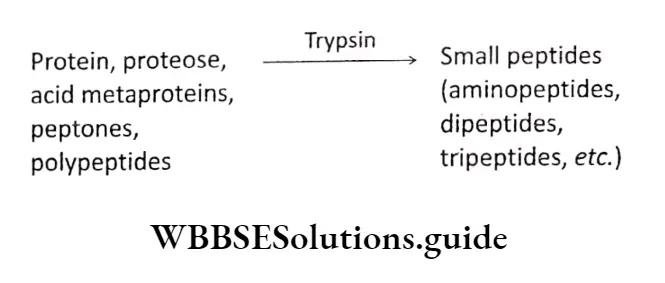
- Activation of trypsin and its role: Inactive trypsinogen present in the pancreatic juice gets activated into trypsin, under the influence of enzymes like enteropeptidase or enterokinase.
- Trypsin hydrolyses proteins, acid metaproteins and peptones into polypeptides and amino acids.
- Trypsin activates chymotrypsinogen.
- Activation of chymotrypsin and its role: Inactive chymotrypsinogen present in pancreatic juice gets activated into chymotrypsin, by trypsin. Chymotrypsin helps to convert milk protein, casein, into paracasein which on reacting with Ca2+, precipitates calcium para caseinate as curd, It also helps in hydrolysing other proteins into polypeptides.
- Activation of carboxypeptidase and its role: Inactive procarboxypeptidase present in the pancreatic juice, gets converted into active carboxypeptidase, by the action of trypsin, in the duodenum. Carboxypeptidase hydrolyses long polypeptide chains into shorter ones and releases terminal amino acids from the peptide, within the cavity of the small intestine.
- Activation of elastase and its role: Inactive proenzyme, proelastase is present in the pancreatic juice. It gets activated by trypsin, to form elastase enzyme. Elastin protein present in yellow fibres (found in connective tissue matrix) gets hydrolysed by this enzyme to form amino acids.
- Role of collagenase: Collagenase is a proteolytic enzyme present in the pancreatic juice. It hydrolyses the fibrous protein collagen into amino acids under a slightly alkaline medium.
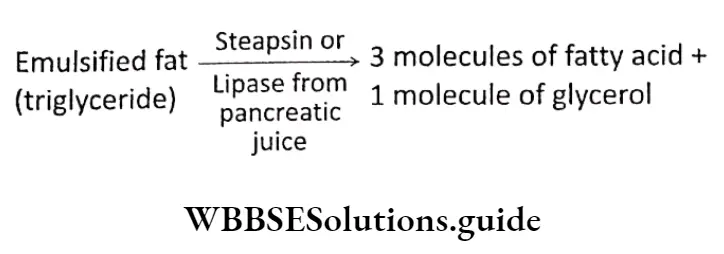
- Role of steapsin: Lipase or steapsin present in the pancreatic juice, hydrolyses emulsified fats into fatty acids and glycerol. 1 molecule of triglyceride gets hydrolysed into 3 molecules of fatty acids and 1 molecule of glycerol.
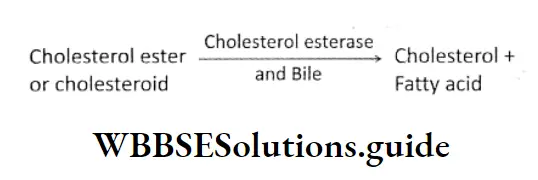
- Role of cholesterol esterase: Cholesterol esterase present in the pancreatic juice, hydrolyses cholesterol ester into cholesterol and fatty acids, under the influence of bile. It may catalyse the esterification of cholesterol esters with free fatty acids.
- Role of phospholipase: Phospholipase present in the pancreatic juice, hydrolyses phospholipids into lipophospholipids and fatty acids.
- Role of nuclease: Dnase and RNase present in I pancreatic juice, hydrolyse DNA and RNA j respectively, into specific nucleotides.
- Role of amylase: Pancreatic juice contains an amylolytic enzyme called pancreatic amylase or amylopsin which converts different polysaccharides (glycogen, starch, etc.) into maltose.
Intestinal Glands
Intestinal glands are the small glands present on the inner epithelium of the small intestine. It secretes enzyme-containing intestinal juice.
Intestinal glands Structure: I small intestine. At the base of the mucosal villi, numerous microscopic intestinal glands are present.
These are called Lieberkiihn’s glands(crypts of Lieberkuhn). These glands are tubular and unbranched and secrete enzymes and mucus.
The submucosa layer of the duodenum has another type of gland called Brunner’s glands. These glands are branched and secrete alkaline watery fluid, enzymes and mucus.
They open into the crypts of Lieberkuhn. The mixture of secretion of these two glands is known as intestinal juice or succus enteric.
Process of digestion and absorption of carbohydrates, proteins, and fats
Intestinal glands Function: The main function of the intestinal glands is the secretion of intestinal juice and mucus.
Intestinal juice or succus entericus: The secretion of intestinal glands, that contains several digestive enzymes is called intestinal juice or succus entericus.
Characteristics and components: Intestinal juice is alkaline in nature. Its average pH is 8.3. An average of 1-2L of intestinal juice is produced every day. The composition of the intestinal juice.
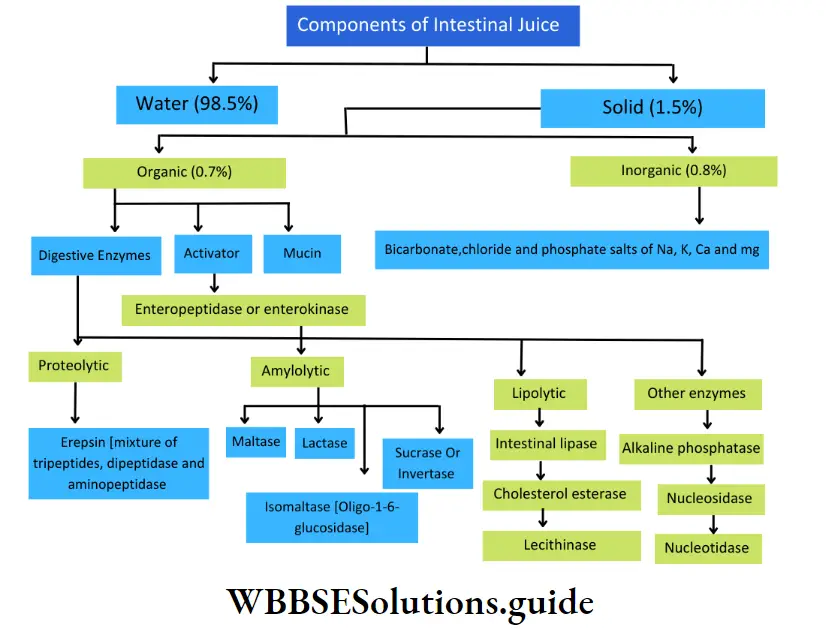
Intestinal glands Function: The functions of the components of intestinal juice are as follows.
- Role of enteropeptidase or enterokinase: Enterokinase, secreted by the intestinal glands into the intestinal juice, activates trypsinogen into trypsin, This enzyme, trypsin, further activates other enzymes.
- Role of erepsin: Erepsin present in the intestinal juice is a mixed enzyme. It is a mixture of aminopeptidase, tripeptidase and dipeptidase. Their functions are as follows—
- Aminopeptidase: It hydrolyses long chains of polypeptides into smaller polypeptides (such as tripeptides and dipeptides),
- Tripeptidase: It hydrolyses specific tripeptides into dipeptides and amino acids,
- Dipeptidase: It hydrolyses specific dipeptides into amino acids.
- Role of amylolytic enzymes: Amylolytic enzymes act on starch and related oligosaccharides and polysaccharides. The most known amylolytic enzymes are or-amylase, amylase and glucoamylase.
The activity of the amylolytic enzymes I are as follows—
Maltase: It hydrolyses maltose into 2 molecules of glucose,
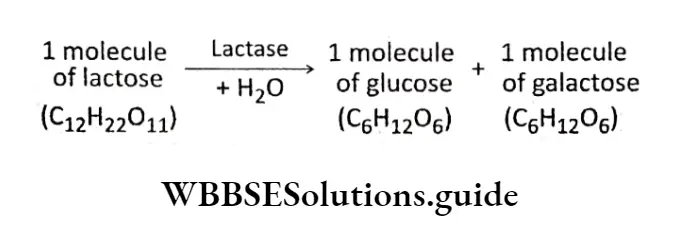
Lactase: It hydrolyses the milk sugar, and lactose into 1 molecule of glucose and 1 molecule of galactose,
Invertase or sucrase: It hydrolyses sucrose/into 1 molecule of | glucose and 1 molecule of fructose,
Isomaltase or oligo-l,6-glucosidase: It hydrolyses isomaltose and branched dextrin into maltose and glucose. It breaks the a-1,6 linkage in dextrin.
Role of lipase: It hydrolyses emulsified fats within the lumen of the small intestine, into fatty acids and glycerol. 1 molecule of triglyceride on complete hydrolysis produces 3 molecules of fatty acids and 1 molecule of glycerol.
Role of lecithinase: Lecithinase removes the fatty acid residue from lecithin. It hydrolyses a phospholipid, lecithin, present within the lumen of the small intestine into fatty acids, glycerol, choline and inorganic phosphate.
Role of nucleotidase and nucleosidase: Nucleotidase (DNase and RNase), hydrolyses nucleotide units of DNA and RNA respectively, into nucleosides. Nucleosidase hydrolyses nucleoside units of DNA and RNA, which leads to the release of basic or nitrogenous components of the chain.
Role of mucin: Mucin proteins are known for providing protection and lubrication to epithelial surfaces of the intestine.
Role of cholesterol esterase: It releases cholesterol from fat-containing food.
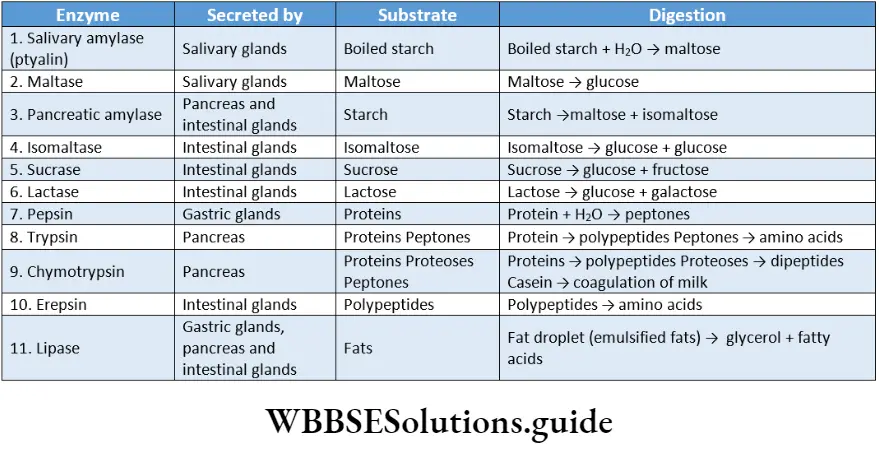
Role Of Digestive Enzymes And Gastrointestinal Hormones In Digestion
Several digestive enzymes and gastrointestinal hormones are secreted by the different glands. Let us study them and their role in digestion in detail
Digestive Enzymes
Digestive Enzymes Definition: The enzymes that act on the complex food substances in the digestive tract and convert them into simple absorbable forms are called digestive enzymes.
Different digestive enzymes and their roles
Different types of digestive enzymes are—
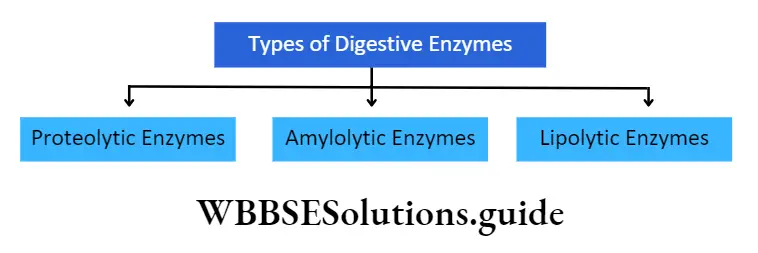
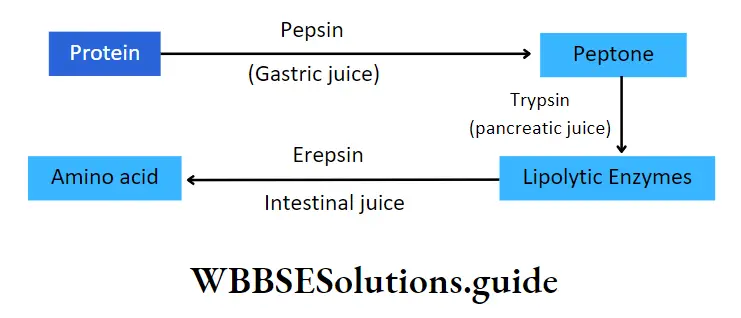
Proteolytic enzymes: The enzymes that hydrolyse the protein molecules present in the food are called proteolytic enzymes or proteases.
Role in digestion: Proteolytic enzymes gradually hydrolyse protein molecules into amino acids, which are absorbed by the cells.
⇒ \(\text { Proteins } \stackrel{\text { Proteolytic enzymes }}{\longrightarrow} \text { Amino acids }\)
Examples: Pepsin, trypsin and erepsin.
Amylolytic enzymes: The enzymes that degrade or hydrolyse complex carbohydrates present in the food, into simpler products are called amylolytic enzymes.
Role in digestion: Amylolytic enzymes facilitate the breakdown of complex carbohydrates such as fibres starches and sugars into simple sugars, mainly mono and disaccharides and monosaccharides like glucose, fructose, etc. are absorbed by the cell.
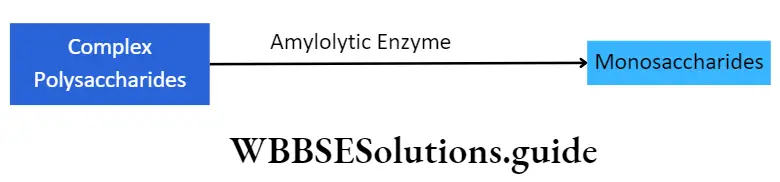
Examples: Salivary amylase (ptyalin), amylopsin, intestinal sucrase, maltase, lactase, etc.
Lipolytic enzymes: The enzymes that hydrolyse fats or lipids present in the food, into fatty acids and glycerol are called lipolytic enzymes or lipases
Role in digestion: Lipases are responsible for the hydrolysis of lipids into fatty acids and glycerol that can be absorbed by the blood as well as the cells.
Examples: Gastric lipase, pancreatic lipase, intestinal lipase, Etc.
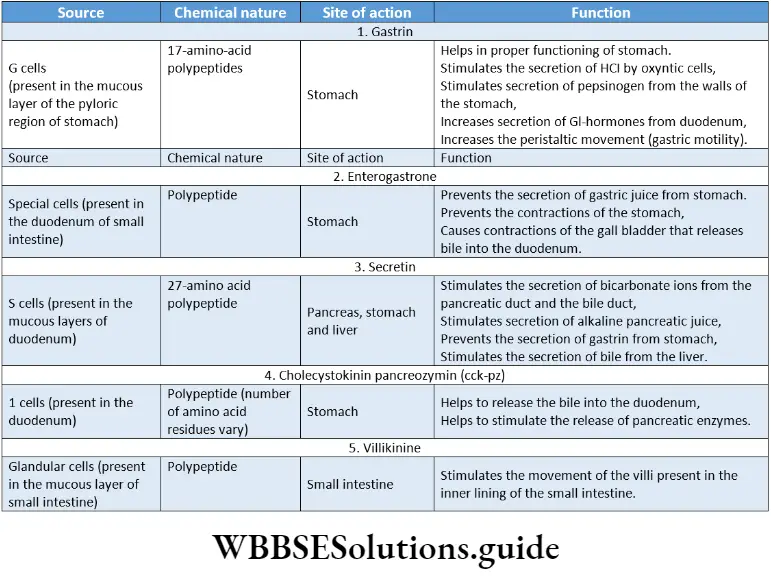
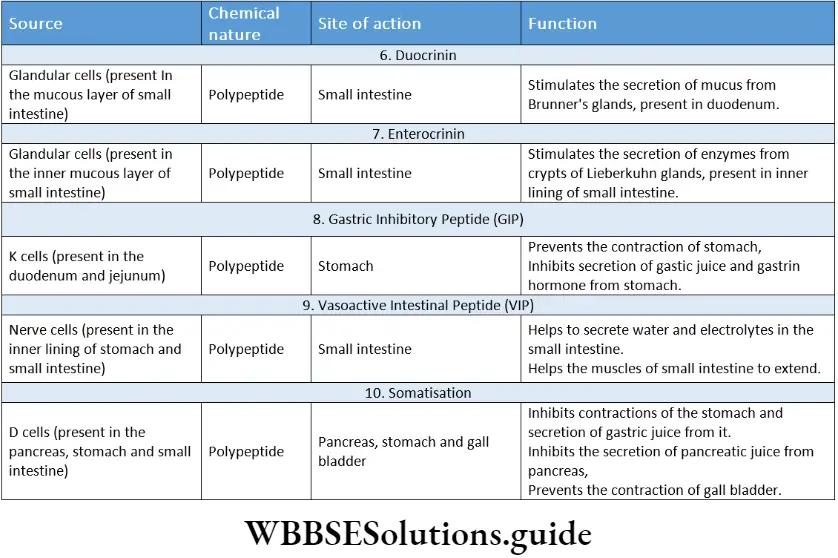
Gastrointestinal Hormones
Gastrointestinal Hormones Definition: The hormones secreted mainly by mucous cells of the digestive tract that control various processes of digestion are called gastrointestinal hormones.
The main gastrointestinal hormones are—
- Gastrin,
- Enterogastrone,
- Secretin,
- Cholecystokinin pan¬creozymin (CCK-PZ),
- Villikinine,
- Duocrinin,
- Enterocrinin,
- Gastric inhibitory peptide,
- Vaso-active intestinal peptide,
- Somatostatin.
These hormones, along with their roles are discussed below.
Peristalsis
Peristalsis Definition: The basic propulsive movement of the digestive tract, including its periodic contractions and relaxations, that enable the food to pass through it, is called peristalsis.
Peristalsis Types: The three types of peristalsis are—
Primary peristalsis: It is the peristaltic wave triggered by the swallowing centre in the brain. It is generally slower and mild in nature. The peristaltic contraction wave travels at a speed of 2 cm/s.
Secondary peristalsis: It is generally faster in nature. It travels around 2-25 cm/s. It extends across the entire small intestine. Scientist Alvarez had named it as true peristalsis. Due to its speed, it is also known as rush peristalsis.
Reverse peristalsis: It is slightly different than the other two types of peristalsis. It occurs in the lower part of the duodenum. Due to this peristaltic movement, the food bolus enters the stomach from the duodenum.
Hence, it is called antiperistalsis or reverse peristalsis. Sometimes, this process occurs in the ileum.
Depending on the condition of the food bolus, the receptors on the inner walls of the duodenum get stimulated. This leads to the antiperistaltic movement. Vomiting is caused due to this antiperistaltic movement.
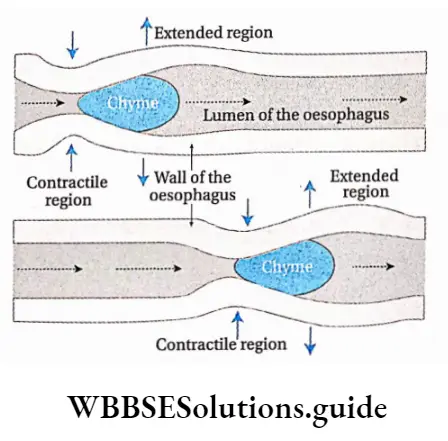
Mechanism of peristalsis: Peristalsis is a propulsive reflex activity that occurs in the digestive tract. Both circular and longitudinal muscle layers are involved in this motion.
Peristalsis is initiated when the outer wall is distended by a bolus or chyme. Bolus of food stimulates mechanoreceptors and chemoreceptors at a specific region in the gastrointestinal tract, ultimately resulting in peristalsis.
The semi-digested food (chyme), after passing through the stomach, enters the small intestine and stimulates the muscles of its inner lining. Due to this, circular muscles of muscularis externa layer, present within the inner lining of the small intestine, contract.
Stimulation at any point in the gastrointestinal tract can cause a contractile ring to appear in the circular muscle. This contractile ring then spreads along the gastrointestinal tract.
This allows the chyme to move downwards. In the next step, these muscles relax and return to their normal state. Due to the alternate contraction and relaxation, chyme gradually moves through the intestine.
Receptive relaxation of the gastrointestinal tract takes place on the distal side of the contractile ring. It allows chyme to be propelled more easily towards the anus. This completes the peristalsis.
Significance of peristalsis: The significances of peristalsis are—
- Transportation of food: In the oesophagus, peristalsis helps to propel the swallowed food or fluid into the stomach. It helps to transport the semi-digested food (chyme) from the stomach to the colon.
- Digestion: Due to peristalsis, different juices like gastric juice, pancreatic juice, bile, etc., can easily mix with the bolus and chyme and stimulate the process of digestion.
- Absorption: It stimulates the absorption of nutrients through the walls of the small intestine, into the bloodstream.
- Blood circulation: Peristalsis or waves of muscular contraction in the gastrointestinal tract also drives the blood flow
- Ejection of faecal matter: Peristalsis occurs about 1-3 times in the large intestine, making the faeces enter the rectum and ultimately helping in its ejection.
Digestion Absorption And Assimilation Of Carbohydrate Protein And Fat
Different substances (such as carbohydrates, protein, fat, etc.) present in food get digested, absorbed and assimilated by the digestive system. These processes are explained below.
Digestion Of Carbohydrates
The process by which complex carbohydrates, present in the food, are broken down into simpler sugars, using amylolytic enzymes is called digestion of carbohydrates.
Carbohydrates comprise 60-80% of our food. An adult human being takes about 300-500 g of carbohydrates every day, which releases about 1200- 2000 kcal of energy.
Carbohydrates present in the food are of three types mainly—
- Monosaccharides (glucose, fructose),
- Disaccharides (lactose, maltose, sucrose),
- Polysaccharides (starch, glycogen, dextrin, cellulose)
Importance of cellulose
Cellulose-containing foods are difficult to digest. But they are an important part of the diet. They provide roughage to the body, which is important for the formation and egestion of faeces.
Roughage is also required for proper peristaltic movements of the intestines and thereby, prevents constipation.
Several bacteria are present within the stomach, small intestine, large intestine, etc., that ferment the cellulose present in the food.
Site Of Digestion
Digestion of carbohydrates is initiated in the mouth by the action of saliva and is completed in the small intestine by I alkaline medium. action of the intestinal juice.
Mechanism of digestion
Carbohydrate digestion by amylolytic enzymes results in the formation of simple carbohydrates, through different steps. These are described in detail below.
Digestion in mouth: The two types of amylolytic enzymes present in saliva are—
- Ptyalin
- Maltase.
Role of ptyalin: This enzyme hydrolyses starch or glycogen into maltose, maltotriose, and isomaltose and limits dextrins in a slightly alkaline medium. But ptyalin can hydrolyse only ar-1, 4-linkages but not ar-1, 6-linkages.
Deglutition Meaning In Biology
Role of maltase: This enzyme acts on maltose to produce two units of glucose.
Digestion in the stomach: There are no carbohydrate hydrolysing enzymes in gastric juice. But HCI present in the gastric juice hydrolyses sucrose molecules into glucose and fructose.
Digestion in the small intestine: Two types of juices, that is, pancreatic juice and intestinal juice, along with bile, are mixed with the chyme in the small intestine.
Digestion by Pancreatic juice: The pancreatic juice contains pancreatic amylase or amylopsin.
It hydrolyses remaining starch, glycogen, dextrin, etc., present in ‘ the food, into disaccharides such as maltose isomaltose, small dextrins, etc., and even glucose. This enzyme functions in the presence of Cl- ions, in an alkaline medium.
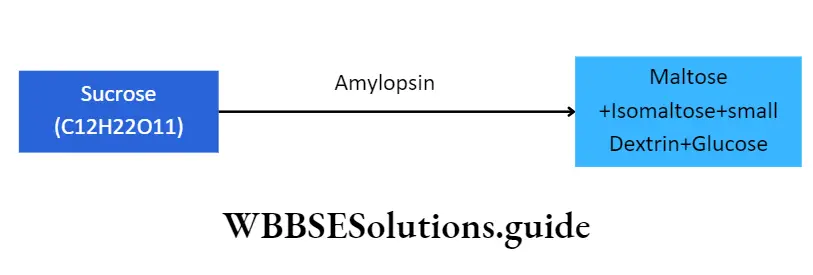
It is to be noted that Cl ions act as activators for both ptyalin and pancreatic amylase.
Digestion by Intestinal juice: The intestinal juice contains the following amylolytic enzymes. These are
- Intestinal amylase
- Isomaltase
- Maltase
- Sucrase
- Lactase.
All these enzymes act in an alkaline medium at pH 8. Their roles in carbohydrate digestion are discussed below.
- Role of intestinal amylase: a-amylase is present in very small quantities in the intestinal juice. The starch and dextrin that somehow escape the action of pancreatic lipase, become the substrate for intestinal lipase. It converts them into disaccharides like maltose, isomaltose, maltotriose, etc.
- Role of isomaltase or oligo-l,6-glucosidase or r-dextrinase: Isomaltase or oligo-l,6-glucosidase or ar-dextrinase breaks ar-1, 6-glycosidic bond of ar-dextrin into maltose and maltotriose. It also hydrolyses isomaltose into glucose.
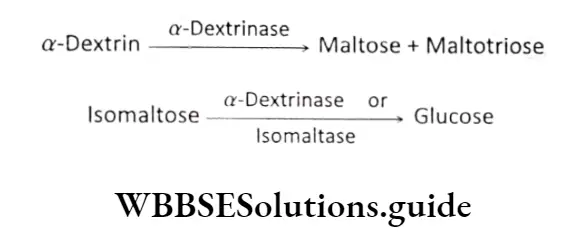
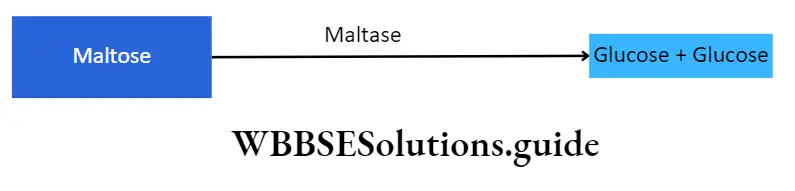
Role of maltase: Maltase present in the intestinal juice hydrolyses disaccharide, maltose, into 2 molecules of monosaccharide, glucose.
1 molecule of maltose (C12H22O11) →Maltase +H2O Glucose (C6H12O6) + Glucose (C6H12O6)
The enzyme hydrolyses trisaccharide, maltotriose into 3 molecules of glucose. The maltase breaks the 1, 4-glycosidic bond between maltose and maltotriose.
1 molecule of maltotriose (C18H32O16) →Maltase 3Molecules of glucose (C6H12O6)
Role of sucrase or invertase: Sucrase or invertase, present in intestinal juice, hydrolyses sucrose into 1 molecule of glucose and 1 molecule of fructose.
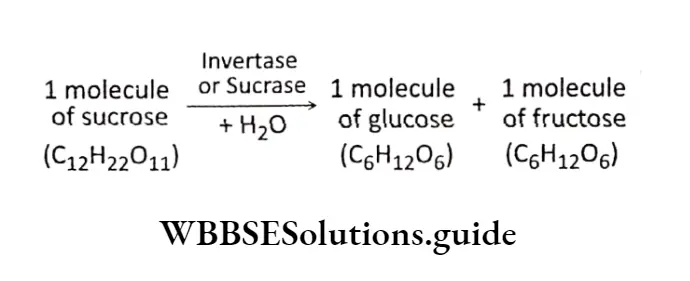
Role of lactase: Lactase, present in intestinal juice, hydrolyses milk sugar lactose, into 1 molecule of glucose and 1 molecule of galactose.
Role of limit dextrinase: Limit dextrinase, present in intestinal juice, hydrolyses dextrins into glucose.
Digestion Of Proteins
The process by which complex protein molecules, are broken down into simpler, absorbable forms (amino acids), using proteolytic enzymes is called protein digestion.
Proteins are required for the proper growth and nutrition of the body. Protein requirement for the body is about 0.5-0.8 g per kg body weight of an adult human being.
For children, this requirement is around 4 g per kg body weight.
The different types of proteins present in the food include—
- Different types of albumin and globulin,
- Milk-protein called casein (phosphoprotein), lactalbumin and lactoglobulin,
- Collagen present in white fibres and elastin in yellow fibres,
- Mucin and
- Nucleoproteins.
Site Of Digestion
Digestion of proteins does not take place in the oral cavity due to the absence of any proteolytic enzymes in saliva. It begins in the stomach and ends in the small intestine.
Mechanism Of Digestion
Protein digestion by proteolytic enzymes results in the formation of amino acids, through different steps. Along with amino acids, some quantities of dipeptides and tripeptides are also generated. These are absorbed by the cells, in their peptide form.
Digestion in the stomach: Protein digestion in the stomach is carried out by the gastric juice.
Gastric juice contains the following proteolytic enzymes—
- Pepsinogen,
- Chymosin,
- Gelatinase.
Besides these, it also contains HCI. Their roles in protein digestion are discussed below.
Role of pepsinogen: It is present in the gastric juice as an inactive proenzyme form. It is initially activated by HCI to form the active enzyme, pepsin.
⇒ \(\text { Pepsinogen } \stackrel{\mathrm{HCl}}{\longrightarrow} \text { Pepsin }\)
Its optimum pH ranges from 1.5-2.2 and hence, can act within the acidic environment inside the stomach.
It is an endopeptidase that cleaves the peptide bond in proteins. It converts metaproteins into proteoses and peptones. It is also capable of digesting collagen, a fibrous protein which is the main constituent of connective tissue in animals.
Role of chymosin: An enzyme, called rennin, is present in the digestive juice of cattle, that helps in the digestion of milk.
It is present in a proenzyme form, prorennin, that gets activated into rennin, in the presence of HCI.
Rennin is present as chymosin in the digestive juice of infants but not in adult human beings. It acts on casein, present in the milk, and converts it to soluble paracasein.
This paracasein binds to calcium ions forming insoluble calcium paracaseinate that is finally digested by pepsin.
Role of gelatinase: In the presence of HCI in the stomach, gelatinase hydrolyses gelatin into peptones
⇒ \(\text { Gelatin } \stackrel{\text { Gelatinase }}{\longrightarrow} \text { Peptone }\)
Role of hydrochloric acid: It is secreted by the oxyntic cells in the stomach.
Its functions in protein digestion are—
- It causes denaturation and disintegration of proteins into small peptides and amino acids.
- It converts proteins to acid metaproteins, which are easily digested.
⇒ \(\text { Protein } \stackrel{\mathrm{HCl} \text { present in gastric juice }}{\longrightarrow} \text { Acid metaprotein }\)
It activates proenzyme forms of the enzymes into their active forms, such as pepsinogen to pepsin and prorennin to rennin.
It lowers the pH in the stomach, making the medium acidic that is suitable for the action of pepsin.
Digestion in the small intestine: Protein digestion continues in the small intestine under the action of pancreatic juice and intestinal juice. Their roles in protein digestion are discussed below.
Role of pancreatic juice: Trypsin, chymotrypsin, carboxypeptidase, elastase and collagenase are pancreatic proteolytic enzymes. Their roles are as follows
Role of trypsin: It is secreted as trypsinogen. It is an inactive form of trypsin. It is initially activated by enterokinase or enteropeptidase enzyme, present in the intestinal juice.
\(\text { Trypsinogen } \stackrel{\text { Enterokinase }}{\longrightarrow} \text { Trypsin }\)Its optimum pH is 8.0. It hydrolyses proteins, proteoses, acid metaproteins, peptones, etc., into simpler and smaller peptides such as aminopeptides, dipeptides, tripeptides, etc.
Deglutition Meaning In Biology
Role of chymotrypsin: It is secreted as chymotrypsinogen. It is an inactive form of chymotrypsin.
It is activated by trypsin. Its optimum pH is 8.0. Chymotrypsin converts casein, present in milk, into paracasein in the slightly alkaline medium of the small intestine. Thus, its function is to coagulate milk.
Role of carboxypeptidase: It is secreted in an inactive form called procarboxypeptidase.
It is activated by trypsin. Carboxypeptidase has an optimum pH of 7.4. It hydrolyses long polypeptide chains into smaller ones.
It specifically hydrolyses the amino acid from the carboxyl end of peptide chains, to yield individual amino acids.
⇒ \(\begin{array}{ll}
\text { Long chain } \stackrel{\text { Carboxypeptidase }}{\longrightarrow} & \text { Small peptides + } \\
\text { polypeptides } & \text { Amino acids }
\end{array}\)
Role of elastase: It acts on a protein, named elastin. It hydrolyses the carboxyl group of the terminal amino acid, producing smaller peptide chains.
⇒ \(\text { Elastin } \stackrel{\text { Elastase }}{\longrightarrow} \text { Small peptides }\)
Role of collagenase: It acts on a protein, named collagen. It hydrolyses the collagen fibres, producing smaller peptide chains.
⇒ \(\text { Collagen } \stackrel{\text { Collagenase }}{\longrightarrow} \text { Small peptides }\)
Role of intestinal juice: The main proteolytic enzyme present in intestinal juice is erepsin.
Erepsin is actually a mixture of aminopeptidases, dipeptidases, tripeptidases and enterokinase. These protein hydrolysing enzymes serve a major role in alkaline medium.
Role of aminopeptidase: It is an exopeptidase (peptidase that catalyses the cleavage of terminal peptide bonds).
It acts on the amino terminal of the polypeptides and finally releases an amino, acid. It results in the formation of dipeptides and tripeptides.
⇒ \(\begin{array}{ll}
\text { Long chains of } \stackrel{\text { Aminopeptidase }}{\longrightarrow} & \text { Tripeptide, }+ \text { Amino } \\
\text { polypeptide } & \text { dipeptide } \text { etc. acids }
\end{array}\)
Role of tripeptidase: Tripeptidases act on tripeptides and hydrolyse them into dipeptides and amino acids.
⇒ \(\text { Tripeptide } \stackrel{\text { Tripeptidase }}{\longrightarrow} \text { Dipeptide + Amino acid }\)
Role of dipeptidase: Dipeptidases act on dipeptides and hydrolyse them into two amino acids.
⇒ \(\text { Dipeptide } \stackrel{\text { Dipeptidase }}{\longrightarrow} \text { Amino acid }+ \text { Amino acid }\)
Digestion Of Fats
The process by which fats and lipids present in the food are broken down into simple and absorbable forms like fatly acid and glycerol using lipolytic enzymes, is called digestion of fat.
Fats are the main source of energy. They provide us with the energy for various metabolic processes.
The different fats that are present in the food are—
- Neutral fats or triglycerides,
- Phospholipids,
- Cholesteroids,
- Free cholesterol,
- Fatty acids and
- Glycerol.
About 25% of the fats get converted into fatty acids and glycerol. Some of the fats undergo partial hydrolysis to form monoglycerides and diglycerides.
Site of digestion
Digestion of fats does not take place in the oral cavity due to the absence of any lipolytic enzyme in the saliva. Its digestion begins in the stomach, by gastric juice and is fully digested in the small intestine, by intestinal juice.
Mechanism of digestion.
The key issue in the digestion of fats is that of solubility—lipids are poorly soluble in water. Thus digestion is greatly aided by emulsification (the breaking up of fat globules into much smaller emulsion droplets). It enhances the surface area of the lipid so that water-soluble.
lipase can work on the globule surface of triacylglycerol (TAG). The mechanism of digestion of fats is as follows.
Digestion in the stomach: The fat-digesting enzyme present in gastric juice is gastric lipase.
Role of gastric lipase: The action of gastric lipase is inhibited by the absence of any emulsifying substance and the presence of hydrochloric acid in the stomach.
So, it has mild action over the fats and converts them into fatty acids and monoglycerides.
⇒ \(\text { Fat } \stackrel{\text { Gastric lipase }}{\longrightarrow} \text { Fatty acids }+ \text { Monoglyceride }\)
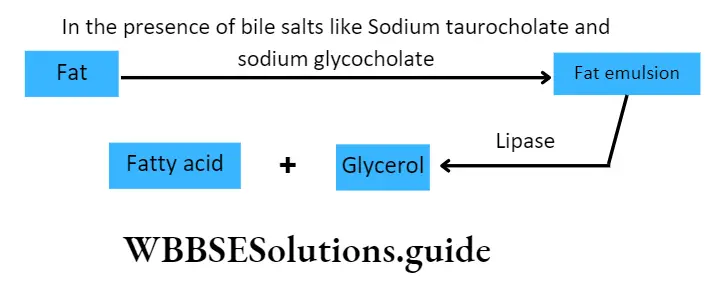
Digestion in the small intestine: The main digestion of fats takes place in the small intestine. When the chyme enters the small intestine, three alkaline secretions— bile, pancreatic juice and intestinal juice, are mixed with it.
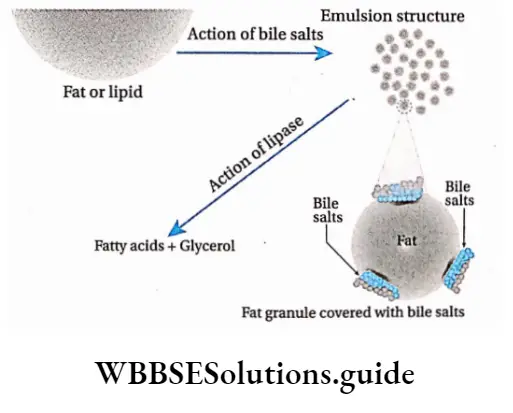
Role of bile: It plays an important role in fat digestion. The chyme mixes with the bile salts due to peristalsis.
The bile salts such as sodium glycocholate and sodium taurocholate have the ability to break down large fat droplets into smaller ones. This process is called emulsification of fats.
It increases the surface area of the fat droplets and decreases the surface tension of the fat droplets to prevent the adherence of the fat droplets together again. This makes the action of the enzyme lipase, easier.
Role of pancreatic juice: The enzymes for fat digestion present in pancreatic juice, are—steapsin, phospholipase, cholesterol esterase. Their roles are discussed as follows.
Role of steapsin: Steapsin present in pancreatic juice, hydrolyses emulsified fats under a slightly alkaline medium. 1 molecule of triglyceride gets hydrolysed into 3 molecules of fatty acids and a molecule of glycerol.
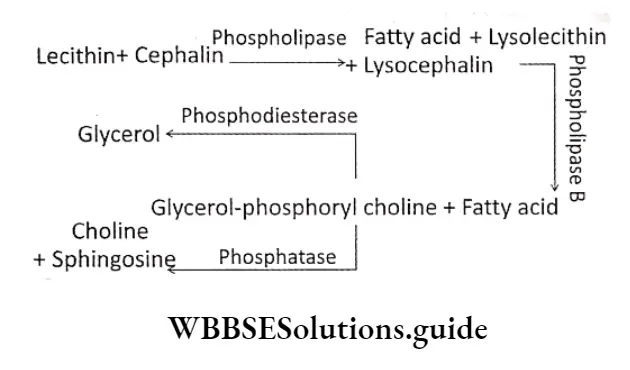
Role of phospholipase: The enzyme, phospholipase, acts upon two phospholipids, lecithin and cephalin
Both lecithin and cephalin release 1 molecule of fatty acid from each of them, producing lysolecithin and lysocephalin, respectively.
Further action of phospholipase B on these products releases another fatty acid molecule and glycerol-phosphoryl choline.
When phosphodiesterase acts upon them, glycerol is released. On the other hand, when phosphatase acts on them, choline and sphingosine are released.
Role of cholesterol esterase: Cholesterol esterase is also termed as cholesterol ester hydrolase.
Cholesterol esterase present in the pancreatic juice, acts on cholesterol ester or cholesteroid to form cholesterol and fatty acids, on hydrolysis under slightly alkaline medium.
Intestinal juice: The intestinal juice contains the following lipolytic enzymes—intestinal lipase, and lecithinase. Their roles in fat digestion are as follows.
Role of intestinal lipase: It breaks down emulsified fats into glycerol and fatty acids. It produces 3 molecules of fatty acids and 1 molecule of glycerol from each molecule of triglyceride.
Role of lecithinase: It hydrolyses a phospholipid named lecithin into fatty acids, glycerol, choline and inorganic phosphate.
⇒ \(Lecithin \stackrel{\text { Lecithinase }}{\longrightarrow} Fatty acid + Glycerol + Choline + Inorganic phosphate\)
Absorption Of Carbohydrates
The process by which end products of carbohydrate digestion pass through the interstitial mucosa into the lymph or blood, is known as absorption of carbohydrate.
Simple carbohydrates (such as glucose, fructose, and galactose) do not require further digestion.
Complex carbohydrates (such as starch, glycogen, etc.,) are absorbed mostly as monosaccharides (such as glucose, galactose, fructose, levulose).
Some quantities of carbohydrates are also absorbed as disaccharides (such as sucrose, maltose, lactose, etc.)
Human digestive system: structure, enzymes, and absorption mechanism
Site of absorption
Even though some amount of monosaccharides may be absorbed through the mucosa of the stomach, most of the soluble products of digestion are absorbed in the small intestine.
The maximum amount of carbohydrates is absorbed in the duodenum and jejunum, leaving a very small amount for the ileum to absorb. Other than this, some amounts of glucose and galactose are absorbed in the large intestine.
Absorption pathway
The products obtained by the digestion of carbohydrates get absorbed by the microvilli or brush-bordered enterocytes, into the lumen of the small intestine.
These substances enter the network of blood capillaries and then into the hepatic portal system. Finally, they enter into the liver. A small amount of these products pass through the lacteals and flow through the lymph.
Process of absorption
Different types of carbohydrates are absorbed by different processes. These have been discussed below.
Absorption of monosaccharides:
Most of the glucose gets absorbed by this mechanism. This means that their absorption requires the expenditure of energy.
It takes place against the concentration gradient, i.e., occurs even when their concentration in the intestinal
lumen is less than that in the blood. For the active absorption of glucose, carrier proteins and Na+ ions are required.
This mechanism is also known as the active sodium-monosaccharide symport process.
In this case, the carrier protein is sodium-glucose transporter (SGLT-1). Na+ ions are present in the intestinal lumen while carrier proteins are present on the membrane covering the microvilli, located on epithelial cells of the villi.
The carrier protein has 2 separate sites—one for Na+, and the other for glucose. A complex is formed by SGLT-1, glucose molecule, Na+ and carrier protein on the microvilli membrane, towards the intestinal lumen.
This complex passes through the microvilli membrane to the cytoplasmic end of the cells. Here the complex breaks down and glucose molecules and Na+ enter the cells.
It transports 2 Na+ ions (along the concentration gradient) and 1 glucose molecule (against the concentration gradient) to the cytoplasm of the cell. The carrier protein separates from the complex and the same mechanism is repeated.
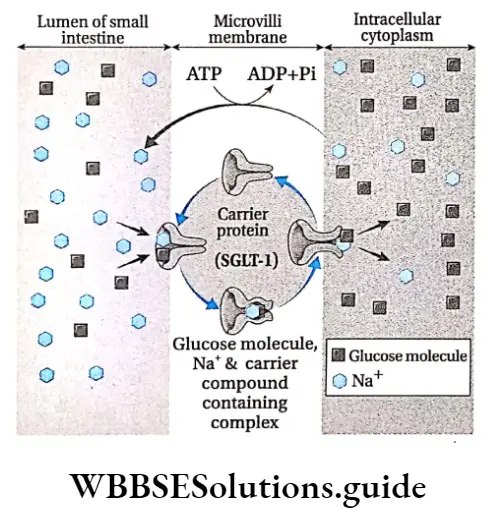
Deglutition Meaning In Biology
Some amounts of glucose and galactose enter the enterocytes by sodium-independent, facilitated diffusion.
During high glucose concentration in the enterocytes, absorption of glucose occurs through a facilitated diffusion process. In this case, a carrier protein named glucose transporter-2 or GLUT-2 is involved.
Some amounts of glucose and galactose also enter the small intestine by simple diffusion.
Absorption of fructose takes place by diffusion. It is passive in nature, i.e., no energy is required for the process and takes place along the concentration gradient.
Among the monosaccharides, pentose and tetrose-like carbohydrates (such as arabinose) get absorbed by simple diffusion.
Absorption of disaccharides: Some amount of disaccharides like sucrose, maltose and lactose get absorbed in the jejunum and ileum. The absorption of these carbohydrates takes place by simple diffusion, which occurs passively, along the concentration gradient.
Absorption Of Proteins
The process by which end products of protein digestion pass through the interstitial mucosa into the lymph or blood, is known as absorption of protein.
Digestion products of proteins are absorbed mainly as amino acids. A small quantity of protein is absorbed as dipeptides or tripeptides.
Site of absorption
Absorption of amino acids occurs in the small intestine. It is rapid in the duodenum and jejunum, but slow in the ileum.
Absorption pathway
The amino acids get absorbed by the epithelium of the villi in the small intestine. They enter the blood flowing through the network of blood capillaries around the villi.
They are then transported to the liver by the hepatic portal vein. From the liver, they are transported to the different organs of the body. A very small amount of amino acid after being absorbed by the villi, gets absorbed into the lacteal and flows through the lymph.
Process of absorption
Amino acids dipeptides and tripeptides are absorbed by different processes. These have been discussed below
Absorption of amino acids:
Active absorption of amino acid in the gastrointestinal tract involves a mechanism similar to that of glucose absorption.
At least four sodium-dependent amino acid transporters are present in the luminal plasma membrane of enterocyte. This process—
- Takes place against the concentration gradient,
- Requires cellular energy and
- Requires carrier proteins (na+-amino acid co-transporter) and na+ ions the carrier protein is present on the microvilli membrane. These transporters bind na+ and amino acid molecules to form a complex.
- This complex passes through the microvilli membrane, towards the cytoplasmic end of the cell.
- On reaching the cytoplasmic end, the complex undergoes conformational change and breaks down to release Na+ and amino acid into the cytoplasm.
- The earner problem separates and repeats the same process with another Na and ammo acid molecule.
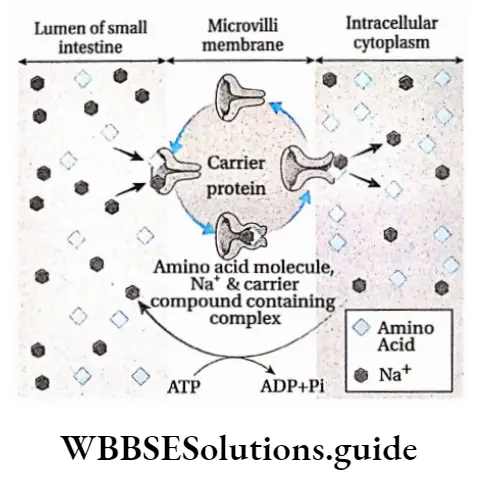
Some of the amino acids get absorbed through the brush-bordered enterocytes by sodium-independent amino acid-transporter.
Once amino acids are in the enterocyte, however, they accumulate and eventually move by facilitated diffusion through the base of the cell and into the blood.
Some amino acids get absorbed within the small intestine by simple diffusion.
Absorption of dipeptides and tripeptides:
Dipeptides and tripeptides are mainly absorbed by the epithelium of the villi and then to blood capillaries.
Absorption Of Fats
The process by which the end product of fat digestion passes through the interstitial mucosa into the lymph or blood is known as the absorption of fat.
About 75% of hydrolysed fat is absorbed mainly as higher fatty acids, glycerol, monoglycerides and cholesterol. Only 25% of the hydrolysed fat is absorbed as fatty acids and glycerol.
Site of absorption
The products of digestion of fats enter the circulatory system from the small intestine, mainly in the jejunum and ileum.
Absorption pathway
- Digested as well as semi-digested fats get absorbed by the epithelium of the small intestine.
- From The epithelium, they get Absorbed into lymph vessels called lacteals. These fats continue to flow within the lymph Present In the Lacteals. The fats next enter the bloodstream from this lymph.
- Only a small amount of fat gets absorbed by the blood in the blood capillaries, surrounding the villi. They are then transported to the liver by the hepatic portal vein.
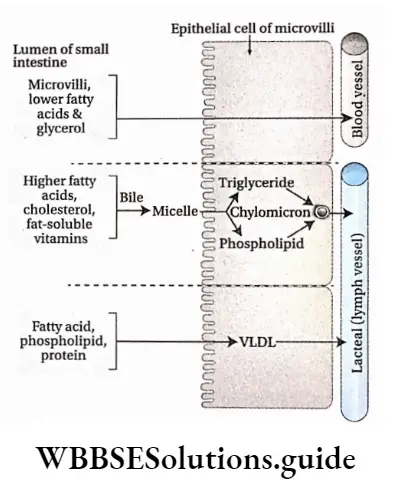
Process of absorption
Fats are absorbed by different processes. These have been discussed below.
Absorption of lower fatty acids and glycerol by portal veins:
- Water-soluble, lower fatty acids and glycerol get absorbed into the epithelial cells of villi from the intestinal lumen.
- From the villi, they enter the nearby blood capillaries. They are then carried to the liver by the hepatic portal vein.
- Some amount of fatty acids, phospholipids and proteins, get absorbed through the villi into the intestinal lumen.
- They combine with each other to form VLDL (very low-density lipoproteins), that enter the lacteal and flow into the lymph. Finally, they enter into the blood flow.
Absorption of higher fatty acids by lacteal: Higher fatty acids being insoluble in water, cannot be directly absorbed into the blood. They are absorbed by the intestine.
In the lumen of the small intestine, higher fatty acids, monoglycerides and fat-soluble vitamins associate to form water-soluble droplets called micelles.
Bile salts and potassium bicarbonate ions help the micelle to penetrate through the microvilli of enterocytes, into the cells.
After entry inside the enterocytes, the bile salts are released and fats (triglycerides) are re-synthesised.
Those triglycerides are then coated with a layer of phospholipids and proteins to form small globules called chylomicrons.
These are about 1 micrometre in diameter. They enter lymphatics (lacteals) instead of blood capillaries due to their larger size. From the lymph, they enter into the bloodstream.
Different hypotheses regarding the absorption of fats
Lipolytic hypothesis:
- This hypothesis was postulated by Verzar and McDougall. According to this hypothesis, the fatty acids and glycerol generated during digestion of fats, are absorbed separately within the body.
- The fatty acids combine with the bile salts to form a complex, which is absorbed by the epithelial cells of the small intestine.
- Especially fatty acids combine with glycerol to synthesise triglycerides that enter the lymph vessels.
Partition hypothesis:
- This hypothesis has been postulated by Frazer. According to this hypothesis, 30% of the fat is hydrolysed in the small intestine to form mono and diglycerides. The rest 70% forms an emulsion of unhydrolysed fats.
- The small hydrolysed fatty acids get absorbed by the portal system. Some part of the hydrolysed as well as unhydrolysed fat gets absorbed by the central lacteal in the villi of the small intestine.
- Finally, they enter the lymph vessels. The unhydrolysed fat is now transferred to the blood vessels through the thoracic duct.
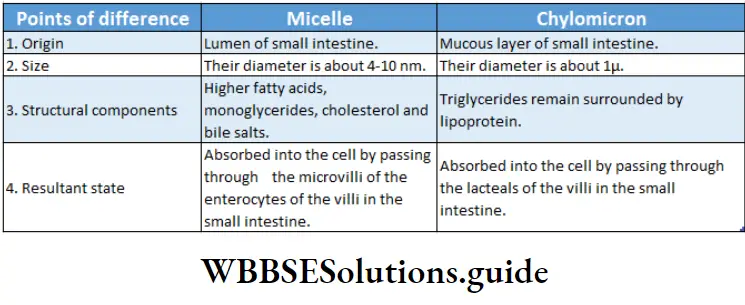
Assimilation Of Carbohydrates
Assimilation is the biological process through which absorbed food materials become the integral component of the protoplasm and extracellular materials.
After digestion of carbohydrates, mainly monosaccharides are obtained. Glucose is the most important monosaccharide obtained, that undergoes various metabolic processes in the body. The metabolic processes of the body that utilise glucose, are as follows.
Glycogenesis
The enzyme-controlled, biochemical process by which glycogen is synthesised within the cell, from glucose and other monosaccharides is called glycogenesis.
Site of occurrence: Liver and muscle fibres
Ribose-5-phosphate and other pentose phosphates are synthesised from glucose and glycogen.
This occurs by a hexose monophosphate (HMP) shunt. These pentose phosphates are used to synthesise DIMA and RNA.
Site of occurrence: Liver, adipose tissue, adrenal cortex, mammary glands, etc.
Glycogenolysis
The enzyme-controlled biochemical process by which glycogen, mainly stored in the liver, gets converted into glucose by several steps within the cell is called glycogenolysis.
Site of occurrence: Liver and cytoplasm of muscle fibres
Normal glucose concentration in the blood
Some amount of glucose is always present in the blood. It is known as blood sugar. An adult human being has 70-100 mg of glucose per 100 ml of blood. This is known as normal blood sugar.
Hyperglycemia, glycosuria and hypoglycemia
Insufficient secretion of the hormone insulin in the body causes diabetes mellitus. Under such conditions, blood sugar level rises (hyperglycemia) and thereby excess glucose gets excreted through the urine (glycosuria).
It is generally seen when there is more than 180 mg of glucose/100 ml of blood. During fasting, the blood glucose level falls, resulting in the condition called hypoglycemia.
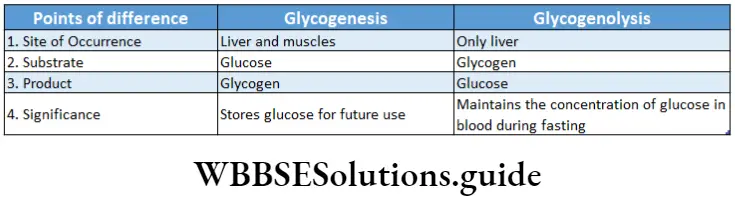
Assimilation Of Proteins
The final products of protein digestion are amino acids. They are absorbed in the small intestine and then pass through the liver before reaching the main bloodstream.
This amino acid are released from the liver to the cells for the synthesis of protein, enzymes, and non-proteinaceous substances (like fat, carbohydrates etc.) and for the production of energy. Excess amino acids get deaminated by the separation of amino groups which combines with CO2 and form urea.
Amino acid pool
The amino acids, resulting from the digestion of proteins, get absorbed in the small intestine and get added to the amino acid pool. The amino acids required for the synthesis of different proteins or non-protein nitrogen (NPN) are taken up from this amino acid pool.
Different uses of amino acids produced from proteins are as follows-
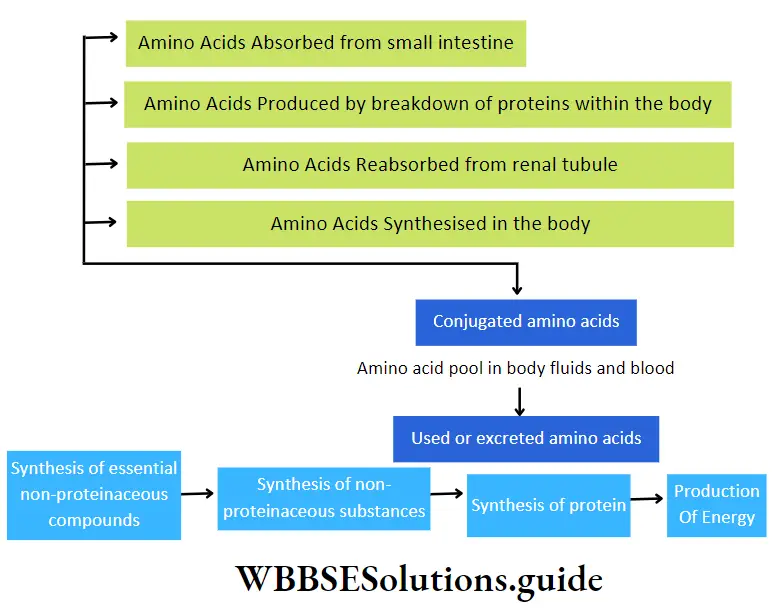
Assimilation Of Fats
Complete digestion of fats or lipid molecules within the alimentary canal produces fatty acids and glycerol.
Partial hydrolysis of lipids produces monoglycerides, diglycerides, etc Fatty acids, glycerol, monoglycerides, diglycerides, etc., get absorbed in the small intestine.
After passing through lacteals, they enter the blood. These components take part in several catabolic and anabolic reactions in the body.
Some important examples are—
- Most of the fats or lipids get stored within the body in several regions like under the skin, mesentery, etc. They prevent the loss of heat from the body.
- A layer of fat is present around the organs, to protect them from mechanical shock.
- Fats or lipids, combine with phosphate and proteins to form phospholipids and lipoproteins. Lipids are essential for the synthesis of steroid hormones.
- Triglycerides or neutral fats are generated from fatty acids and glycerol, mainly in the hepatic cells. This process is known as lipogenesis.
- These are synthesised by intestinal cells and passed into the chyle (milky body fluid consisting of lymph and emulsified fats). Then they go to blood as neutral fat being suspended in plasma.
- Ketone bodies are produced from the fats by ketogenesis. It is used as fuel by the body.
- Energy is released from fatty acids by β-oxidation.
β -Oxidation Of Fatty Acids
The oxidation of fatty adds at β-carbon (third carbon) considering —the COOH group as the first carbon is known as β-oxidation of fatty adds.
Site of occurrence: It takes place in the mitochondria of hepatic cells. It may also take place in cells of the brain, cardiac muscles, kidneys, etc. Additionally, peroxisome also contains the enzyme for this process.
Calorific Value Of Food
Definition: The amount of energy produced by oxidation of lg of protein, fat or carbohydrate, within the cell is called its calorific value.
Unit of calorific value: The solar energy remains stored as chemical energy within the molecules of proteins, fats and carbohydrates. On oxidation, the chemical energy gets converted into heat energy.
This heat energy is utilised by the cells to carry out the various metabolic and physiological processes in the body.
The unit of energy is calorie (cal). It is the heat required to raise the temperature of lg of pure water by 1°C. In biological processes, the unit is generally used in kcal.
1 Kcal=1000 cal
Calorific values of proteins, carbohydrates and fats: Different types of food provide different fat yields of 9.3 kcal (1 kcal = 4.1868 x 103 joules). One gram of carbohydrate yields 4.1 kcal while, one gram of protein yields 4.3 kcal.
Bomb Calorimeter
A bomb calorimeter is used to measure the calorific values of proteins, carbohydrates and fats. The specific amount of the food sample is placed within a funnel-shaped container inside the instrument.
This sample is oxidised by passing electricity in the presence of oxygen. The energy that is released is measured according to the principle of calorimetry.
Later, scientists Benedict and Atwater determined the amount of energy released by the food inside the cell
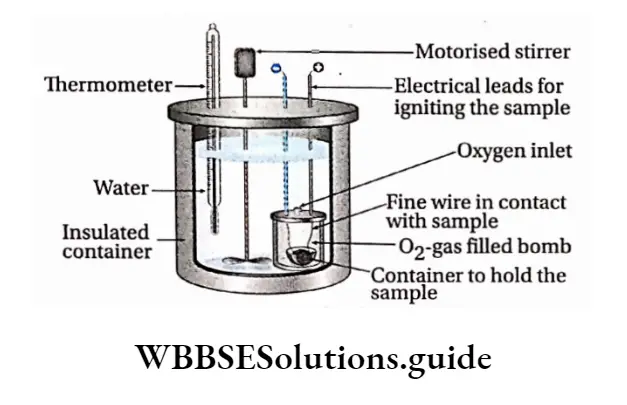
Egestion
Egestion Definition: The process by which remaining undigested, unabsorbed parts of the food are removed from the body, through the anus is called egestion.
Colon during the last phase of digestion. After the nutrients are absorbed in the small intestine, the undigested part of the food passes through the ileocecal valve into the large intestine.
By the peristaltic movement, these substances pass through the ascending, transverse, descending and sigmoid colon, Finally, they reach the rectum where they are stored for some time before egestion.
Composition of faeces: About 1500 ml of chyme enters the large intestine of an adult human being, out of which only 200 ml is excreted as faeces. Faeces are composed of water (75%) and undigested food, fibres, inorganic substances, epithelial cells, etc. It also contains microorganisms, mainly bacteria (5%), secretions of the gastrointestinal tract and mucus secreted by goblet cells,
Egestion of faeces:
- Egestion of faeces occurs as a reflex action. It is excreted from the body through the anus.
- The anus is normally closed by a pair of sphincter muscles. The internal anal sphincter is composed of smooth muscle, and the external anal sphincter is composed of skeletal muscles.
- The external anal sphincter is voluntary in nature, therefore, the opening and closing of the anus are under control.
- Faecal matter enters the rectum due to strong contractions of the sigmoid colon. This causes sudden distension of the walls of the rectum. The receptors in the rectum get stimulated due to this distension.
- This stimulation is sent to the brain, via the nerves. It is interpreted by the brain and the need to defecate is felt. Increased contractions of the colon and rectum help to push faeces through the anal canal, and out of the anus.
Significance of egestion:
- Undigested food, edible fibres (cellulose, hemicellulose, etc.), bacteria, etc., are released from the body by faeces.
- If the egestion of faeces is not regular, then the ability of the colon to undergo peristaltic contractions decreases.
- This leads to the accumulation of faeces in the colon. This condition is known as colonostasis or atonia constipation.
Disorders associated with improper egestion
- Irritable bowel syndrome (IBS): It includes stomach ache, constipation, flatulence in the intestines due to accumulation of gas, etc.
- Inflammatory bowel disease: It includes stomach ache, diarrhoea, wound in the colon, fever, loss of body weight, etc.
- Colorectal cancer: It includes the formation of a malignant tumour (cancerous in nature) in the colon or rectum
- Haemorrhoids or piles: It includes thickening of the inner lining of the rectum or anal canal, which may lead to bleeding and painful egestion of faeces.
Nutritional And Digestive Disorders
Nutritional And Digestive Disorders Definition: The disorders that pertain to the gastrointestinal tract and are caused due to nutritional deficiency or improper functioning of the digestive system are called nutritional and digestive disorders.
Some of these nutritional and digestive disorders are discussed below in detail
Protein Calorie Energy Malnutrition (PCM ) Or Protein Energy
The group of clinical conditions, observed mainly in children, which occur due to deficiency of protein or energy-giving nutrients or both in the diet, are called Protein Calorie Malnutrition (PCM) or Protein Energy Malnutrition (PEM).
Protein Calorie Energy Malnutrition Causes:
- A deficiency of protein-rich food during the foetal stage as well as during infancy and childhood is a major cause of PEM. Besides proteins, deficiency of vitamins, minerals, etc., can also lead to such disorders.
- The inability of the body to digest, absorb and assimilate the nutrients that are generated due to improper functioning of the digestive system is another important cause of such disorders.
- Lack of health consciousness and inadequate breastfeeding by the mother also cause PEM.
Protein Calorie Energy Malnutrition Types: Two types of disorders are caused by PEM—
- Kwashiorkor
- Marasmus.
Protein Calorie Energy Malnutrition Causes:
- Kwashiorkor is caused by protein deficiency. This condition usually occurs at about the age of 12 months to 4 years.
- Marasmus is caused by total calorie/energy depletion. It usually develops in children between the ages of six months and one year.
Protein Calorie Energy Malnutrition Symptoms:
- Symptoms of kwashiorkor include improper growth and weight loss, liver enlargement, oedema, dry or peeling skin, hair discolouration, abdominal distension due to accumulation of fluid, anaemia, diarrhoea, ulcers in the tongue and at the corner of the lips, weak immune system, irritation, moon-like face, etc.
- Symptoms of marasmus include stunted growth and loss in weight. It is also characterised by weak limbs, profound weakness, frequent infections, loss of appetite, diarrhoea, dry skin, loosening of the skin due to degeneration of fats, and thin and discoloured hair.
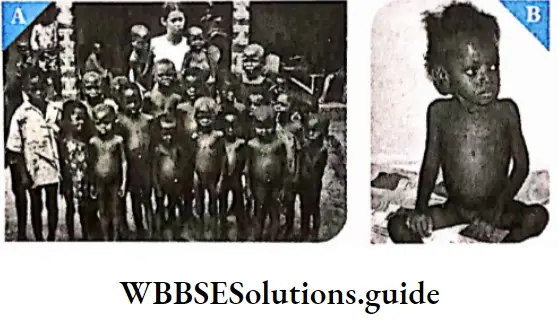
Deglutition Meaning In Biology
Preventive measures: PEM and PCM can be prevented by the following preventive measures—
- Adequate nutrition, specifically, intake of adequate amounts of protein in the diet must be taken.
- Proper care of the mother should be taken right from the beginning of her pregnancy. Adequate amount of proteins must be there in her diet.
- Breastfeeding for the first six months of the child should be ensured, along with proper nutrition.
Indigestion
The disorder that arises due to improper digestion of food, leading to a loss of appetite and feeling of stomach satiety is called indigestion or dyspepsia.
Indigestion Causes:
- Eating too spicy or fat-containing heavy meals, eating too heavy meals may be an important cause of indigestion.
- Decreased secretion of the enzymes required for digestion also leads to indigestion.
- Indigestion may also be caused due to mental anxiety.
- Food poisoning is another cause of indigestion.
Indigestion Symptoms: Symptoms of indigestion include loss of appetite, feeling of stomach satiety, sour taste, nausea, stomach ache and feeling of discomfort. Sometimes constipation is also a symptom of indigestion.
Preventive measures: Indigestion can be prevented by adopting the following measures—
- Eating very rich, spicy foods should be avoided.
- Too heavy meals must be avoided. Small, regular meals must be taken.
- Enough consumption of water must be ensured. This helps in proper digestion.
- Regular exercise ensures the proper functioning of the digestive system. Hence, exercise should be a part of the daily routine. Mental anxiety must be avoided.
Constipation
The disorder that is marked by difficult or infrequent passage of faeces is called constipation.
Constipation Causes:
- Decreased contractions of the intestines lead to slower movement of bowels through the colon. Hence, constipation occurs.
- Lack of an adequate amount of fibre in the diet causes constipation.
- A low amount of water intake causes constipation.
- Mental anxiety or depression, and lack of physical activity also lead to constipation.
- It may also be caused by tumours or ulcers in the intestines, which block the pathway of the faeces.
- Taking laxatives or medications against constipation can make it chronic.
Constipation Symptoms:
- Symptoms of constipation include very less bowel movements, with the stool being very hard and dry.
- Blood may also be discharged along with the faeces. Loss of appetite and stomach discomfort are its other symptoms.
Vomiting Or Emesis
Forceful oral expulsion of gastric or intestinal content, due to reverse peristalsis caused by accumulation of fluid in the stomach or intestine, is called vomiting.
Vomiting Causes:
- Due to improper absorption of water from the food during digestion, food in semi-liquid or liquid form accumulates in the stomach or small intestine. This stimulates the mucous layer leading to vomiting.
- Vomiting may also be caused by stimulation of the inner walls of the pharynx due to any chemical or foreign body that has entered the body along with food.
- Over-consumption of alcohol or infection in the gall bladder and intestines also causes vomiting.
- In the case of some people, travelling to high altitudes (high altitude sickness) or by sea (sea sickness due to rolling to sea) may initiate vomiting.
Vomiting Symptoms: Symptoms of vomiting include a feeling of discomfort in the stomach, nausea and loss of appetite.
Preventive measures: Vomiting can be prevented by the following measures—
- Particular chemicals or odours that may initiate vomiting for a person should be avoided.
- Consumption of small and light meals must be ensured if vomiting has occurred due to indigestion.
Jaundice
The disorder caused due to the accumulation of bile pigments (bilirubin, biliverdin) in blood is called jaundice,
Jaundice Causes and types: Based on the causes, jaundice can be categorised into three types—
- Haemolytic jaundice is caused by to excessive destruction of RBCs within the spleen. This leads to the rupturing of the plasma membrane of the RBCs, releasing haemoglobin (haemolysis) formation of dark yellow-coloured stool.
- Hepatocellular jaundice is caused due to improper functioning of the liver, when the person is suffering from viral hepatitis or drug-induced hepatitis cirrhosis of the liver, etc. This leads to an accumulation of bile pigments in blood and other cells of the body.
- Obstructive jaundice is caused due to blockage in the bile duct. This leads to less bile secretion and more bile absorption by the hepatic portal vein and lymphatic ducts. As a result, the concentration of bile pigments increases in the blood, colour of the stool becomes pale mud Causing Obstructive jaundice.
Jaundice Symptoms: Symptoms of jaundice include yellowing of skin, mucous membranes and conjunctiva of eyes. Dark yellow or yellowish-green coloured urine is also released in jaundice.
Preventive measures: Jaundice can be prevented by the following measures—
- Since this disease is mainly caused due to improper functioning of the liver, hence, its proper functioning must be checked regularly.
- Bilirubin excretion test, liver function test, etc., are some of the tests that can check liver functioning.
- According to the results of the above tests, proper medical assistance should be taken.
- Water that is consumed must be clean and filtered. Contaminated and impure water consumption can cause jaundice.
Diarrhoea
Gastrointestinal infections caused by a wide range of pathogens including bacteria, viruses and protozoa are called diarrhoea.
Diarrhoea Causes and Types: Diarrhoea can be categorised into the following types—
- Infectious diarrhoea—Diarrhoea that is caused mostly due to contamination by bacteria (such as Campylobacter sp., Salmonella sp., Shigella sp., and Escherichia coli.) and viruses (such as Rotavirus, Calicivirus, and Adenovirus).
- Psychogenic diarrhoea— Tension, fear, etc., are some of the emotions that can cause diarrhoea.
- Ulcerative colitis—In this case, ulcer and inflammation occur in most of the large intestine.
Diarrhoea Symptoms: Symptoms of diarrhoea can range from slightly watery stools to more frequent extremely watery stools.
The frequency of bowels may reach upto 15-20 times a day. Due to the loss of water and minerals like sodium, and potassium salts through the stools, the body gets dehydrated and becomes weak.
Diarrhoea Preventive measures: Diarrhoea can be prevented by the following measures—
- Proper hygiene and cleanliness must be maintained to prevent infection by germs.
- Food should always be kept covered.
- In the case of diarrhoea-affected patients, ORS solutions must be given frequently to replenish the water content in the body.
- In case of severe diarrhoea, intravenous saline must be given after proper medical assistance.
Digestion And Absorption Notes
- Bile salts: A mixture of sodium salts of bile acids, cholic acid and chenodeoxycholic acid, synthesized in the liver as a derivative of cholesterol. It helps in emulsification of fats.
- Bolus: A small rounded mass of chewed food.
- Castle’s Intrinsic Factor: A glycoprotein produced by the parietal cells of the stomach and is necessary for the absorption of vitamin B12. It has been named after American physiologist W.B. Castle.
- Emulsification: A process by which two immiscible substances are mixed or one is suspended in another
- Enterocytes: The tall columnar cells that are found in the luminal side of the small intestine and colon and are capable of absorbing water and nutrients from the digestive tract
- Lymph Node: Each of the small swellings present in the lymphatic system where lymph is filtered and lymphocytes are formed.
- Mucin: A class of glycoprotein present in mucus having water-retaining properties.
Points To Remember
- The major function of the GL tract is the digestion and absorption of nutrients.
- The alimentary canal is the continuous muscular digestive tube comprising of mouth, pharynx, oesophagus, stomach, small intestine, and large intestine.
- Saliva, secreted by salivary glands, helps in swallowing food, carbohydrate digestion and transport of immunoglobulins.
- The pharynx provides a common path for food, fluids, and air.
- The stomach is the part of the alimentary canal that can be distended the most. It is continuous with the oesophagus.
- The inner surface of the stomach consists of long folds called rugae.
- The chyme is prepared by digestion of food in the beginning small intestine.
- Parietal cells produce hydrochloric acid and intrinsic factors, and chief cells secrete pepsinogen.
- Gastrin helps to stimulate the secretion of gastric acid.
- The small intestine is the part of the gastrointestinal tract extending between the stomach and the large J intestine. It has three regions—duodenum, jejunum j and ileum.
- The small intestine is the site where digestion and absorption of nutrients are completed. Digestion of all the contents of food—fats, proteins, and carbohydrates occurs in the small intestine to convert them into soluble molecules that can be absorbed,
- The liver is the largest gland in the body and it produces bile, which is a fat emulsifier.
- Bile is a yellowish-green, alkaline solution. It is composed of bile salts, bile pigments, cholesterol, neutral fats, phospholipids and a variety of electrolytes.
- Bile is received by the small intestine from the gall bladder through the common bile duct and pancreatic i juice is received from the pancreas via the pancreatic duct.
- Bile does not usually enter the small intestine until the gallbladder contracts by stimulation of cholecystokinin (CCK).
- Pancreatic juice mainly contains water and enzymes that break down all categories of foodstuffs and electrolytes.
- Pancreatic secretion helps in the neutralisation of the acids present in chyme. It also has enzymes involved in the digestion of carbohydrates, fats and proteins.
- The pancreas is stimulated by secretin to secrete a bicarbonate-rich fluid for neutralising acidic chyme.
- Glycerol and fatty acids enter the epithelial cells of the villi and are packed as lipoprotein droplets. These droplets then enter a lacteal.
- The large intestine comprises of caecum, colon, rectum and anal canal. The diameter of the large intestine is larger than the small intestine.
- The large intestine absorbs water from undigested food residues and eliminates the latter as faeces.
- When the vagus nerve gets damaged, peristalsis within the oesophagus decreases drastically. This condition is known as achalasia.
- The large intestine has thick mucosa, that has crypts with a large number of mucus-producing goblet cells.
- Bacteria enter the colon via the small intestine and anus. They colonise in the colon and ferment some of the indigestible carbohydrates.
- On digestion, carbohydrates form maltose, maltotriose, and a-limit dextrins. These are cleaved by enzymes to monosaccharides and are taken up by enterocytes.
- Enterocytes absorb the lipids. These lipids are packed and secreted as chylomicrons into the lymph.
- On digestion, proteins break down into amino acids, dipeptides, and tripeptides. These are taken up by enterocytes and transported into the blood.
