Neural Control And Coordination Introduction
As you are reading this book, Think about the organs That are Functioning with functioning within you right now! Your eyes are sensing the light reflected off this page.
Your brain is decoding the meanings of the words you are reading. Think about the processes that are running within your body. You are breathing, perhaps perspiring, feeling the chair on which you are sitting, and your heart is beating.
All of these are being regulated by an organ system inside your body. It is the neural system or nervous system.
The nervous system controls various metabolic and physiological functions of the body.
Different organs of the body are directly connected to the nervous system. The actions of these organs are coordinated by the nervous system. This is known as neural coordination.
Read and Learn More: WBCHSE Notes for Class 11 Biology
Neural System
All organ systems of animals are controlled and coordinated effectively by the neural system or the nervous system. The neural system allows the organism to interact with its environment, appropriately.
This system functions at the cellular level through nerve cells or neurons.
It receives sensory information, interprets it, and generates appropriate responses using organs like muscles. The neurons set up the neural system in a number of discrete anatomical locations in the brain.
These systems send and receive impulses from the sense organs and other receptors of the body.
Thus, neural control provides the basis for body functions such as perception of senses, attention, memory, emotions, rational thinking, etc.
Morphology of leaf structure and its modifications
Neural system of different animals
- Sponges (Porifera) do not have any neural system, Hydra (Cnideria) has a neural system that is composed of a network of neurons.
- Planaria (Platyhelminthes) have two nerve cords that converge to form a rudimentary brain.
- The neural system of earthworm (Annelida) is composed of a single nerve cord and paired nerve ganglia.
- The neural system of arthropods is better organized, It consists of the brain, ganglia, and neural tissue.
- The neural system of vertebrates is highly developed.
The nervous system of humans and other advanced vertebrates consists of three parts—
- Brain,
- Spinal cord and
- Nerve.
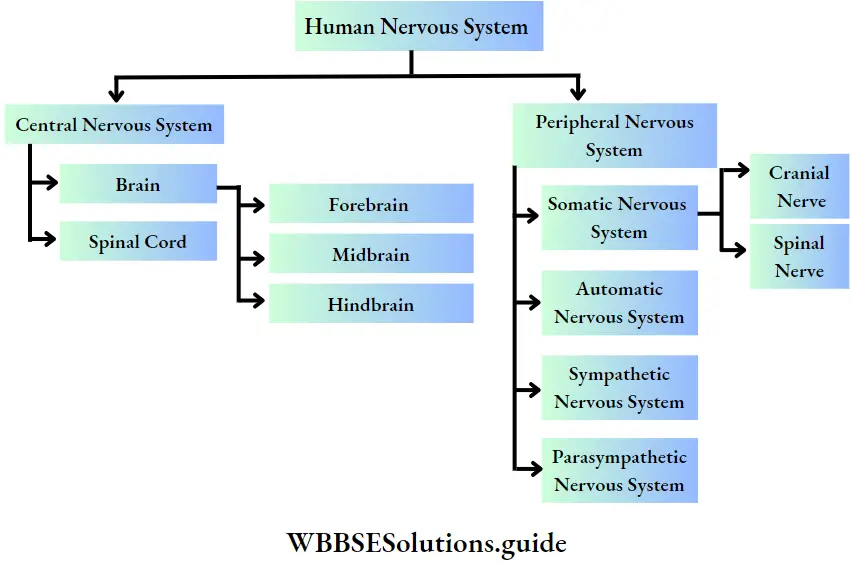
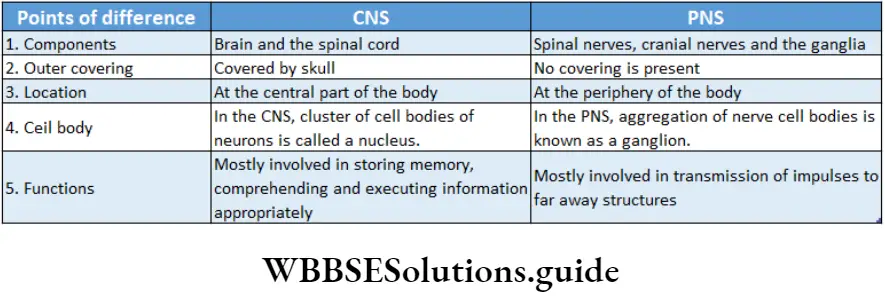
The brain and spinal cord form the central nervous system while nerves form the peripheral nervous system.

Neurons As Structural And Functional Units Of Neural System
Though neurons are the main structural and functional components of the nervous system some other cells also take part in maintaining the proper functioning of this system.
The cells of the nervous system can be divided into two broad categories—
- Nerve cells (or neurons) and
- Supporting cells called neuroglia (or simply glia), are discussed below
Neuron
The human brain alone contains over 100 billion neurons. Each neuron can have up to 10,000 connections to other neurons in the brain.
Types of leaves and their modifications with examples
Neuron Definition: The Structural And Functional units of the nervous system which are capable of Sending and receiving nerve impuluses is called a neuron.
” class 11th biology chapter 21 notes”
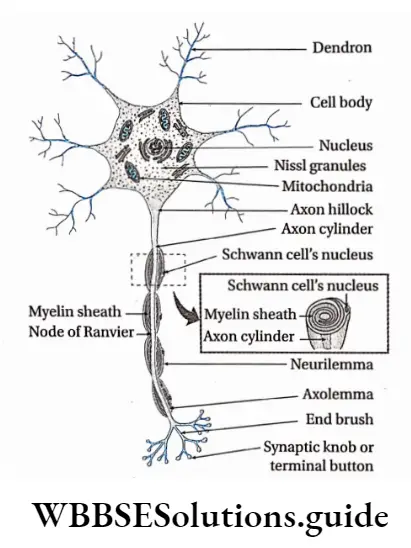
Different Parts Of A Neuron
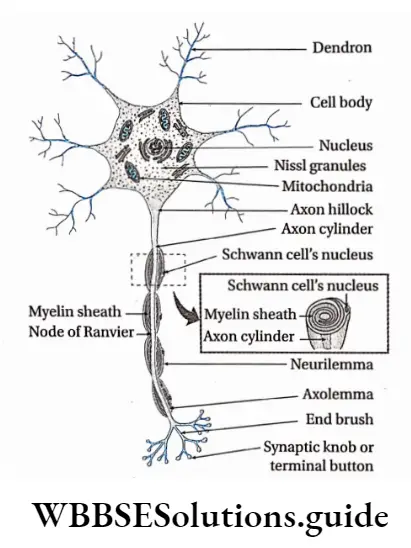
A typical neuron consists of a cell body (perikaryon or soma) and cellular processes called dendrons and axons. Different parts of a neuron are discussed below.
Cell Body or soma or perikaryon or neurocyton: The swollen part of a typical neuron, containing cytoplasm and nucleus, from which cellular processes emerge, is known as the cell body.
Different parts of the cell body are as follows—
- The cell membrane forms the external boundary of the neuronal cell body and its processes. It is also known as a neurilemma.
- The nucleus is located at the center of the cell body. The contents of the nucleus are enclosed within a double-layered nuclear membrane.
- The cytoplasm is known as neuroplastic.
Neuroplasm contains—
- Microtubules—These are hollow rod-like filaments that are composed of a globular protein named tubulin.
- Neurofilaments— These are thinner than microtubules but thicker than microfilaments. They are a major Component Of the neuroral Cytoskeleton.
- Microfilaments— These Are Thinner Than The Neurofilaments. They consist of two intertwined strands, each of which is a polymer of actin protein subunits. They help in the maintenance of cell shape, changing of cell shape, and in cytoplasmic streaming.
- Neurofibrils— Neurofibrils are filamentous structures or microscopic fibrils that are found running in every direction through the nerve cell. They provide the neuron support and help to give it a shape,
- Nissl granules— These are the granular material present throughout the entire cell body and proximal portions of the dendrites. However, it is not present in the axon hillock (a portion of the soma from which the axon arises). The Nissl granules consist of ribosomes and endoplasmic reticulum.
- Centrosome— Nerve cells are incapable of division. So, it is assumed that neurons lack centrosomes. However, under the electron microscope, a non-functional centrosome has been observed,
- Other organelles—The cell organelles, commonly found in animal cells are also present within the neuroplasm. These include the Golgi complex, endoplasmic reticulum, mitochondria, lysosomes, etc.
- Storage material—The cytoplasm of a neuron contains glycogen, lipids, etc., as storage material They consist of two intertwined strands, each of which is a polymer of actin protein subunits. They help in the maintenance of cell shape, changing of cell shape, and in cytoplasmic streaming.
- Neurofibrils— Neurofibrils are filamentous structures or microscopic fibrils that are found running in every direction through the nerve cell. They provide the neuron support and help to give it a shape,
- Nissl granules— These are the granular material present throughout the entire cell body and proximal portions of the dendrites. However, it is not present in the axon hillock (a portion of the soma from which the axon arises). The Nissl granules consist of ribosomes and endoplasmic reticulum.
- Centrosome— Nerve cells are incapable of division. So, it is assumed that neurons lack centrosomes. However, under an electron microscope, a non-functional centrosome has been observed,
- Other organelles—The cell organelles, commonly found in animal cells are also present within the neuroplasm. These include the Golgi complex, endoplasmic reticulum, mitochondria, lysosomes, etc.
- Storage material—The cytoplasm of a neuron contains glycogen, lipids, etc., storage material.
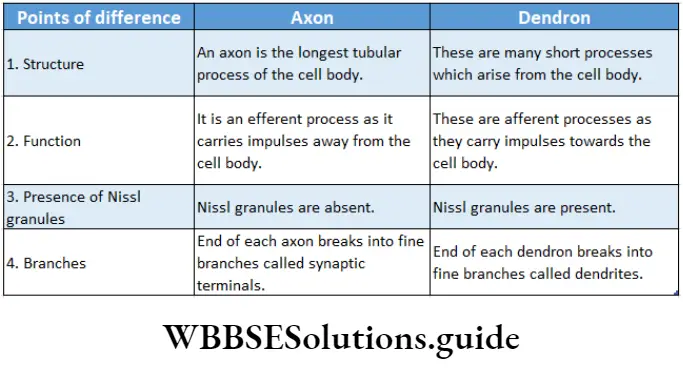
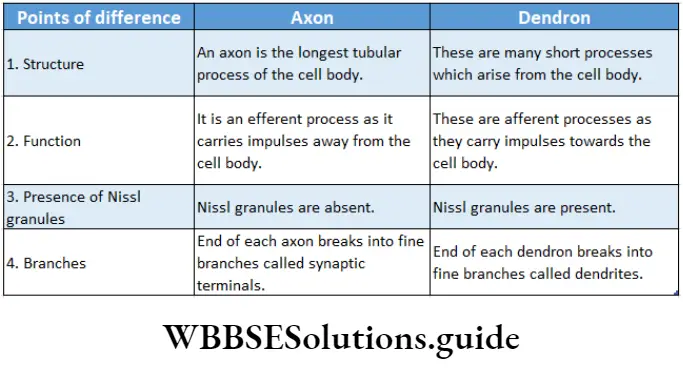
Cellular processes: The cytoplasmic, thread-like appendages that emerge from a cell body are known as cellular processes. These projections are of two types—dendrons and axons.
Dendron: The short cellular processes emerging from the cell body of a neuron that receives impulses from another neuron is called dendron (from the Greek dendron = tree branch).
Dendron Structure:
- The number of dendrons can be from one to many,
- Branches of dendrons are known as dendrites,
- Nissl granules, ribosomes, smooth endoplasmic reticulum, neurofilaments, micro-filaments, microtubules, and mitochondria are present in the dendrites,
- Dendron lacks myelin or medullary sheath.
Dendron Function:
- The dendrite is the impulse-receiving part of the neuron,
- Dendrites increase the surface area for receiving signals from other neurons.
Axon: A long cellular process emerging from a neuron that transmits nerve impulses from the cell body to another neuron is called an axon.
Dendron Structure:
- In most cases, a neuron consists of one axon. Apoiar neuron lacks any axon,
- The plasma membrane of the axon is called the axolemma and its cytoplasm is called axoplasm.
- The axoplasm does not contain the Nissl substance or Golgi apparatus. But the axoplasm does contain mitochondria, microtubules, and neurofilaments,
- Depending upon the presence or absence of myelin sheath around axons, they are either myelinated or non-myelinated, respectively.
- In myelinated axons, the part that lacks myelin forms a ridge due to the fusion of neurilemma and axolemma. This region is called the node of Ranvier. Generally, nodes of Ranvier are distributed at a distance of 1-3.
- At their distal ends, the axons branch extensively. Their terminal ends, which are mostly enlarged, are called synaptic terminals (synaptic buttons)
Neurons are classified into different categories on the basis of certain features which are as follows-
Detailed structure of a leaf with labeled diagram
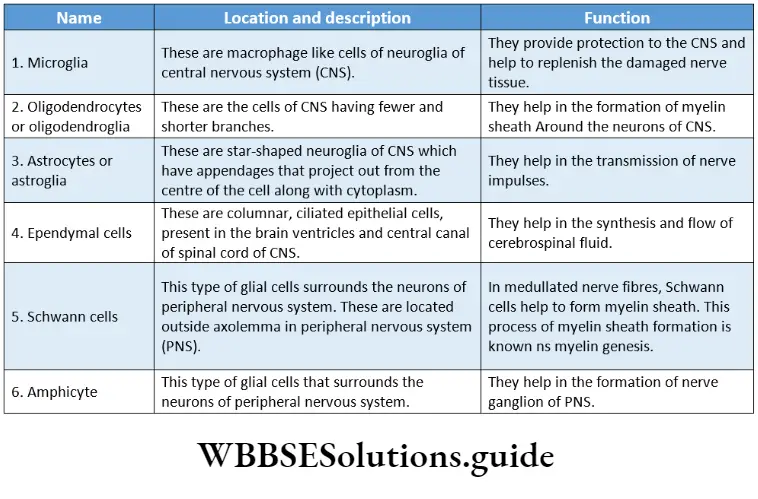
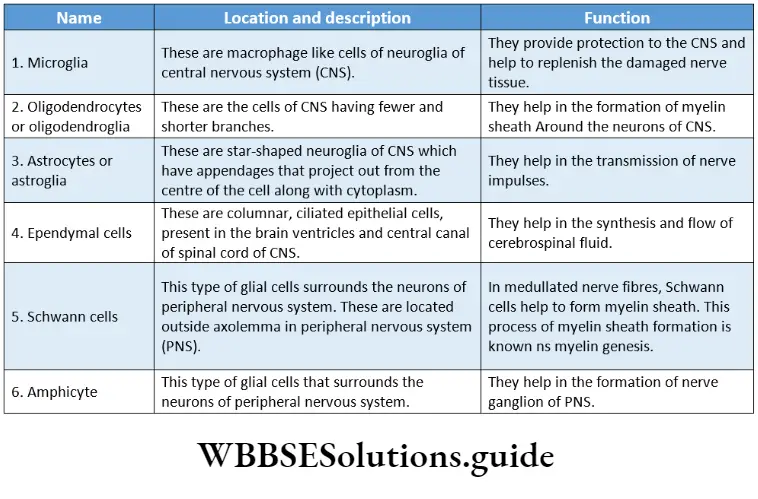
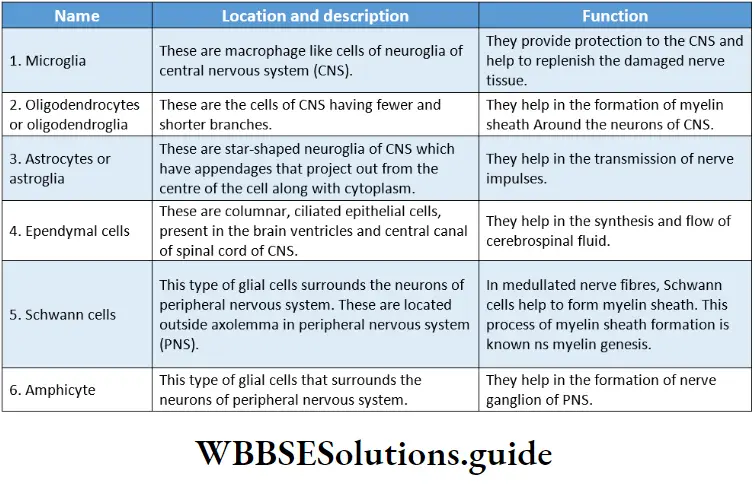
Neuroglia Or Glial Cell
Neuroglia Or Glial Cell Definition: The cells of the nervous system other than neurons that are incapable of generating and transmitting nerve impulses but provide structural and functional support to the neurons are called neuroglia or glial cells.
Neuroglia Or Glial Cell Characterises:
- Neuroglia are incapable of transmitting nerve impulses.
- These cells can divide (unlike nerve cells).
- The brain contains more neuroglial cells than neurons.
- The appendages of some glial cells (astrocytes) are thinner at their terminal end and form special structures called end-feet that remain associated with blood capillaries.
Ganglion
The region outside the CNS where there is an aggregation of numerous nerve cell bodies, is known as ganglion.
Ganglion Example: 31 pairs of nerves have originated from the human spinal cord. Two main nerve roots—dorsal nerve root and ventral nerve root, combine to form spinal nerves.
But before their meeting point, a thinner region is seen where numerous neurons remain associated with each other. This region is known as the dorsal ganglion.
Nerve
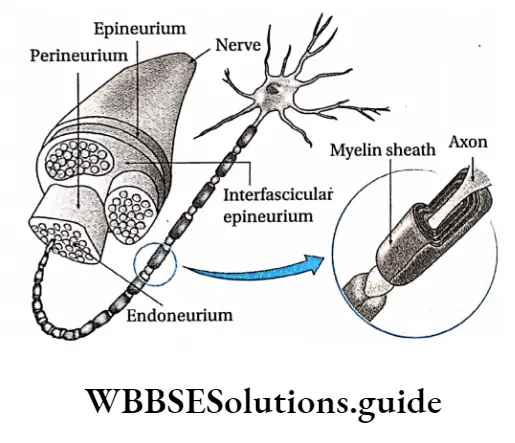
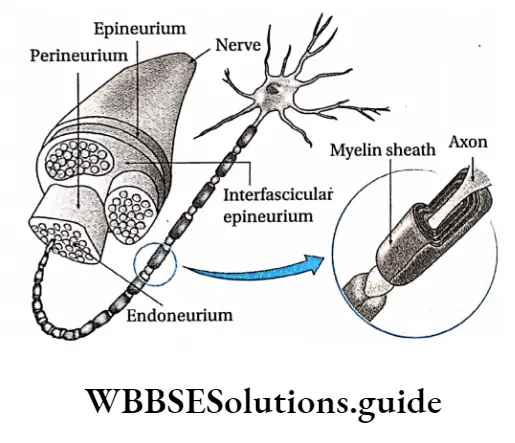
Nerve Definition: A cord-like structure, comprising a collection of neurons, blood vessels, lymph vessels, and adipocytes enclosed by a layer of connective tissue, that conveys impulses throughout the body is called a nerve.
Structure Of Nerves
Nerves emerge from the brain and spinal cord and branch out to almost all parts of the body. The nerves are composed of nerve fibers or neurons.
These nerve fibers are bundled together like strands of an electric cable enclosed within a connective tissue covering.
Connective tissue coverings: On the outer side of the nerve, there is a covering made up of connective tissue.
- Blood vessels, lymph vessels, and adipocyte cells are found within it.
- This covering consists of three layers—endoneurium, perineurium, and epineurium.
Endoneurium: It is the innermost layer that covers up the individual nerve fibers. This layer is relatively thin.
Perineurium: A collection of nerve fibers that are individually bound by endoneurium, is again surrounded by another connective tissue layer called the perineurium.
The bundle of nerve fibers bound together by perineurium is called fasciculus (plural: fasciculi).
Epineurium: Several fasciculi are again bound together by another layer of connective tissue. It is called epineurium. It is the outermost layer of connective tissue layer covering the nerve.
This layer is usually thick and rich in blood vessels, lymph vessels, adipocytes, and collagen fibers.
Parts of a leaf and their functions in plants
Nerve fibers: A nerve may have a few to more than a million nerve fibers. These are actually axons of different neurons. Several of these fibers remain bound together beneath the connective tissue coverings.
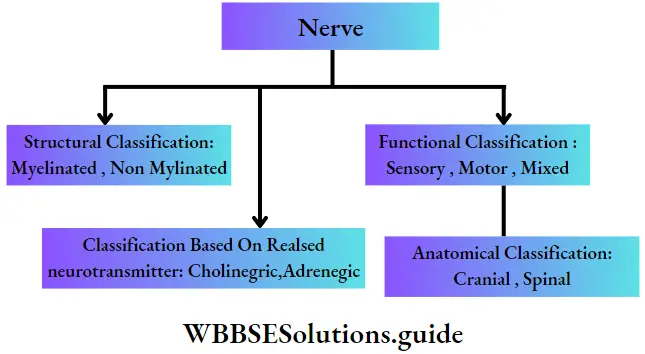
Types Of Nerves
Nerves are of different types. Their classification on the basis of several criteria has been discussed below
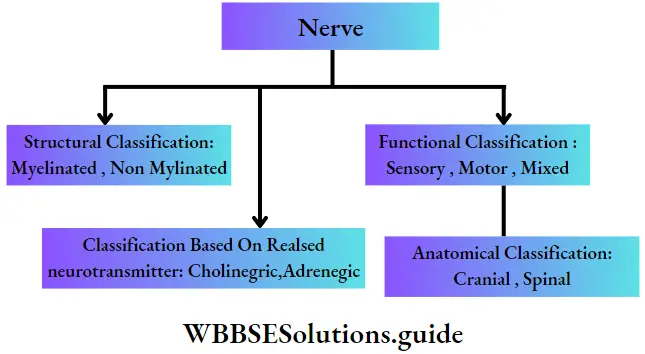
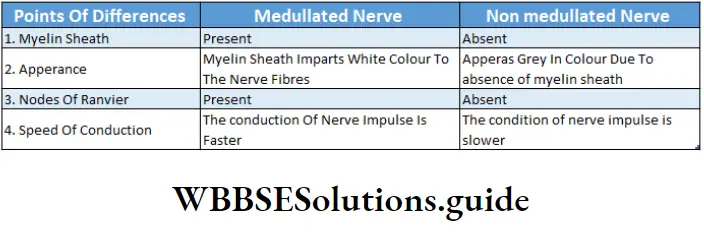
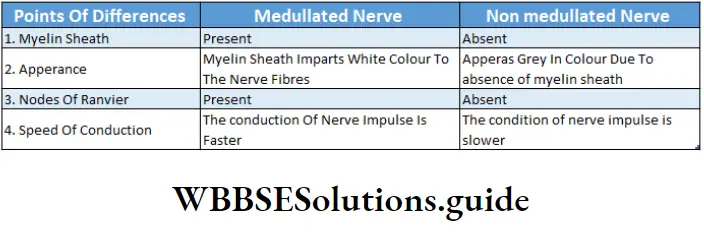
Structural classification of nerves: Based on the presence or absence of myelin sheath, nerves are classified as—
Myelinated nerve: Medullated or myelinated nerves are nerves with large diameters. The nerve fibers of medullated nerves remain wrapped with a protein-lipid sheath called myelin sheath, through which nerve impulse is conducted rapidly.
This type of nerve is made of nerve fibers consisting of three main components. These components are—
- Axis cylinder— It is the central core of the axon of a neuron. There is a thin covering called an axolemma that surrounds the axon. The axolemma is again enclosed by an outer covering called a myelin sheath.
- Myelin sheath—It is an external covering of the axon. It is made up of protein and lipids. It provides insulation to the nerve fiber and hence prevents the spreading of nerve impulses to adjacent tissues. In the nerves of the peripheral nervous system (PNS), the myelin sheath is produced by a type of glial cell called Schwann cell. Nodes of Ranvier are present in this type of nerve.
- Neurilemma—There is another covering external to the myelin sheath, which is called neurilemma.
Example: This type of nerve fiber is found in the white matter of the central nervous system.
Non-myelinated nerve: Non-medullated or non-myelinated nerves are nerves of small diameter. The nerve fibers of these nerves are devoid of the myelin sheath. Through these nerves, a nerve impulse is conducted very slowly. This type of nerve fiber is covered with an external neurilemma. They are devoid of nodes of Ranvier.
Example: This type of nerve fiber is found in the grey matter of the central nervous system.
Functional classification of nerves: Based on the functions carried out by nerve fibers, nerves are classified into three kinds. These are—
Sensory nerves: These nerves contain sensory fibers. Sensory nerves carry impulses from sense organs to the brain or the spinal cord. These nerve fibers are also called afferent nerve fibers. The nerve impulse conducted by sensory nerve fibers is called sensory impulse.
Examples of sensory nerves are—the olfactory nerve, optic nerve, auditory nerve, etc fibers.
Sensory nerves carry impulses from sense organs to the brain or the spinal cord. These nerve fibers are also called afferent nerve fibers. The nerve impulse conducted by sensory nerve fibers is called sensory impulse.
Examples of sensory nerves are—the olfactory nerve, optic nerve, auditory nerve, etc.
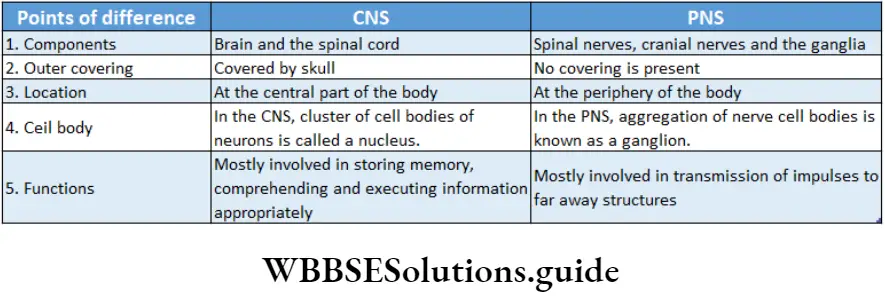
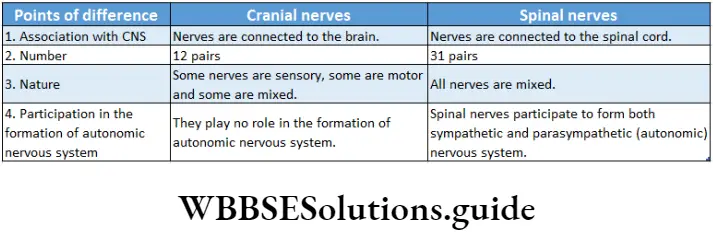
Anatomical Classification: Based on the anatomical origin of nerves, these are classified as—
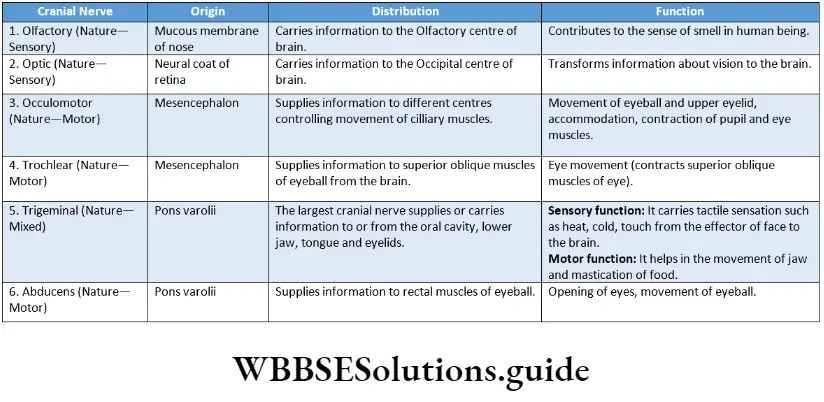
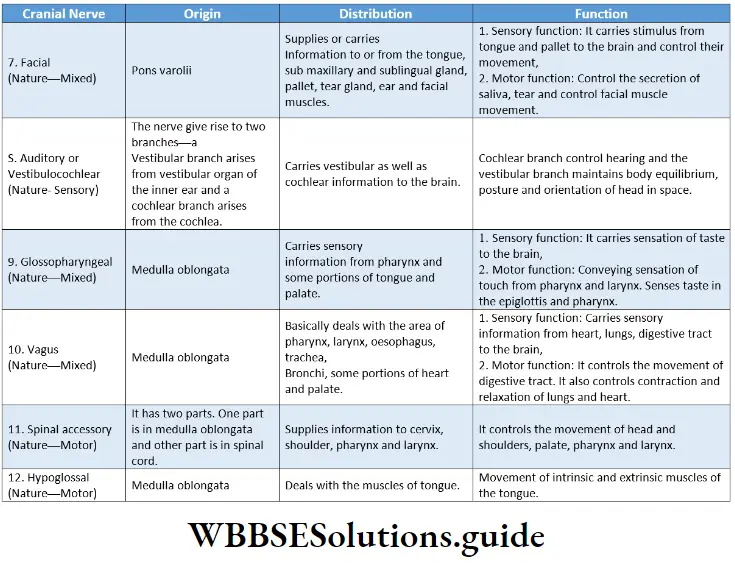
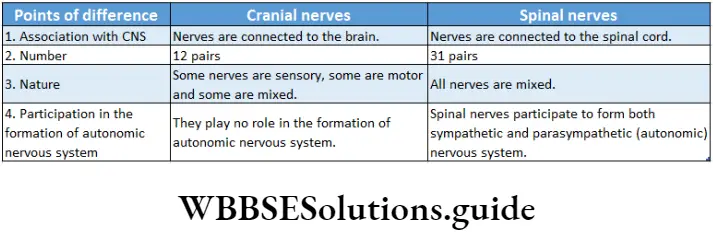
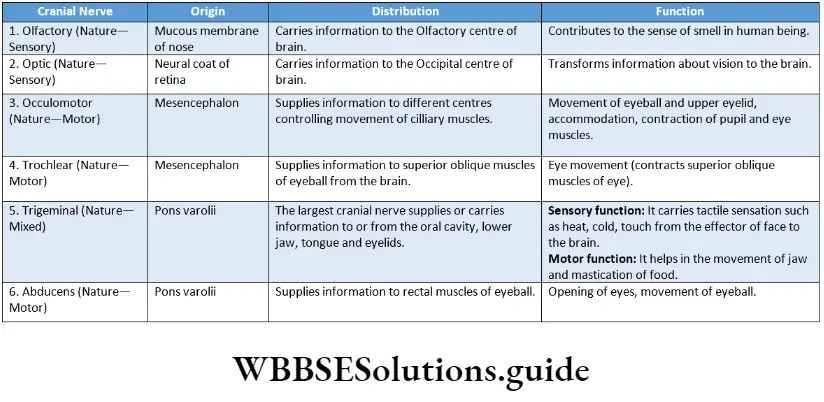
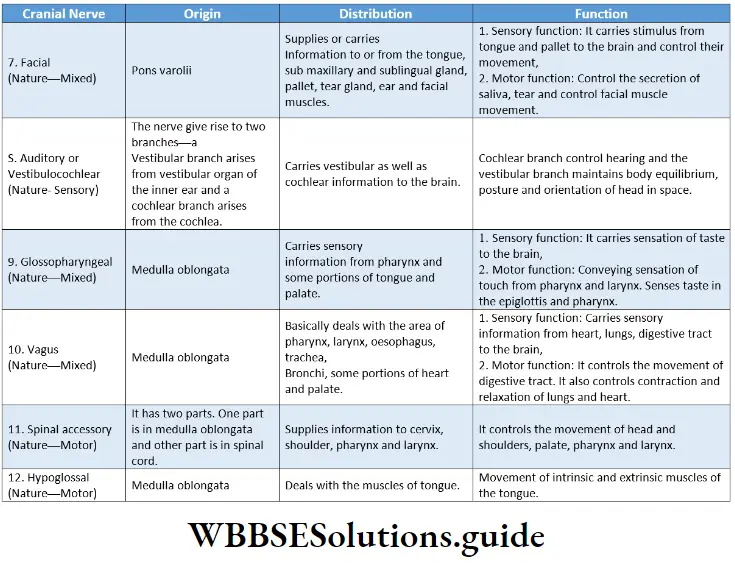
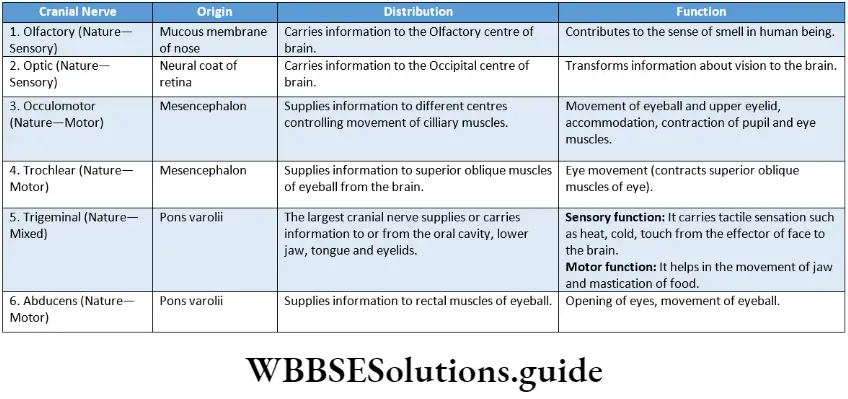
Cranial nerves: These nerves originate from the brain. They may be entirely motor-sensory or mixed.
The human nervous system consists of 12 pairs of cranial nerves.
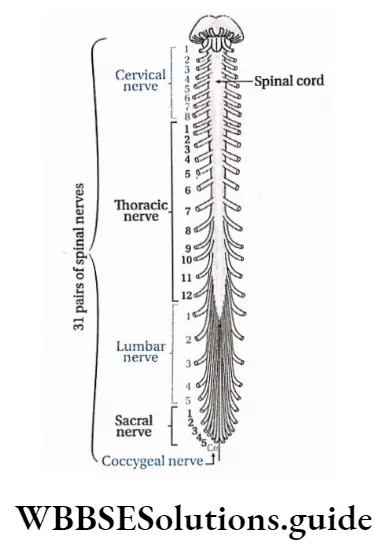
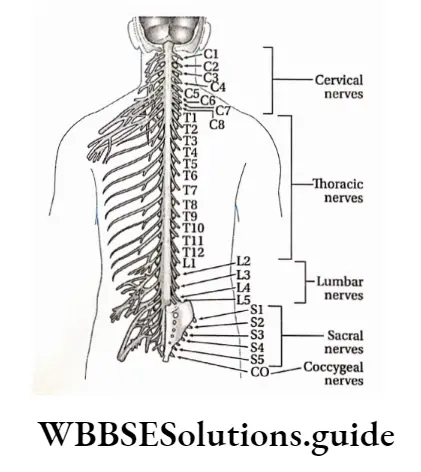
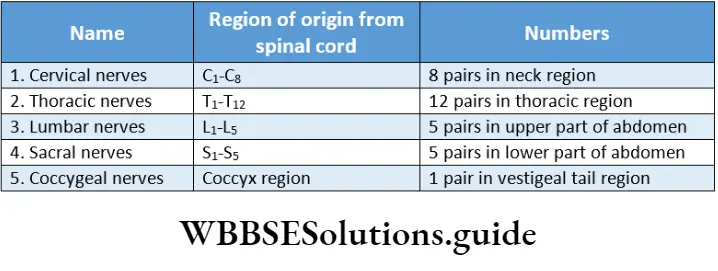
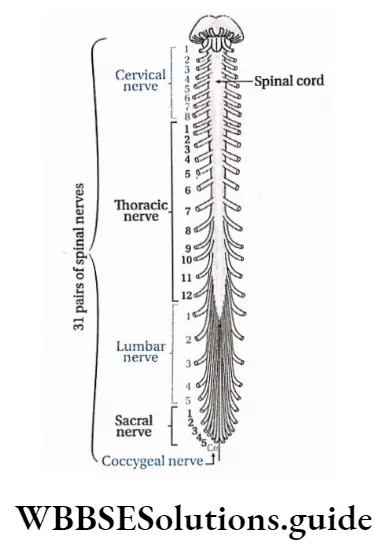
Spinal nerves: It is always of a mixed type originating from the spinal cord. The human nervous system consists of 31 pairs of spinal nerves.
Classification based on neurotransmitter: Based on neurotransmitter released, nerves are classified as—
Adrenergic nerves: These nerves synthesize and release adrenaline and nor-adrenaline.
Cholinergic nerves: These nerves synthesize and release acetylcholine (ACh).
“class 11 neural control and coordination “
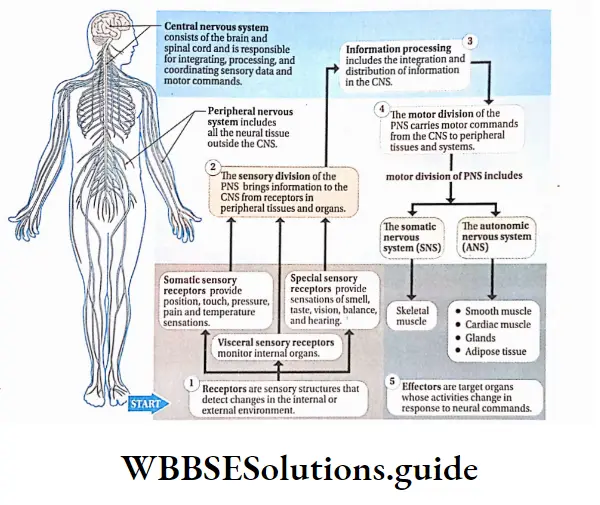
Nervous System In Humans
The nervous system in the human body is an organ system that coordinates the functioning of all the systems of the body and helps the body to respond to external stimuli.
Functions Of Nervous System
The main functions of the nervous system in humans and other animals are described below.
Response to external stimuli: The human nervous system is equipped to sense and respond to continuous changes within the body and in its external environment.
Control and coordination: The nervous system works along with the endocrine system to communicate, integrate, and coordinate the functions of various organs and organ systems in our body. It also helps the body to respond to the external stimuli.
Higher mental functions: It also acts as a seat of self-consciousness, intelligence, thoughts, and emotions.
Maintenance of balance with the environment: Humans And Other higher animals sense the changes in the environment and Act Accordingly, Both with the help of the nervous System.
Control of reflex action: Grey matter of the spinal cord, within the central nervous system, controls the reflex actions of the body.
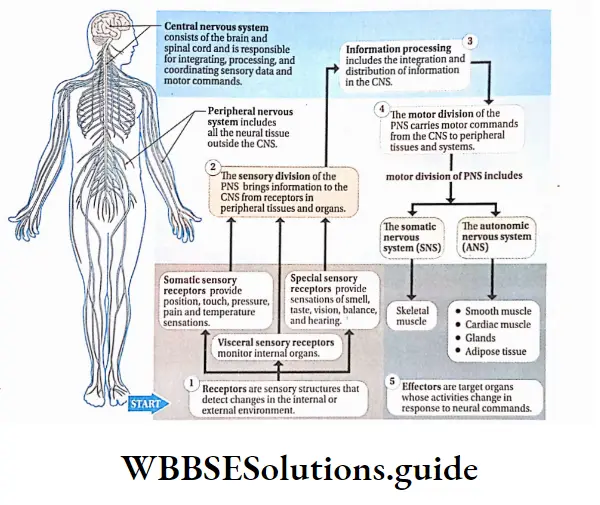
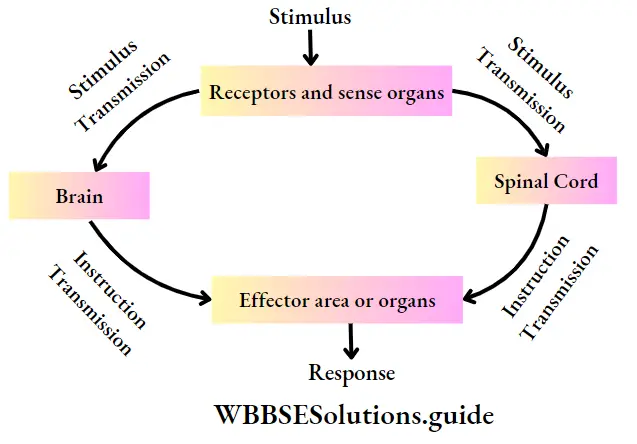
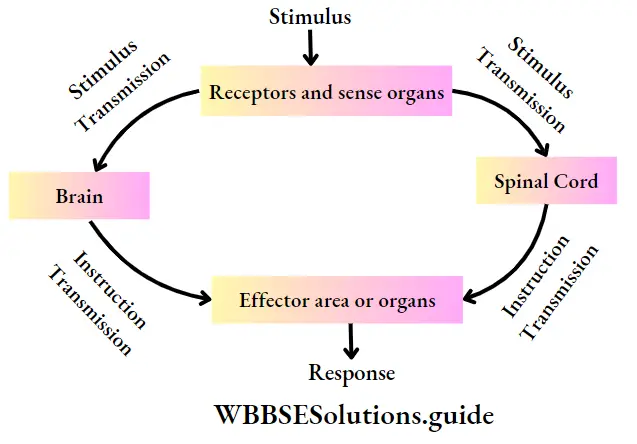
Mechanism Of Action Of The Nervous System
The action of the nervous system is accomplished in some stages. These are—
Receiving stimulus: Mechanical, chemical, or physical changes that excite the body or body parts, are known as stimuli.
Stimulus is received by the receptors present in the eyes, ears, nose, tongue, skin, and other parts of the body.
Transmission of impulse to the central nervous system: The received stimulus is transmitted to the central nervous system as a sensory nerve impulse, by sensory nerves.
Sending instructions from the central nervous; system to the target site: The sensory information is analysed in the brain and spinal cord of the central nervous system.
Instruction for necessary action is then sent as a motor impulse, through the motor nerves, to the effector organizer
The accomplishment of action: As per instruction from the central nervous system, actions are completed in the effector area or organizer:
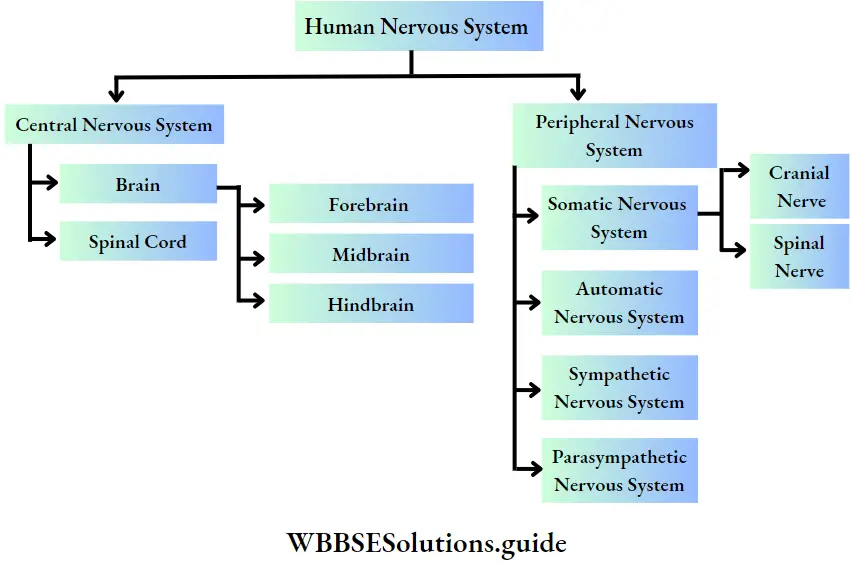
Divisions Of Human Nervous System
The human nervous system comprises the following divisions—
” neural control and coordination notes pdf download”
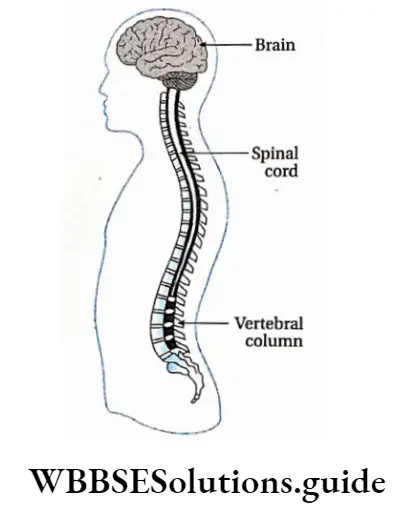
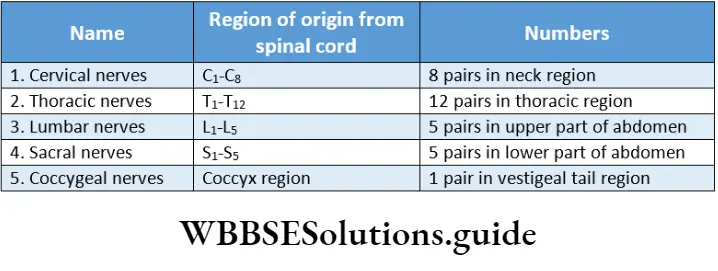
Central Nervous System
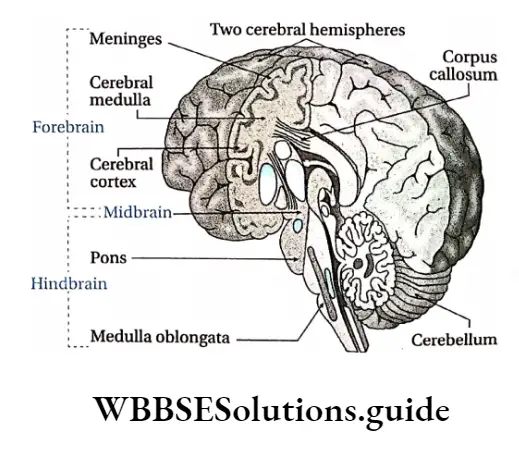
Central Nervous System Definition: The structural and functional center for the entire nervous system comprising the brain and spinal cord is called the central nervous system or CNS.
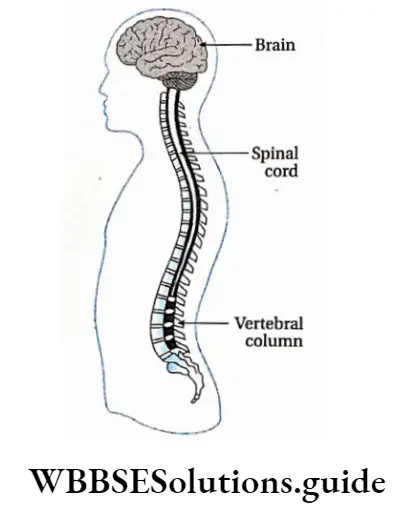
Central Nervous System Characteristic features:
- The components of the CNS are the brain and the spinal cord.
- The brain is located within a bony cavity called the cranium or brain box. The dorsal part of the brain bears an opening called the foramen magnum.
- Through this opening, the spinal cord enters the vertebral column. The spinal cord is present within the neural canal of the vertebral column. It runs upto the end of the vertebral column.
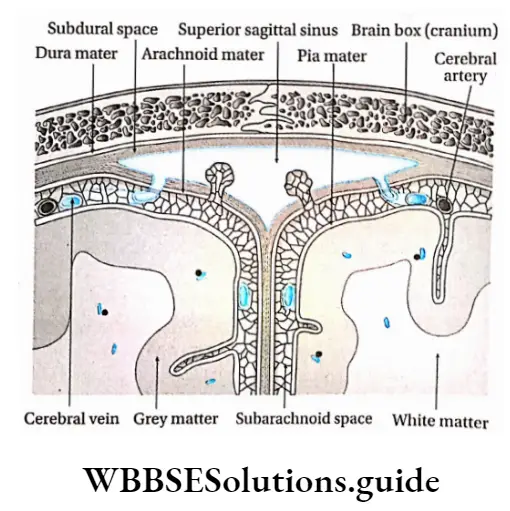
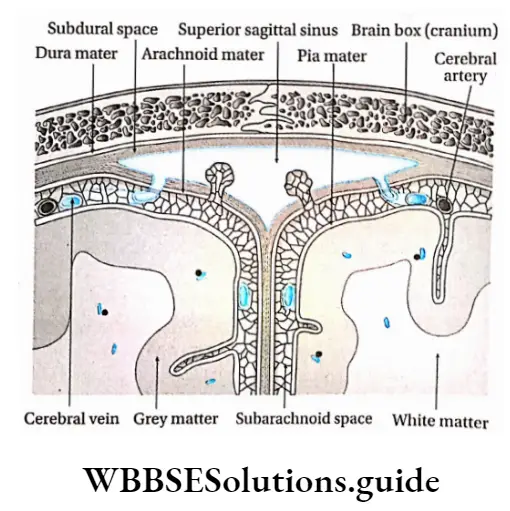
- Outside the CNS, three layers of protective tissues are present, which are referred to as meninges.
- These meninges surround the brain and the spinal cord providing additional layers of protection to. The three layers of meninges are—
- Dura mater,
- Arachnoid mater and
- Pia mater.
- The space between the dura mater and the arachnoid mater is called subdural space.
- The small space between the arachnoid mater and the pia mater is called subarachnoid space. Within this space cerebrospinal fluid (CSF) is present.
- At the end of the spinal cord, the pia mater extends upto the coccyx like a thin thread, termed filum terminale. This part is composed of fibrous connective tissue.
- Human CNS has grey matter and white matter beneath the layer of meninges. In the CNS of the brain, the white matter lies beneath the grey matter.
- But in the spinal cord, the grey matter lies beneath the white matter. CNS of vertebrates comprises four brain ventricles. The spinal cord consists of one central canal or neurocoel.
- Note that brain ventricles (chambers within the brain) and central canal or neuronal are completely filled by cerebrospinal fluid (CSF).
- Within CNS, grey matter is present like an island in white matter. This is known as the nucleus.
Central Nervous System Structure: The central nervous system is mainly composed of two parts—the brain and the spinal cord. These are described below in detail.
Brain Ventricles
- The human brain contains four connected cavities called brain ventricles. The cerebrum of the forebrain has two cerebral hemispheres.
- The first and second ventricles are located there laterally and are called lateral ventricles.
- The diencephalon of the forebrain includes two parts—the hypothalamus and epithalamus.
- The third ventricle is present between the epithalamus and the hypothalamus and is connected to the lateral ventricles by an interventricular pore, known as the foramen of Monroe.
- The fourth ventricle is located within the cerebellum and pons of the metencephalon of the hindbrain.
- The fourth ventricle is connected to the third ventricle by a tubule called the aqueduct of Sylvius.
- The fourth ventricle remains connected to the central canal of the spinal cord. Two holes are present in the fourth ventricle—the foramen of Lusaka and the foramen of Magendie.
- Through these pores, the cerebrospinal fluid moves upward to enter into the subarachnoid space.
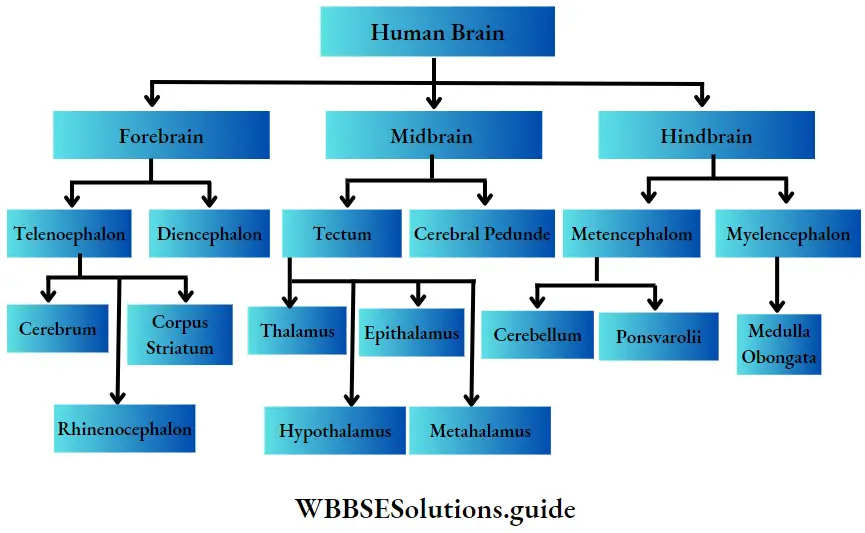
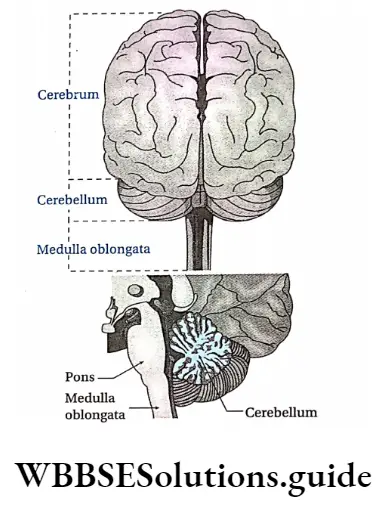
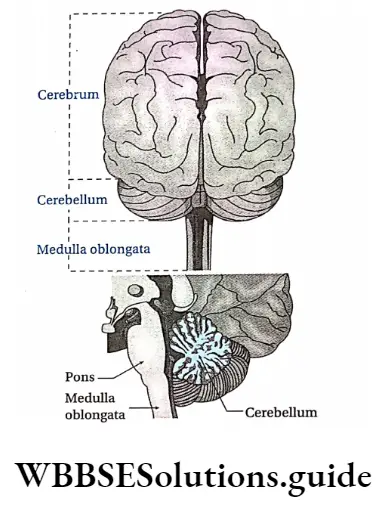
Brain
Brain Definition: The swollen part of the central nervous system located in the brain box, having cavities filled with CSF and Procted By meninges, is called Brain.
Brain Location: The brain is located in the cranial cavity of the human skull.
Brain Structure: The brain of vertebrates is made up of 100 billion neurons and a large number of neuroglia.
The approximate weight of an adult human brain is 1.36 kg. The different parts of the human brain are shown below in the given chart.
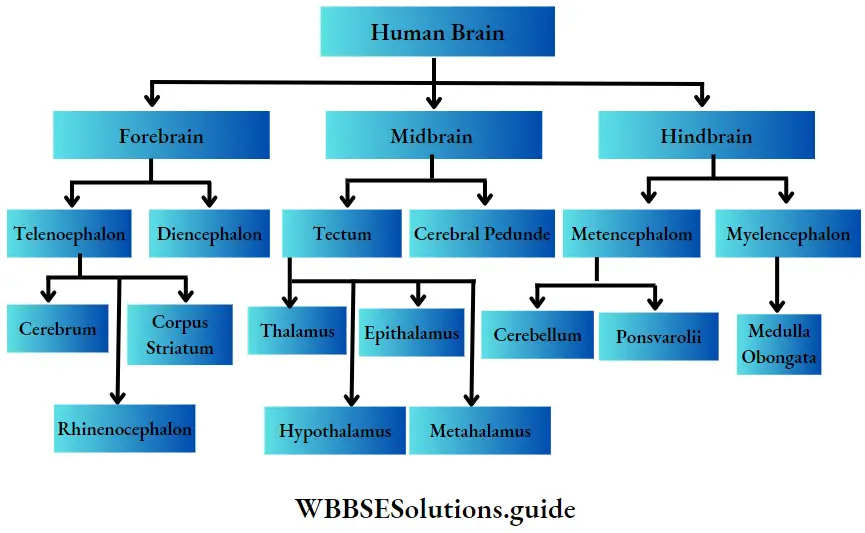
Forebrain or Prosencephalon
The forebrain has two subdivisions—the telencephalon and the diencephalon.
Telencephalon: Telencephalon is again subdivided into three parts namely, cerebrum, corpus striatum, and rhinencephalon.
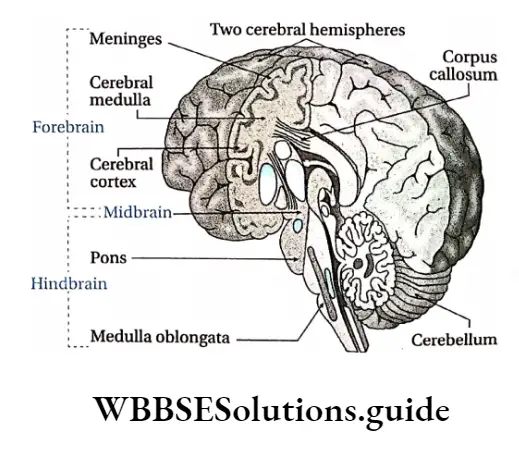
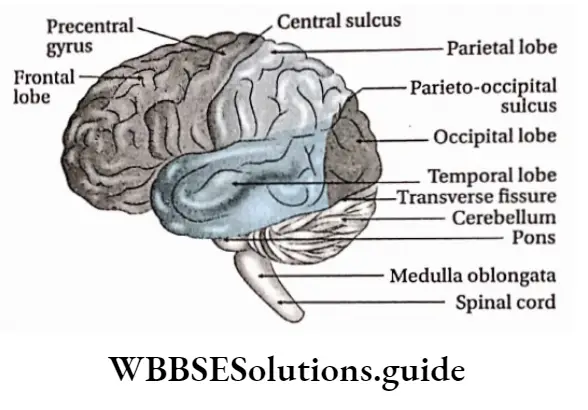
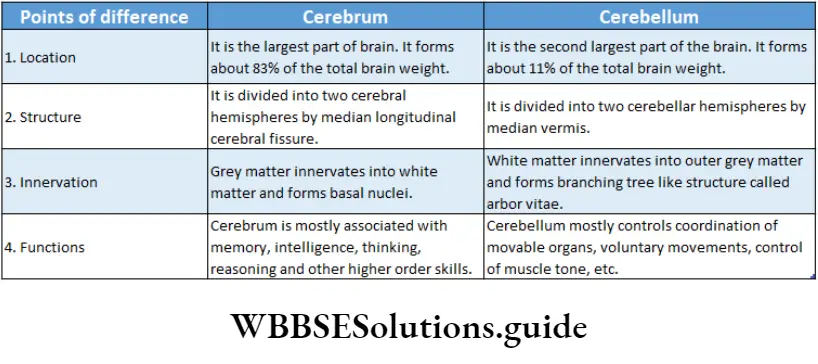
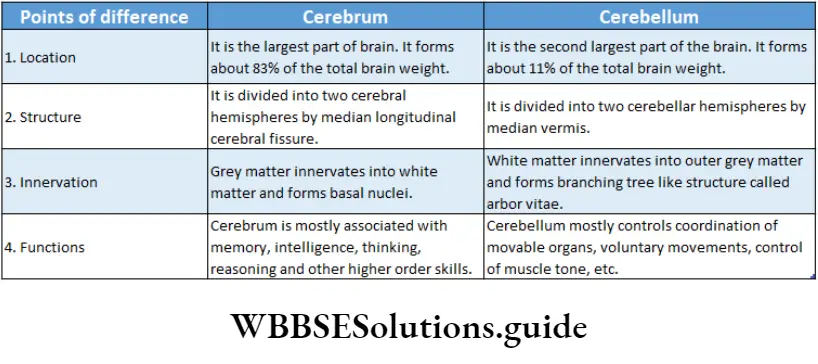
Brain Structure: Cerebrum is divided into two symmetrical semicircular parts called cerebral hemispheres.
The surface area of the cerebral hemisphere is greatly folded, accommodating several layers of neurons.
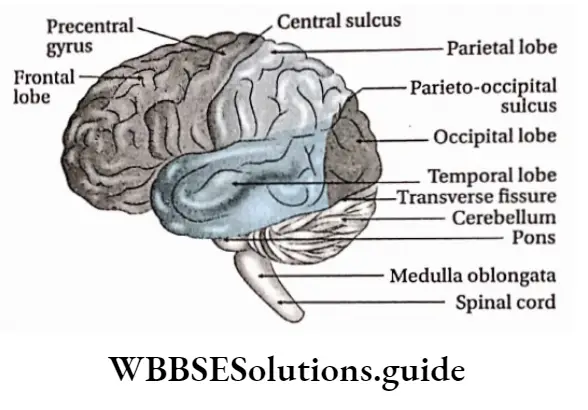
This area is called the cerebral cortex. Each fold is known as gyrus (plural: gyri) and the groove or depression between them is called sulcus (plural: sulci).
Deep and wide sulci are called fissures. Fissures divide the cerebral hemisphere into a number of lobes.
These are—
- Frontal lobe,
- Parietal lobe,
- Occipital lobe,
- Temporal lobe.
The fissure between the frontal and parietal lobes is called the fissure of Rolando or central sulcus.
The fissure between the parietal and temporal lobes is known as the Sylvian fissure. The fissure between the parietal and occipital lobe is called the parieto-occipital fissure.
Beneath the cerebral cortex, there lies the cerebral medulla. It is made up of white matter which is mainly composed of nerve fibres.
The two cerebral hemispheres are linked by a bundle of longitudinal nerve fibers called the corpus callosum. The cerebrum contains pyramidal (Betz), stellate, and spindle neurons.
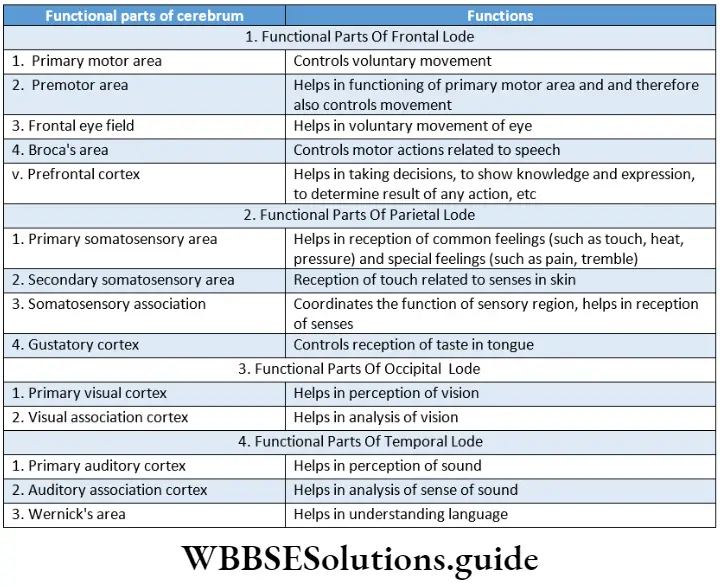
Brain Functions:
The cerebrum controls the action of different voluntary muscles, the movement of eyelids and eyeballs,
Different areas of the cerebral cortex control our ability to speak (Broca’s area) and write (Wernicke’s area),
The temporal lobe contains the auditory cortex and is involved in auditory perception,
Similarly, the occipital lobe contains the visual cortex and is responsible for visual processing.
Different areas of the cerebral cortex are also responsible for the perception of other sensations like taste, smell, touch, pressure, pain, heat, and cold.
The cerebrum is the center for memory, intelligence, judgment, conscious thought, and other activities associated with thinking and feeling.
Corpus striatum: It is made of grey matter suspended within white matter within the cerebrum.
This part of the brain constitutes a structure called basal ganglia. The Corpus striatum helps in the modification of functions of the motor region in the cerebrum.
Rhinencephalon: The ring-like structure around the brain stem is known as rhinencephalon. The rhinencephalon helps in sensing smell.
Limbic System
The system that is composed of parts of the telencephalon, diencephalon, and mesencephalon and is expanded at the periphery of the cerebral cortex and diencephalon, controlling human emotions, feelings, inspiration, etc., is called the limbic system. The term limbic’ means border or boundary.
The parts of the diencephalon that are associated with the limbic system are—the hypothalamus and the nucleus of the frontal thalamus.
The parts of the telencephalon such as the amygdala, hippocampus, septal nuclei, para-olfactory lobe, and limbic cortex form the structural components of the limbic system. Other than these, reticular formations of the midbrain are also associated with the limbic system.
In human beings, the primary function of the limbic system is to control emotions such as fear, hopelessness, anger, depression, happiness, etc.
Diencephalon: It is located between telencephalon and mesencephalon. The diencephalon is situated between the two cerebral hemispheres.
It has four parts, namely—hypothalamus, epithalamus, metathalamus, and thalamus.
Hypothalamus: It is a small cone-shaped structure of the brain lying below the thalamus. It makes up the floor of the third cerebral ventricle projects downwards from the brain and ends in the pituitary gland.
Location: The hypothalamus is located below the thalamus, just above the brain stem, and anterior to the third ventricle.
Structure: Hypothalamus consists of numerous neurosecretory cells. Near infundibulum (pituitary
Limbic System Structure: Hypothalamus consists of numerous neurosecretory cells. Near the Infundibulum (pituitary stalk) of the hypothalamus, two optic nerve crosses each other.
This region of crossing is known as optic chiasma. The hypothalamus also consists of numerous hypothalamic nuclei.
Limbic System Function:
- The hypothalamus plays a significant role in the regulation of body temperature (thermoregulation),
- The hypothalamus regulates our appetite and feeding behavior,
- The hypothalamus also helps in the maintenance of water balance in our body.
- The hypothalamus also helps to maintain the normal functioning of the cardiovascular system.
- The hypothalamus regulates the action of the autonomic nervous system,
- The neurosecretory cells situated in the hypothalamus secrete neurohormones.
- These act as releasing factor or inhibitory factor, that controls the secretion of different hormones from adenohypophysis or anterior pituitary
- The hypothalamus helps to regulate circadian rhythm. Different functions of our body like sleep, wakefulness, etc., take place in a cyclic way following the day-night cycle.
- This rhythm inside our body is called circadian rhythm,
- The hypothalamus is also involved in the expression of emotions like rage, fear, and extreme anxiety.
Epithalamus: It is a small region in the diencephalon.
It is located in the posterior (dorsal) segment of the diencephalon (superior and posterior to the thalamus). It is connected to the pineal gland and epiphysis by a stalk.
The functions of the epithalamus are—
- It controls the function of the pineal gland.
- It plays an important role in receiving smell impulses and analyzing them.
Thalamus: It is a mid-line symmetrical structure of two halves, within the brain, situated near the center of the brain, superior to the mid-brain.
The thalamus consists of a large mass of grey matter and is located on both the lateral walls of the third ventricle.
The thalamus acts as a relay station for sensory impulses such as pressure, temperature, touch, pain, etc. From there, the impulses are retransmitted to the different areas of the cerebral cortex.
Metathalamus: It is a small region located at the extreme dorsal end of the brain. It consists of the two, paired, lateral and medial geniculate bodies. The metathalamus lies between the epithalamus and the hypothalamus.
The functions of the metathalamus are—
The medial geniculate body of the metathalamus acts as a relay station of audition i.e., it helps us to hear.
The lateral geniculate body of the metathalamus acts as a relay station of vision i.e., it helps us to see.
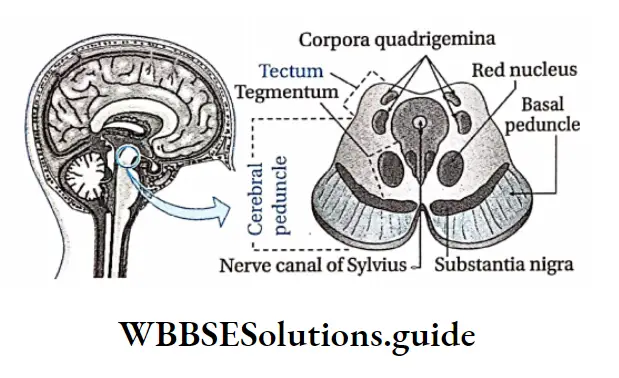
Midbrain or Mesencephalon
The midbrain is located between the diencephalon and mid-region of the hindbrain. It is the smallest part of the human brain. It is almost not visible from the outside. It consists of two parts, namely— tectum and cerebral peduncle.
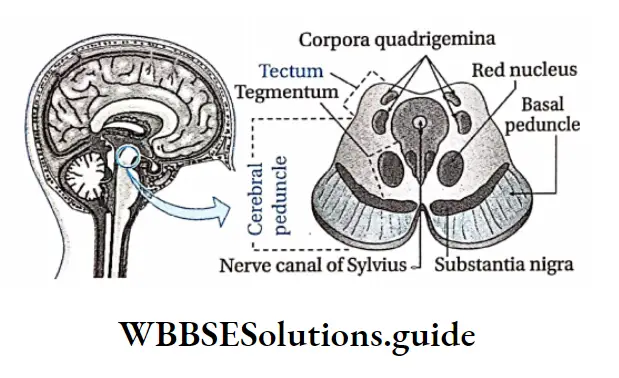
Tectum: The tectum of the midbrain is located in the dorsal region of the aqueduct of Sylvius. The primary structure of the tectum includes two swollen regions— superior colliculi and inferior colliculi.
The superior colliculi forms part of the visual system. The inferior colliculi is a part of the auditory system.
The structures appear as four small bumps on the brain stem. These bumps are together known as corpora quadrigemina.
Simple and compound leaf types with examples
Cerebral peduncle: The cerebral peduncles (or crus cerebri) are located anterior to the aqueduct of Sylvius in the midbrain.
From the interior, three layers are the visible tegmentum, substantia nigra, and basal peduncle.
Due to the presence of melanin pigment, the substantia nigra appears black or brown.
Function Of Midbrain:
- It coordinates the actions of different regions of the midbrain, forebrain, and hindbrain.
- The tectum region of the midbrain coordinates the reflex actions related to visual perception and olfaction.
- The midbrain plays an important role in controlling the body temperature.
- The red nucleus of the midbrain controls muscle tone.
- The midbrain controls the actions of different voluntary muscles.
Hindbrain Or Rhombencephalon
It is located at the posterior end of the midbrain. It consists of two parts metencephalon and myelencephalon.
Metencephalon: The Metencephalon is located in the posterior region of the hindbrain.
It has two parts— the cerebellum and the pons.
Cerebellum: Cerebellum is a major structure located at the top of the brain stem (where the spinal cord meets the brain) and at the back portion of the brain, lying under the occipital and temporal lobes of the cerebral cortex.
The cerebellum is the most important and largest part of the human hindbrain. It is also known as the ‘little brain’ or the ‘tree of life’.
Cerebellum Structure: Cerebellum is made up of two hemispheres called cerebellar hemispheres. Two cerebellar hemispheres are connected by a mid-region named vermis. The cerebellum contains Purkinje cells.
Cerebellum Functions:
- The cerebellum plays an important role in controlling body balance,
- The cerebellum controls the movement of the hands and legs. It receives impulses from the cerebral cortex. Depending on these impulses, it controls the movement of the hands and legs.
- The cerebellum controls voluntary movement.
- The cerebellum exerts control over the reflex arc involving muscles. In this way, it helps to maintain normal muscle tone.
Pons Varolii:
- Pons Varolii is a region in the brain stem that lies between the midbrain (above) and medulla oblongata (below) and in front of the cerebellum.
- The ventral part of the pons is convex and the dorsal part is plain. Pons is connected to 5, 6, 7, and 8 cranial nerves.
The main functions of pons Varolii are as follows—
- Pneumotaxic and apneustic centers of pons act as respiratory centers for the regulation of respiration.
- Pons serve as a relay station between several areas of the brain.
- The nerve center of pons Varolii conducts contraction of the detrusor muscle of the urinary bladder, in order to carry out urination.
Myclencephalon or medulla oblongata:
- The medulla oblongata is a cone-shaped structure located in the hindbrain, anterior to the cerebellum, below the pons, and above the foramen magnum. It is the lowest part of the hindbrain.
- The medulla oblongata constricts at the posterior end and appears like a cone. Its length is approximately 2.4 cm. The spinal cord arises from its posterior end.
- Cranial nerves 9, 10, 11, and 12 remain connected to it. Medulla oblongata consists of different nerve centers, such as—the vasomotor center, respiratory center, vomiting center, and salivary center.
Pons Varolii Functions:
- Medulla oblongata controls visceral reflexes such as—sneezing, coughing, vomiting, secretion of saliva, engulfing, etc.
- Medulla oblongata plays an important role in controlling respiration.
- Medulla oblongata plays an important role in controlling the action of the cardiovascular system including the heartbeat.
CSF Or Cerebrospinal Fluid
Cerebrospinal Fluid Location: CSF is present in the neuronal of the central nervous system and central canal of the spinal cord.
It is also present in the subarachnoid space of the meninges.
Cerebrospinal Fluid Origin: The first and second ventricles of the human brain have ciliated epithelium on their wall.
The wall has enough capillary-rich area known as choroid plexus. Plasma of the blood, in the capillaries of the choroid plexus, enters the brain ventricles by diffusion and forms CSF.
CSF content: The total CSF content of a human body is approximately 150 ml.
Components: CSF is clear, and slightly alkaline in nature (pH—7.33). The various components of CSF are—water, plasma proteins, glucose, mineral salts or ions, creatinine, etc.
Cerebrospinal Fluid Functions:
- It acts as a shock absorber and protects the brain from mechanical injury,
- It maintains the shape and structure of the brain by maintaining an outward pressure,
- It transports nutrients to the tissues of the brain and spinal cord,
- It moistens the brain and spinal cord and enables the exchange of substances within I nerve cells,
- It has white blood corpuscles that protect the brain from infections,
- CSF provides buoyancy to the brain.
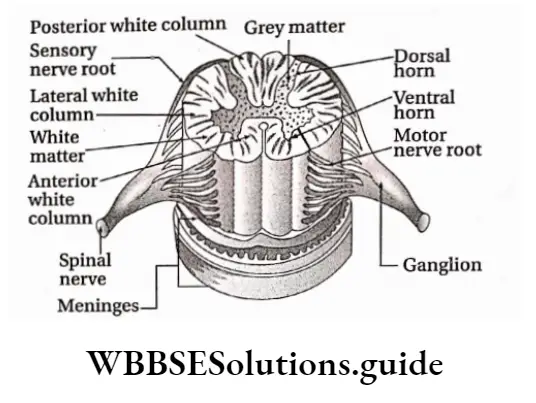
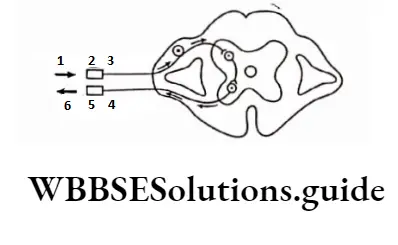
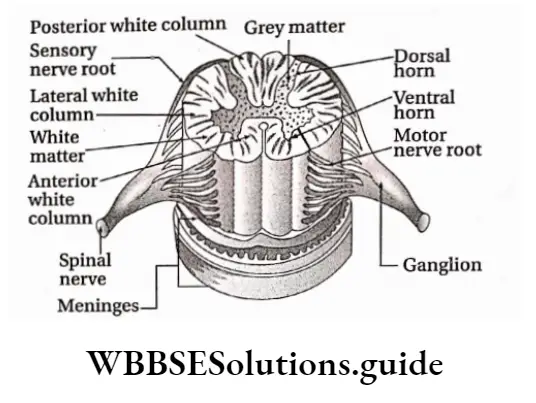
Spinal Cord
Spinal Cord Definition: The long, thin, tubular bundle of neurons and supporting cells that originate from the posterior end of the medulla oblongata of the brain enters the vertebral column, and runs through it is known as the spinal cord.
Spinal Cord Location: The human spinal cord originates from the medulla oblongata of the brain and is present within the neural canal of the vertebral column.
Spinal Cord Length and breadth: It is elongated and about 45 cm long in men and around 43 cm in women. It is enlarged in the cervical and lumbar regions.
Spinal Cord Coverings:
Just like the brain, the spinal cord also has an outer covering of meninges.
From outside to inside, layers of meninges are—dura mater, arachnoid mater, and pia mater.
Spinal Cord External structure:
- The human spinal cord continues upto the conus medullaris (tapering posterior end of the spinal cord) near the first or second lumbar vertebra, terminating in a tapering fibrous extension, known as the filum terminale.
- It is hollow, elongated, and cone-shaped.
- The posterior and anterior sides of the spinal cord bear longitudinal grooves.
- The posterior groove is known as the posterior median sulcus and the anterior groove is known as the anterior median fissure. Along these two grooves, the spinal cord divides into two symmetrical parts.
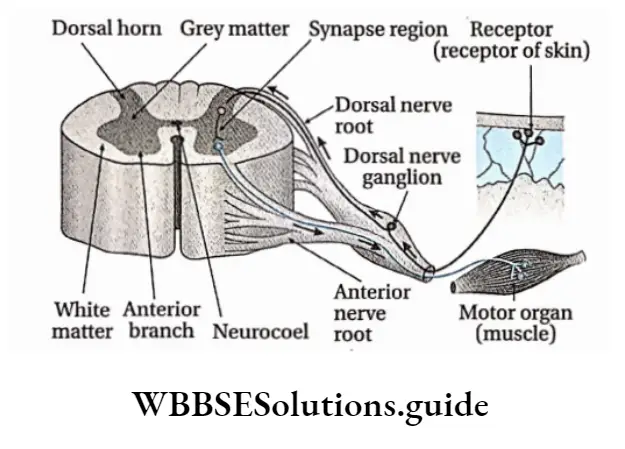
Internal structure: The transverse section of the human spinal cord shows the following structures—
Central canal: The transverse section of the spinal cord shows two symmetrical hemispheres.
Its center constitutes the central canal. The canal and its ducts are together known as neurocoel.
The central canal is lined by ciliated epithelial tissue known as ependyma. Through this canal, the CSF flows.
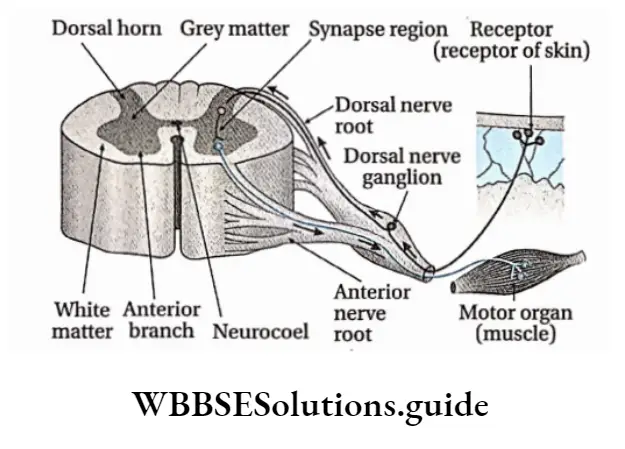
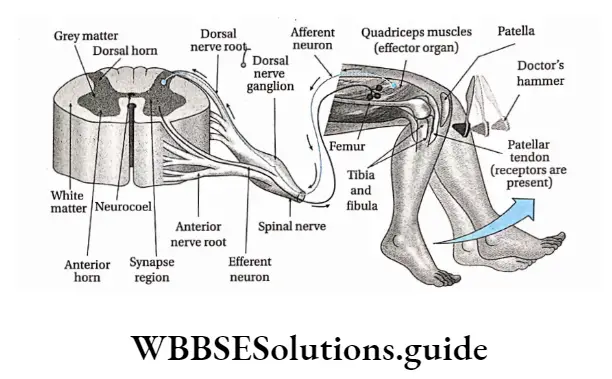
Grey matter: Grey matter is present in the center of the spinal cord like ‘H’ or like the wings of a butterfly. In each segment of the spinal cord, grey matter is distributed in three grey columns—the posterior grey column or dorsal horn,
Anterior grey column or ventral horn and Lateral grey column or lateral grey horn. Two nerve roots originate from the human spinal cord. The dorsal nerve root originates from the dorsal horn and the ventral nerve root originates from a ventral horn.
White matter: White matter envelopes grey matter and is present at the periphery of the spinal cord. In each half of the spinal cord, white matter is distributed in three columns. These are—
- Posterior white column,
- Anterior white column and
- Lateral white column
Functions:
- Spinal cord functions as the central control center for reflex actions.
- It partially controls the functions of the autonomic nervous system.
- Controls muscle tone.
- Through afferent nerve fibers, impulses from the peripheral nervous system are transmitted to the brain.
Again, motor impulses are transmitted from the brain to effector organs by efferent nerve fibers, many of which pass through the spinal cord.
This means the spinal cord maintains coordination between the peripheral system and the brain.
Peripheral Nervous System
Peripheral Nervous System Definition: The part of the nervous system that is constituted of nerves is called the peripheral nervous system.
Peripheral Nervous System Structural characteristics: The peripheral system is of two types—the somatic nervous system which is constituted of 31 pairs of spinal nerves and 12 pairs of cranial nerves and the autonomic or visceral nervous system which is constituted of sympathetic and parasympathetic nerves.
These nerves innervate various visceral organs of the body. These nerves carry sensory impulses from these organs to the CNS.
Leaf modifications in different plants with examples
Also, they carry motor impulses from the CNS to the effector organizer As a result, a response is being given by that organ.
Cranial Nerves
Cranial Nerves Definition: The nerves that originate directly from the brain are known as cranial nerves. These nerves are of three types—sensory or afferent, motor or efferent, and mixed types.
Note that, sensory nerves or afferent nerves originate from receptor organs or sense organs and meet at the brain. But, efferent nerves or motor nerves originate from the brain and meet at the effector organizer
Spinal Nerves
Spinal Nerves Definition: The nerves that emerge from the spinal cord are known as spinal nerves.
The human body consists of 31 pairs of spinal nerves. They are named as per their origin
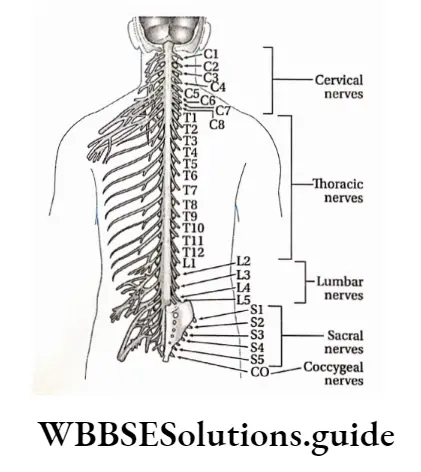
Features
- Dorsally, a branch of the spinal nerve called the dorsal root divides into six to eight nerve rootlets that enter the spinal cord.
- There is swelling, a little away from the rootlets. It is called the dorsal root ganglion.
- It contains cell bodies of afferent neurons.
- Ventrally, another six to eight rootlets leave the spinal cord and converge to form the ventral root.
- The ventral and dorsal roots merge, penetrate the dural sac, and enter the intervertebral foramen to form the spinal nerve proper.
- Spinal nerves are mixed nerves, with a two-way traffic of afferent (sensory) and efferent (motor) signals.
Function: Within the grey matter of the spinal cord, the sensory nerve enters carrying the sensory impulses.
These impulses are translated into motor impulses in the grey matter. Finally, the motor impulses leave the grey matter by traveling through the motor nerve.
Divisions of the peripheral nervous system Based upon the consciousness of our body movements PNS can be classified into the somatic nervous system (SNS) and autonomic nervous system (ANS).
The somatic nervous system controls our voluntary movement. On the other hand, the autonomic nervous system works on its own, self-controlled and independent of our voluntary efforts.
Visceral Or Autonomic Nervous System
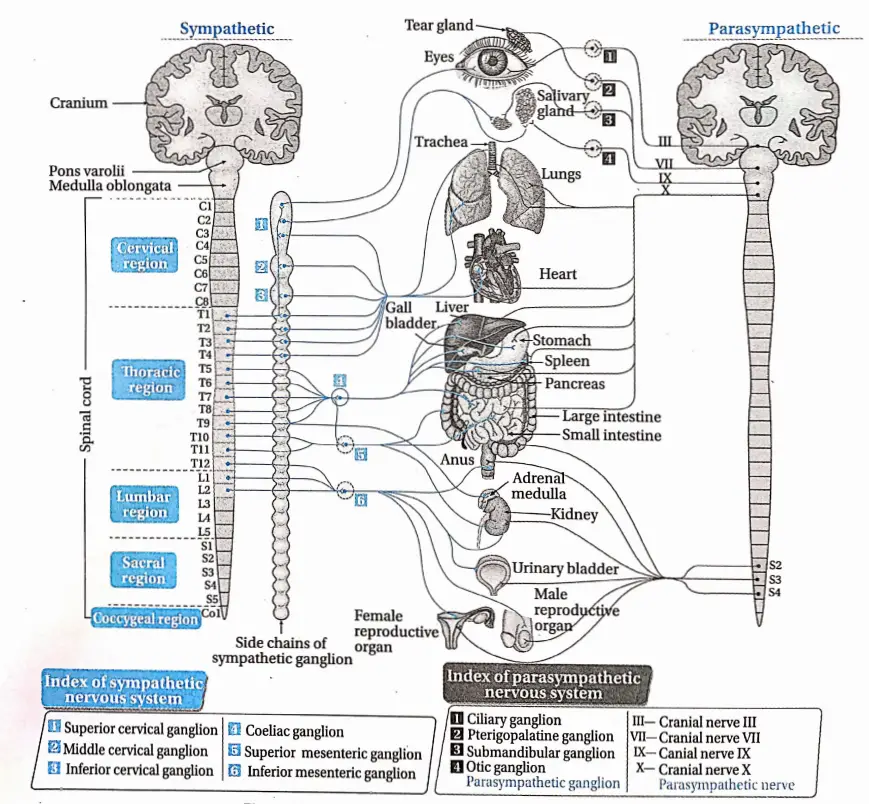
Visceral Or Autonomic Nervous System Definition: The part of the nervous system that controls bodily functions that are not controlled voluntarily such as breathing, heartbeat regulation, digestive processes, etc., is known as the autonomic nervous system.
It consists of a pair of chains of ganglions (a ganglion is a group of cell bodies of neurons outside the CNS) and nerves, found on either side of the backbone.
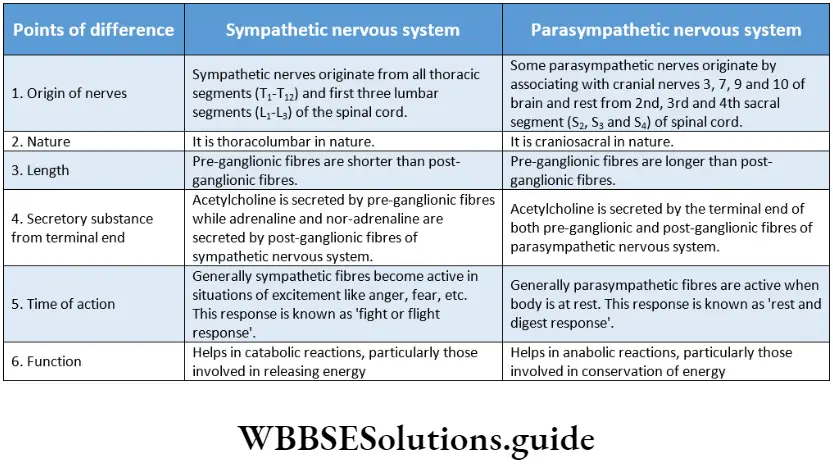
Two antagonistic and anatomically separate divisions comprise the autonomic nervous system.
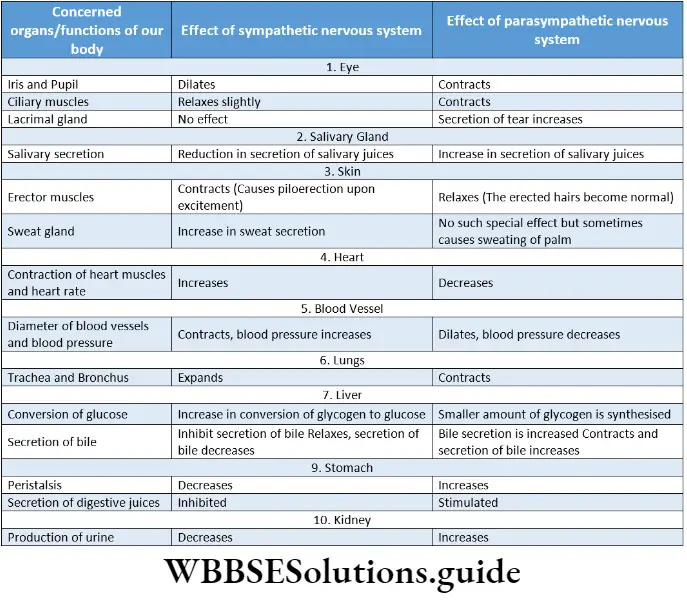
These two are called the sympathetic and parasympathetic divisions, With a few exceptions, the two subdivisions influence and act upon the organs of the body with differential effects.
Functions of the autonomic nervous system:
The general functions of ANS are as follows—
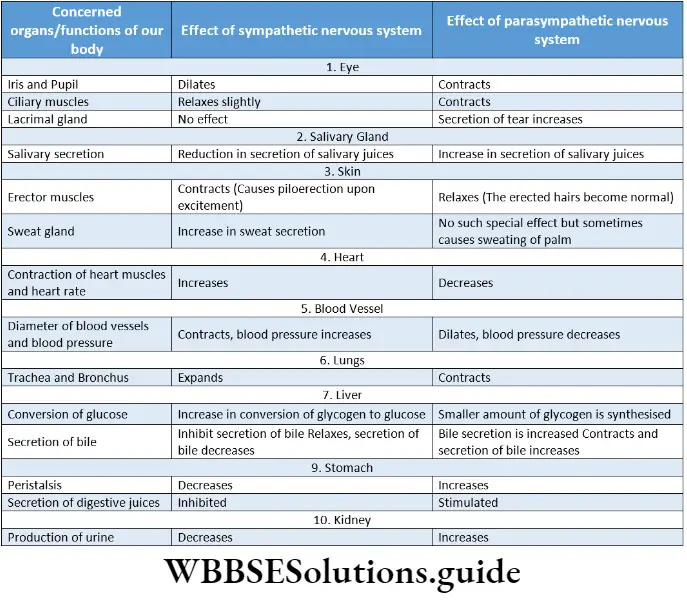
General functions: The autonomic nervous system maintains homeostasis in the body. It controls the actions of cardiac muscles and muscles of different visceral organiser
Due to the antagonistic or opposite actions of the sympathetic and parasympathetic nervous system, a balance is maintained.
Fight Or Flight Response
The ‘fight or flight’ response was first described by an American physiologist, Walter Bradford Cannon to describe the physiological reaction that occurs within animals in response to a perceived attack or threat. In this response, the animal reacts to the threat by choosing either to fight or to flee from the area.
Rest and digest the response
The ‘rest and digest response occurs when the body is at rest, especially after feeding. In this response, energy is conserved as it slows heart rate, increases intestinal and glandular activity, and relaxes sphincter muscles in the gastrointestinal tract, thereby facilitating the process of digestion.
Functions of sympathetic division:
The sympathetic nervous system controls catabolic reactions associated with the release of energy.
It functions along with the adrenal medulla. Together they constitute the sympathetic-adrenal medullary system, It increases heart rate, blood pressure, etc., dilates the pupil, reduces the secretion of saliva, secretion of sweat, expands the bronchioles of the lungs, and also expands the gall bladder, urinary bladder, etc.
Functions of the parasympathetic nervous system:
The parasympathetic nervous system controls the anabolic reactions of the body. It enables digestion, absorption, storage of food, etc., and stores energy in the body.
The parasympathetic nervous system controls normal regular physiological activities of the body. It helps to secrete various digestive juices and thus helps in digestion. It also helps to absorb the digested food.
It increases the secretion of tears, reduces blood pressure, and contracts the urinary bladder.
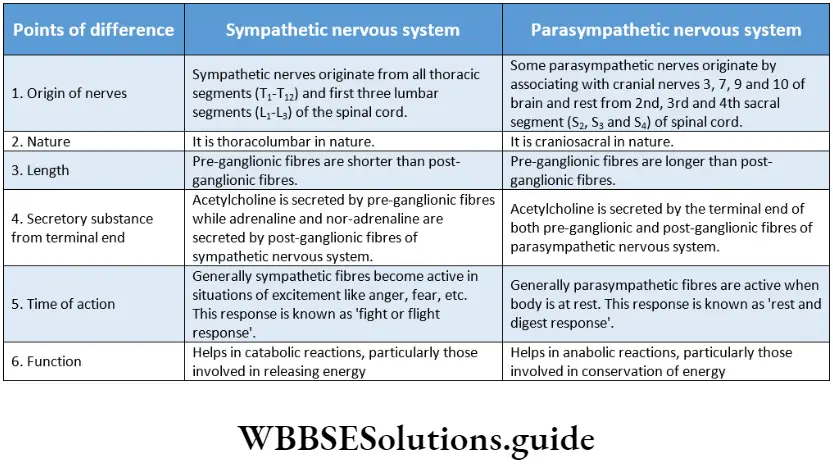
Sympathetic Nervous System
The division that accelerates various activities of the body like heartbeat, breathing, etc., is called the sympathetic nervous system. The response given by this system is a ‘fight or flight’ response.
Sympathetic nerves originate from the thorax and lumbar region. During anger, fear, etc., the activity of the sympathetic nervous system is increased.
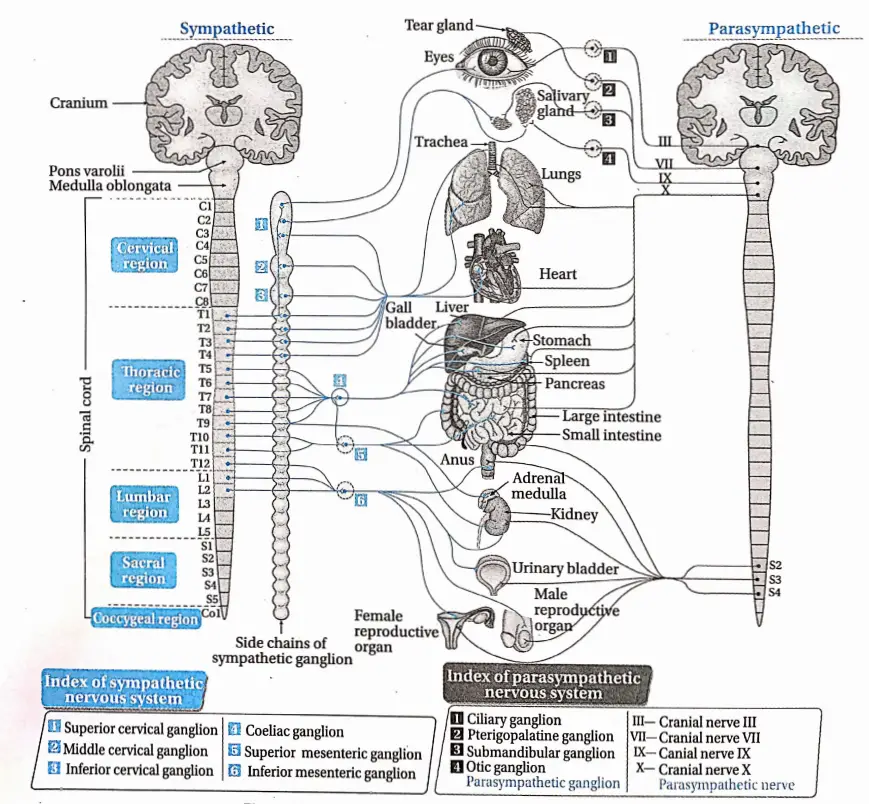
Origin: Sympathetic nerves originate from the lateral horn of grey matter of the first thoracic vertebra to the third lumbar vertebra.
Components: The four components of the sympathetic nervous system are—
Chain of lateral ganglia: This chain is composed of 21 ganglia which extend from the cervical to the sacrum region.
Pre-ganglionic fibers: These fibers are axons of neurons that are located in the spinal cord.
Collateral ganglia: Coeliac ganglion, superior mesenteric ganglion, and inferior mesenteric ganglion are the three collateral ganglia of the sympathetic nervous system which are located in the abdominal cavity.
Parasympathetic Nervous System
The part of the autonomic nervous system that decreases or slows down various activities of the body like heartbeat, respiratory process, etc., is called the parasympathetic nervous system.
The parasympathetic nervous system is anatomically of craniosacral type. The response given by this type of nervous system is Vest and digest’ response.
The nerves of the parasympathetic nervous system originate from the cranium and sacral vertebral segments of the spinal cord and are called the craniosacral nervous system.
Generally, the action of parasympathetic nerves increases when the body is at rest.
Parasympathetic Nervous System Origin: Some of the parasympathetic nerves originate from the brain by fusing with cranial nerves 3, 7, 9, and 10.
The rest of the parasympathetic nerves originate from the sacral vertebra 2nd, 3rd, and 4th (S2, S3, and S4) of the spinal cord.
Components: The three components of the parasympathetic nervous system are—
Pre-ganglionic fiber: These are the axons of neurons that are located in the midbrain, brain stem, and sacral segment of the spinal cord.
Parasympathetic ganglia: These ganglia are located very close to the peripheral tissue.
They do not form a chain of ganglia. The pre-ganglionic fibers synapse with the neurons of parasympathetic fibers.
Post-ganglionic fiber: These are the axons of neurons that are located in the sympathetic fiber.
Nerve Impulse
A nerve impulse refers to an electrical or chemical signal that is transmitted along a nerve fiber.
The neurons of the nervous system are not connected directly i.e., they lack any cytoplasmic connections between them.
So nerve impulses are transmitted from one neuron to another by synapse.
So before going into the details about the process of transmission, we have to know about synapses which are as follows.
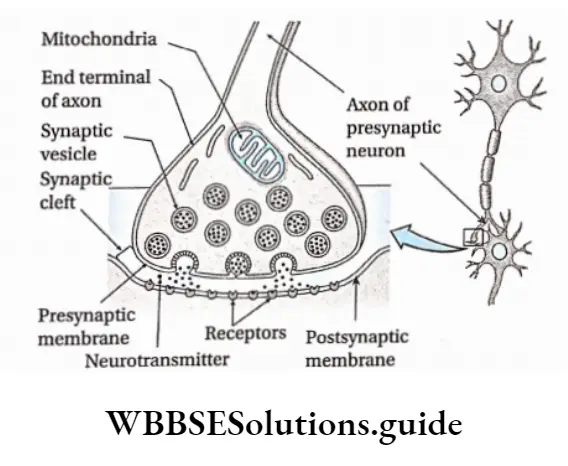
Synapse
The word ‘synapse’ came from ‘synaptein’, which Sir Charles Scott Sherrington et a!., had coined from the Greek word ‘syn-‘ (‘together’) and ‘haptein’ (‘to clasp’).
Synapse Definition: The microscopic gap present between the terminal end of the axon of one neuron and the dendron or axon or cell body of another neuron, through which nerve impulses are transmitted by neurotransmitters or electrical ions from the neuron to the post neuron is called a synapse.
Synapse Structure:
- In a neuron, an impulse travels along the length of the axon until it reaches the far end, called the axon terminal.
- The axon terminal branches profusely and gives a brush-like appearance hence called end brush.
- The terminal portion of each of these branches is swollen. It is called the synaptic knob or terminal knob.
- The axon terminal ends very close to the dendron or cell body or axon of another neuron, with which it forms the synapse.
- Here, the first neuron is called a presynaptic neuron while the second one is called a postsynaptic neuron.
- The nerve impulse is transmitted from the presynaptic neuron to the postsynaptic neuron.
- The membrane of the presynaptic neuron along the synapse is called the presynaptic membrane.
- The membrane of the postsynaptic neuron along the synapse is called the postsynaptic membrane. There is a gap between pre- and postsynaptic neurons. It is called the synaptic cleft.
- In the cytoplasm of the presynaptic axon terminal, there are small membrane-bound vesicles called synaptic vesicles which contain neurotransmitters.
- These substances act as chemical messengers and help to carry the neural signal from one neuron to another.
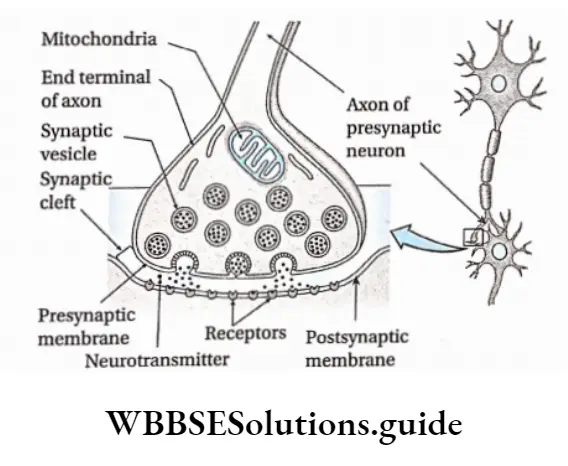
Types of synapses: On the basis of the medium of transmission of impulses synapses can be classified into three types, such as—
- Chemical synapse: Impulses are transmitted by neurotransmitters.
- Electrical synapse: impulses are transmitted by ions.
- Conjoint synapse: Impulses are transmitted by both chemical as well as electrical signals.
On the basis of structure, synapses can be classified into four types, such as—
Axodendritic synapse: The synapse between the axon of the presynaptic neuron and the dendrite of the postsynaptic neuron.
Axosomatic synapse: The synapse between the axon of the presynaptic neuron and the cell body or soma of postsynaptic neurons.
Axoaxonic synapse: The synapse between the axons of both, pre and postsynaptic neurons.
Dendrodendritic synapse: The synapse between the dendrites of both, pre and postsynaptic neurons.
On the basis of participating nerve cells, synapses can be classified into 3 types—
One-on-one: In this case, one neuron forms a synapse with another neuron.
Many with one: In this case, the terminal end of a number of neurons forms a synapse with one neuron.
One with many: In this case, the terminal end of one neuron forms a synapse with many neurons.
Functions: Synapses have four main functions. They are as follows—
They transmit information between neurons or neurons and their target cells.
They filter out low-frequency impulses.
They act as valves to ensure that impulses pass across them in one direction only.
They also act as junctions allowing impulses to be divided up along many neurons or merge into one.
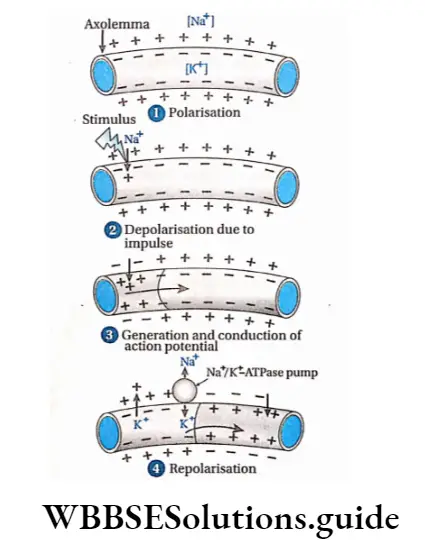
Generation Of Nerve Impulse
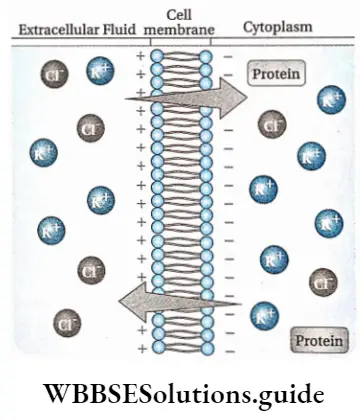
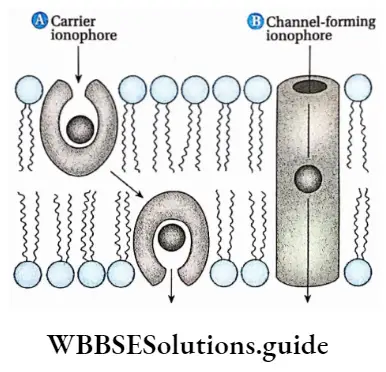
The generation of nerve impulses in nerve fibers depends on the distribution of Na+ and K+ in and out of the axolemma. Again, the distribution of Na+ and K+ is controlled by protein channels.
(such as Na+ and K+ channels) and carrier proteins like Na+/K+ -ATPase pump, in the axolemma. The different stages of the generation of nerve impulses are described below.
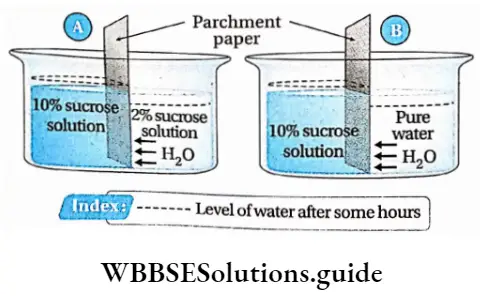
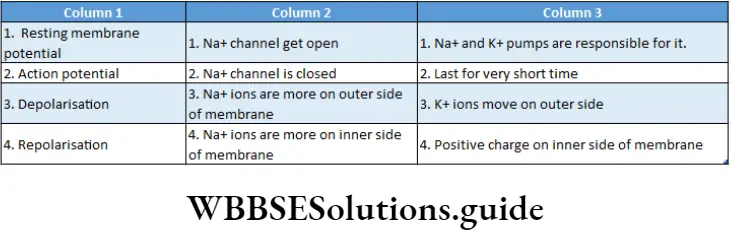
Resting Potential: It is the potential difference across the membrane of a resting neuron i.e., when nerve impulses are not transmitted.
At this stage, the axonal membrane is nearly impermeable to Na+ while comparatively more permeable to K+.
The ‘membrane is also impermeable to negatively charged proteins present in the axoplasm. As a result, inside the axoplasm, there is a high concentration of K+ and negatively charged proteins and a low concentration of Na+.
During resting conditions, this potential difference across the axonal membrane is called resting membrane potential. This state of the resting membrane is called the polarised state.
The average value of resting membrane potential is -70mV.
Action Potential: When a nerve receives a stimulus, a sequence of events occurs.
Due to the conduction of impulse in a region, Na+ channels of that region open.
This causes an influx of Na+ inside the axoplasm. This creates an increase in positive charge in the axoplasm.
Thus the polarisation across the membrane, as found under resting conditions is now reversed. The reversal of polarity is called depolarization. The potential difference across.
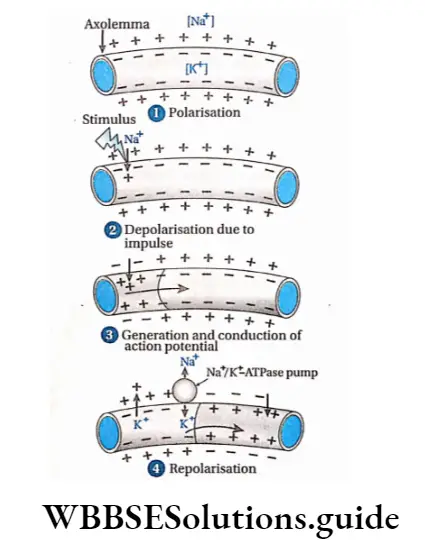
The membrane under this condition, is called action potential. Its value is +35mV.
After depolarisation, Na+ channels are closed. The wave of this reversed polarity of depolarisation (action potential) moving down an axon is called a nerve impulse or spike.
Repolarisation: When the action potential of the axon becomes +35 mV, the K+ channel of the axolemma opens. Due to this reason, K+ from the intracellular matrix moves out to extracellular fluid. As a result, electric potential is reduced.
Gradually, the positive charge in the extracellular fluid increases compared to td axoplasm.
After some time, the concentration of K+ increases in extracellular fluid so much that the K+ channel closes. At this time, the Na+/ K+-ATPase pump opens.
Through this pump, three Na+ move out from the axolemma, and two K+ move inside the axolemma.
In this way, after some time, the concentration of Na+ and K+ becomes the same as before (as in resting condition) on either side of the axolemma. Thus, nerve fibers again attain resting potential.
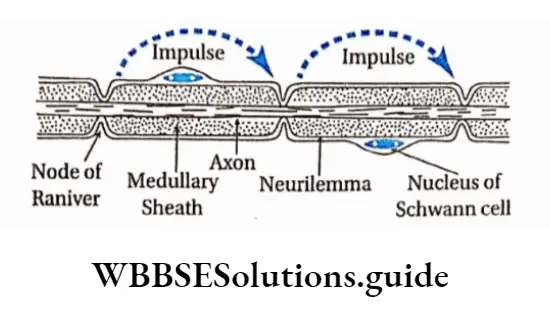
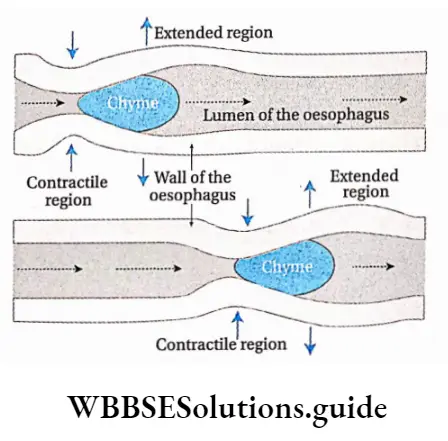
Conduction Of Nerve Impulse
The process of conduction of nerve impulses through medullated, and non-medullated nerve fibers and synapses follows various methods as described below.
Conduction of nerve Impuluses in Non-medullated nerve fibres: Nerve impulse or action potential is transmitted in small steps. In each step, repolarisation and depolarisation take place. This is known as continuous conduction.
Conduction of nerve impulses in medullated nerve fibers: Myelin sheath contains fat. Since fat is a poor conductor of heat and electricity, it cannot transmit impulses.
Only nodes of Ranvier allow transmission of impulses and ion exchange occurs at these points. So, depolarisation of nodes of Ranvier occurs.
The depolarised node of Ranvier triggers an increase in the permeability of ion channels leading to depolarisation in the adjacent node of Ranvier. Therefore, nerve impulses are transmitted by jumping from one node to the next.
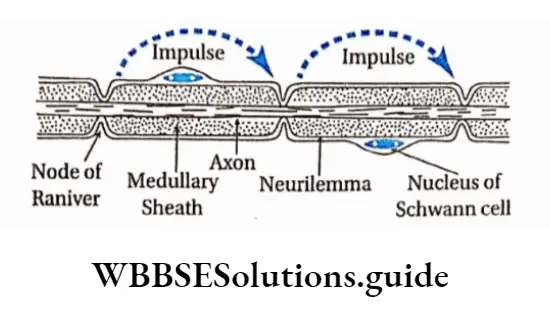
So, it is faster in the medullated nerve fibers than the non-medullated nerve fibers.
This type of conduction is called saltatory conduction because it has been derived from the Latin word saltare which means ‘leaping’.
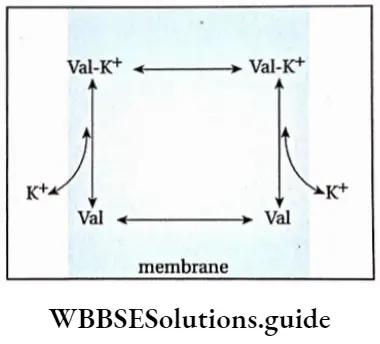
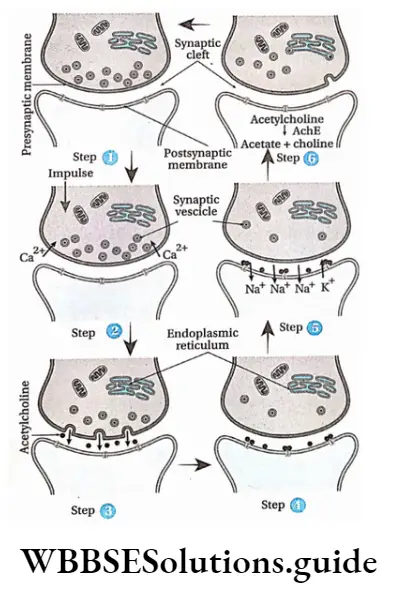
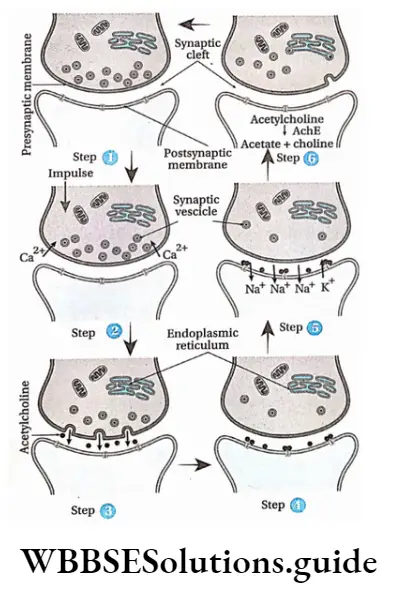
Synaptic transmission: Synaptic transmission is the process whereby electrical impulses pass through a synapse with the release of neurotransmitters.
Transmission of nerve impulses in the synapse region is a chemical process.
The sequence of events that lead to postsynaptic changes is as follows—
- As the action potential reaches the axon terminal of a presynaptic neuron, depolarisation occurs which causes voltage-gated Ca2+ channels to open. This leads to an influx of Ca2+ into the synaptic knob from the cisternal.
- Ca2+ influx in the axoplasm of the synaptic knob continues. This causes an increase in concentration of Ca2+ and eventually induces vesicles filled with neurotransmitters, to migrate towards the presynaptic membrane. There the vesicles fuse with the presynaptic membrane.
- The presynaptic membrane and vesicles now form a continuous membrane, so that the neurotransmitter i.e., acetylcholine, is released into the synaptic cleft also by exocytosis. There may be other types of neurotransmitters such as adrenalin, dopamine, etc., but the following discussion is given with respect to acetylcholine.
- Acetylcholine diffuses through the synaptic cleft and binds with receptor site on the postsynaptic membrane.
- As a result, acetylcholine-dependent sodium ion channels open, and movement of sodium ions takes place through the postsynaptic membrane. This creates a change in the membrane potential of the post-synaptic membrane.
- The postsynaptic membrane and synaptic cleft contain the enzyme acetylcholinesterase. This enzyme hydrolyses acetylcholine into acetate and choline. This causes repolarisation of the postsynaptic membrane.
- The entire cycle repeats again.
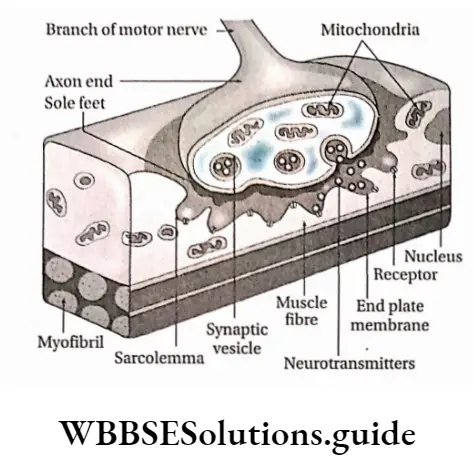
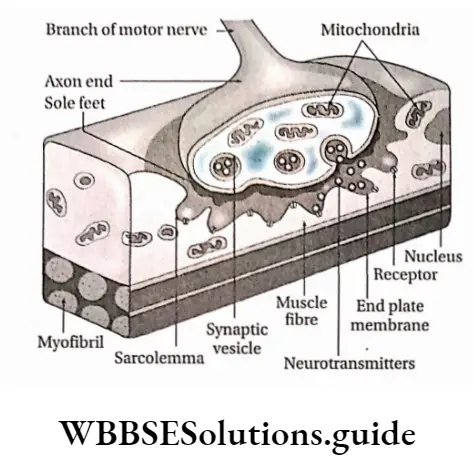
Neuromuscular transmission: The junction between a motor neuron and a muscle fiber by which the nerve can communicate with the muscle fiber is called the neuromuscular junction.
Through these junctions, neurotransmitters are transmitted from the neuron to the muscle. This type of transmission is known as neuromuscular transmission.
In this case, the terminal end of the axon extends and appears like a plate, which is located near the sarcolemma.
At the neuromuscular junction, the plate-like structure formed by the axon terminal is known as the motor end plate.
The extended part of the terminal end motor neuron is known as sole feet or end feet. The axoplasm of this part contains more vesicles.
These vesicles contain neurotransmitters like acetylcholine. This portion also contains endoplasmic reticulum, mitochondria, etc. Sarcolemma of muscle fibers are thick and contain grooves.
The following events occur at the neuromuscular junction—
The axon of the motor neuron carrying a vesicle containing acetylcholine reaches the motor end plate with the help of Ca2+ ions.
Acetylcholine from these vesicles is released between the membrane of the sole feet and muscle fibers. This causes depolarization of the end plate and creates action potential.
As a result, impulses from the end plate enter muscle fibers and cause contraction of muscle fibers.
Neurotransmitters
The organochemical substances that transmit nerve impulses from the presynaptic region to the postsynaptic region at the synapse are known as neurotransmitters.
They are of two types—excitatory and inhibitory.
Excitatory: These are capable of depolarising the postsynaptic membrane and transmitting nerve impulses. Examples—are acetylcholine, and noradrenaline.
Inhibitory: These prevent the transmission of nerve impulses in the synaptic region. Example—GABA (y-amino butyric acid), is Screted from the axon end of some neurons in CNS.
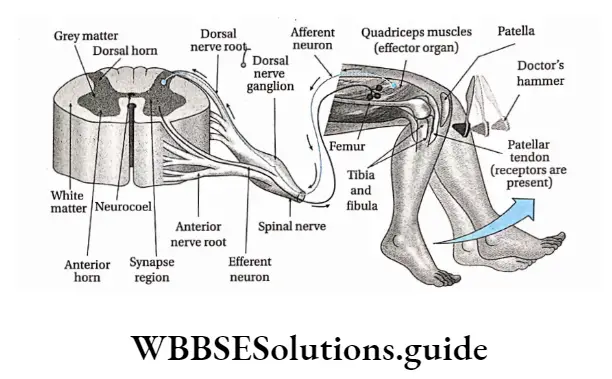
Reflex Action And Reflex Arc
Some neurons are organized to enable the human body to react rapidly at times of danger, even before consciously being aware of the threat. Under such conditions, impulses from sense organs are not transmitted to the brain but to the grey matter of the spinal cord.
Venation in leaves and its types with diagram
There it is analyzed fast and action impulses are transmitted to the effector organiser These sudden, unlearned, involuntary responses to certain stimuli are called reflex action. The neural path along which reflex action takes place is known as the reflex arc.
Reflex Action
Reflex Action Definition: A spontaneous, automatic, involuntary response to a stimulus that occurs without any conscious effort or thought and requires the involvement of CNS, is known as a reflex action.
Examples:
- Drawing back of the hand when pricked with a needle.
- Sudden closing of eyes when flashed with a high-intensity light.
- Secretion of saliva on seeing or smelling food.
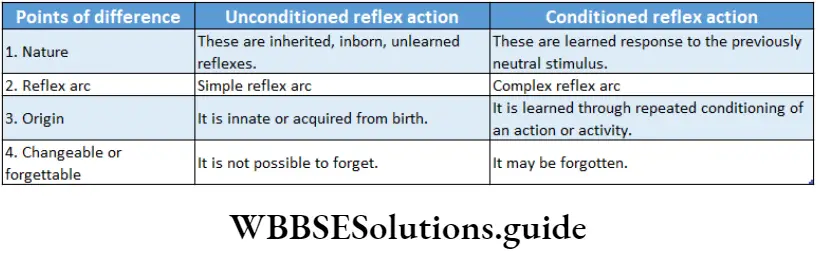
Types Of Reflex Action
The types of reflex actions are described below.
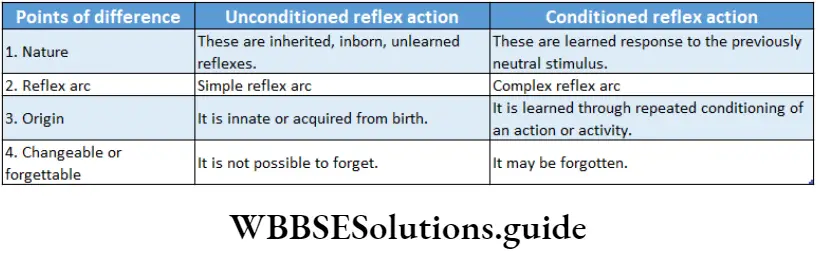
Unconditioned or inborn reflexes: The reflexes which are automatic, instinctive, unlearned reaction and can be evoked even immediately after birth, is called inborn or unconditioned reflex action.
These reflex actions do not need previous exposure to the stimulus.
So these are inborn and inherited reflex actions. The reflex arc of this reflex action is stable (that is, it follows a simple reflex arc. These types of reflex actions cannot be changed or forgotten easily.
Types: On the basis of the type of organs involved with inborn reflex actions, these are divided into three types. These are as follows—
Superficial reflex action: The types of reflex action in which stimuli are exerted on superficial structures, mainly in skin or mucous membranes, are known as superficial reflex action.
Example:
- Sudden exposure to bright light causes us to close eyes due to pupillary reflex,
- Sudden exposure of the hand to fire causes it to draw it back.
Simple And Complex Reflex Arc
If a sensory neuron connects directly to a motor neuron in the special cord then it is known as a simple reflex arc.
However, in some reflex arcs, the sensory neuron connects to the motor neuron through association neurons, and such reflex arcs are known as complex reflex arcs.
Effect Of Cerebellum On Reflex Action
The role of the cerebellum is to finely tune the reflex arc. This role of the cerebellum is gradually archived and adjusted through the process of learning.
Based on past experiences, the cerebellum rectifies any motor error in the reflex arc and uses this prediction to adjust motor output, thereby helping in the process of reflex action.
Visceral reflex action: The type of reflex action in which stimuli are exerted on the visceral organs of the body is called visceral reflex action.
Example:
Digestive reflexes such as secretion of digestive juices after engulfing food and movement of the bowel after digestion.
Cardiovascular reflexes such as regulation of heartbeat, blood pressure, etc.
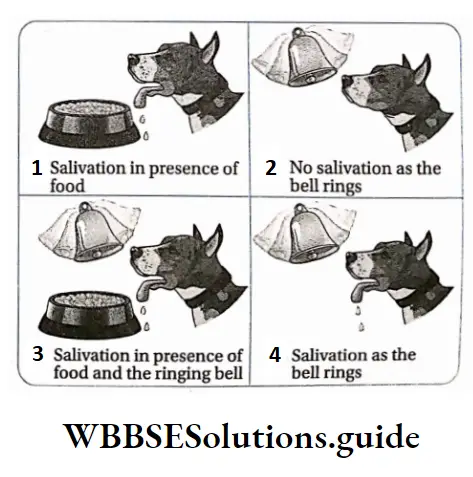
Acquired or conditioned reflex action: The reflex actions that are acquired by training after birth and are subjected to changes are known as acquired or conditioned reflex actions.
These actions are acquired by humans and other vertebrates after birth. These actions depend on repeated conditioning. These actions are subjected to be forgotten or changed as per need.
Example:
- Walking, writing by a child.
- Riding bicycle.
- Reciting poem.
- Actions shown by animals in circuses, etc.
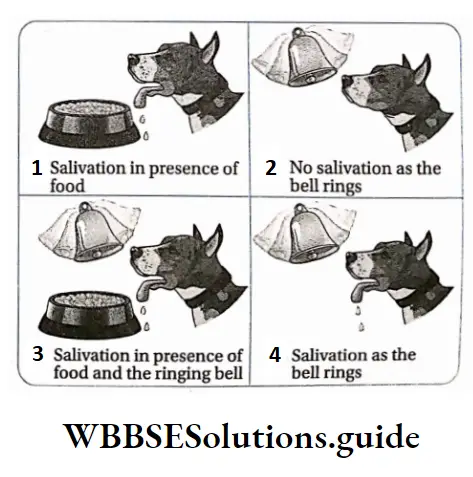
Pavlov’s experiment
The famous Russian scientist Ivan Petrovich Pavlov is known as the father of conditional reflex action.
He has performed an experiment to prove how an unconditioned reflex action can generate a conditioned reflex action. His experiment was as follows
Deep reflex action: The type of reflex action in which stimuli are exerted on some underlying structures, mainly in muscles and tendons, is known as deep reflex action.
Example:
Knee jerk or patellar tendon reflex—When the knee is hit by a doctor’s hammer, the thigh and lower portion of the leg jerk,
Biceps jerk reflex—Suddenly hitting the biceps causes stretching in the tendon due to which elbow folds.
An unconditioned stimulus (food—meat) was presented to a hungry dog every day. It caused salivation (an unconditioned response).
At the same time, a conditioned stimulus (ringing a bell) was given. The dog learned to associate the conditioned stimulus (bell) with the unconditioned stimulus (food).
Eventually, after some days, it was observed that ringing of the bell alone caused salivation. This is because the dog adapted to the stimulus of a ringing bell that brought food.
Reflex arc Definition: The path through which reflex action takes place and extends between the sensory organ to the effector organ through the grey matter of the spinal cord is called reflex arc.
Different components of a reflex arc and their functional roles
The reflex arc is constituted of five parts that are described below.
Receptor: To accomplish a reflex action, the reflex arc must be directly linked with a receptor organ. Reflex action occurs when sense organs or receptors are excited by a stimulus.
Sensory or afferent neuron: These neurons of a reflex arc remain connected with the receptor. They carry impulses from the receptor to the grey matter of the spinal cord.
Grey matter of spinal cord: Grey matter of the spinal cord acts as the controller or center of reflex action. In the grey matter of the spinal cord, sensory impulses are analyzed and interpreted.
Effector organ: Effector organs are capable of responding to a stimulus to perform a particular action. Generally, muscles, glands, etc., participate as effector organs.
Sense Organs
Sense Organs Definition: The organs that are specialized to acquire and process sensory stimuli from different sources, both external and internal are called sense organizer
Sense Organs Types: Humans and other advanced vertebrates have different types of sense organizers The human body consists of five main types of sense organizer
These are—
- One Pair Of Eyes
- One Pair Of Ears
- Nose
- Tounge
- Skin
Sensory Receptors
Sensory Receptors Definition: The sensory nerve endings, a cell or group of cells, that respond to various kinds of stimulation are called receptors.
They are transducers that convert various forms of energy in the environment (internal or external) into action potentials in the afferent neurons. The awareness that results within the body is called sensation.
The sense organs—the eyes, ears, skin, mouth, and nose—have receptors that detect sensations. The sensory neurons present within them transmit the information to the central nervous system where it is interpreted as sight, sound, touch, taste, or smell.
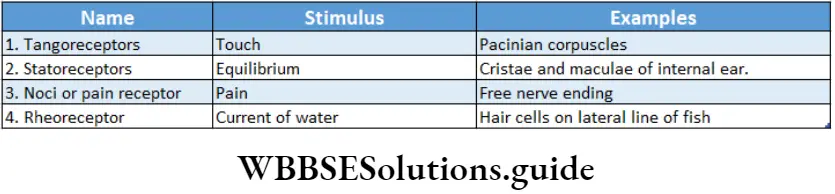
Types of receptors: Receptors are classified into different types, as depicted in the chart given below.
On the basis of the location of the receptors, it can be classified into three types—
Exteroceptors: These receptors are located near the surface of the body. They can sense changes in the surrounding environment. Generally, they include receptors for touch, heat, cold, etc.
Interoceptors: These receptors are located within the body. They are stimulated by the internal stimuli which are generated inside the body.
There are several types, such as—chemoreceptors, stretch receptors, baroreceptors, etc.
Proprioceptors: The receptors which can detect the position and posture of the body.
They are located in skeletal muscle, bones, tendons, ligaments, etc. On the basis of the type of the received stimuli, receptors can be classified into five types, etc
Mechanoreceptors: These are receptors that are stimulated by mechanical forces, such as touch, pain, equilibrium, etc., received on muscles, tendons, ligaments, and joints. They comprise both exteroceptors and interoceptors.
Several types of mechanoreceptors are discussed in the following table.
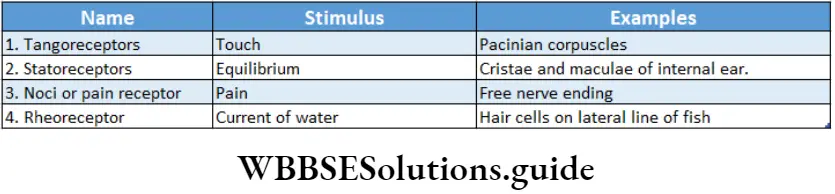
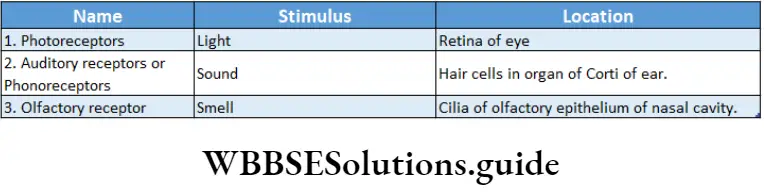
Telereceptors: Receptors sensing light and sound, which provide information about the distant environment, are called telereceptors.
Telereceptors, on the basis of their location, have been divided into three types which have been discussed below.
Chemoreceptors: These are receptors that are stimulated by chemical changes or by chemicals that are either inhaled or tasted (gustatory receptors).
They also modify hydrogen ion and carbon dioxide concentrations in blood. For example, chemoreceptors of the carotid artery can sense changes in blood partial pressure of 02 and C02 in the blood
Thermoreceptors: These are receptors that are sensitized by heat. For example, Ruffini’s end organs, are the end organ of Mazzoni.
Galvanoreceptors: These are receptors that are sensitized by gravity. For example, the organs of some fish have this type of receptor.
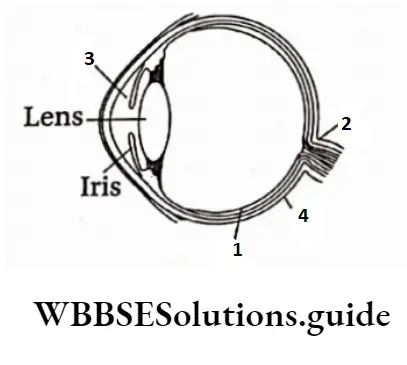
Human Eye
Our eyes are sense organs for vision. They also help in the perception of color.
Human beings have two simple eyes, present ventrally to the cranium and above both sides of the nose.
They are placed within the eye orbits. We have binocular vision (which involves two eyes to view an object). In the case of frogs, fish, etc., monocular vision (which involves one eye to view an object) is observed.
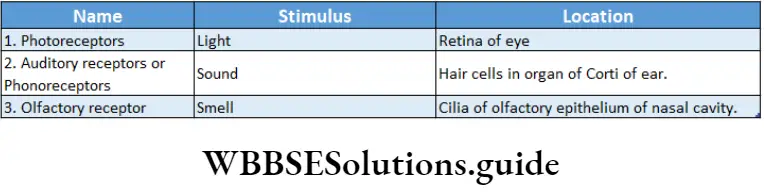
Eyeball
On the ventral portion of the brain box and above both sides of the nose, there are two cavities or orbits called the eye cavities within which eyeballs are located. These are supported by muscular tissue.
Each eyeball is almost spherical and has a diameter of 2.5 cm. The eyeball remains in position within the cavity with the help of six muscles. Eyeball actually is a fluid-filled sac-like structure.
It is composed of three parts—
- Coats,
- Eye chambers and
- Refractory media
- Coats
The human eyeball is covered with three layers or coats which are—
- Fibrous coat,
- Pigmented coat and
- Neural coat.
Fibrous coat: The outermost layer of the wall of the eyeball is made up of fibrous connective tissue. This layer can be divided into two—
Sclera: This is the outer covering layer of the eyeball. The sclera is present in the posterior portion, comprising about five-sixth part of the external layer.
The sclera is a comparatively tough, translucent, and thick layer that is composed of white collagenous connective tissue. The posterior region of the eyeball from where the optic nerve emerges lacks sclera.
Cornea: It is the bulged, transparent anterior region of the eyeball. It covers the l/6th part of the fibrous coat of the eyeball. On the outer surface of the cornea, there is a thin and clear layer called the conjunctiva.
Functions of fibrous coat:
The sclera provides shape to the eyeball and forms a protective rigid layer for the eyeball.
Being transparent, the cornea acts as a refractive medium and permits light to pass through easily and fall on the lens. It acts as a convex lens to converge the diverging rays.
Pigmented coat or vascular coat: The middle layer of the human eyeball contains melanin pigment in its cells.
So, this layer appears brown. This layer is known as the pigmented layer. It is calculated and so, known as vascular coat. The different parts of this layer are discussed below.
Choroid: The melanin-containing brownish part beneath the sclera, in human eyeball is known as choroid.
Ciliary body and suspensory ligament: The thin layer that is present in the terminal region of the choroid, at the junction of the sclera and cornea of the human eyeball is known as the ciliary body. The thin fibers projecting from the ciliary body are known as suspensory ligaments.
Iris: The pigmented part present in front of the ciliary body, suspensory ligament, and lens of the human eyeball is called the iris. It controls constriction and dilation of the pupil.
At the center of the iris, a spherical opening is present, known as the pupil.
Iris contains two types of muscles—
Circular Muscles And Radial Muscles.
Functions of pigmented or vascular coat:
Due to its deep brown color, the choroid absorbs excess light and prevents its repeated reflection. Thus, it helps to form a clear image.
Suspensory ligaments hold the lens in its proper position.
While seeing objects nearer or farther, we cannot move the lens forward or backward, but with the help of ciliary muscles, the curvature of the lens can be changed. As a result, the focus of the lens can be changed as required. This phenomenon is known as accommodation.
The pupil dilates and constricts due to the action of circular muscles and radial muscles of the iris. In this way, the iris modifies the diameter of the pupil and controls the incident rays on the lens. The color of the iris is considered the color of the eye.
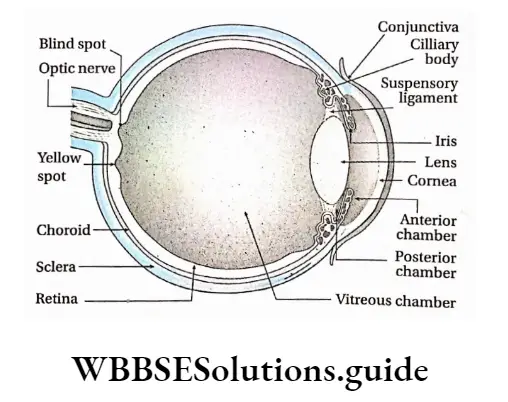
Neural coat or retina: The most internal layer of the human eye is the posterior part of the lens and the inner portion of the choroid where the optic nerve is found. This layer, made up of nervous tissue and connective tissue is known as the neural coat or retina
Structural features of the retina:
- Retina, present posterior to the lens, is extended dorsally to ciliary bodies.
- The different cells of the retina are arranged in 10 layers.
- The most external layer among the 10 layers is pigmented and remains associated with the choroid.
- There are two types of pigmented cells in this layered cells and cone cells. These cells are also described later.
The different neuronal cell layers of the retina bear four types of cells—bipolar cells, ganglion cells, horizontal cells, and amacrine cells.
All the nerve cells in the most internal retinal layer form the optic nerve.
The retina also contains one type of glial cell called Muller cell that helps in maintaining its structural integrity.
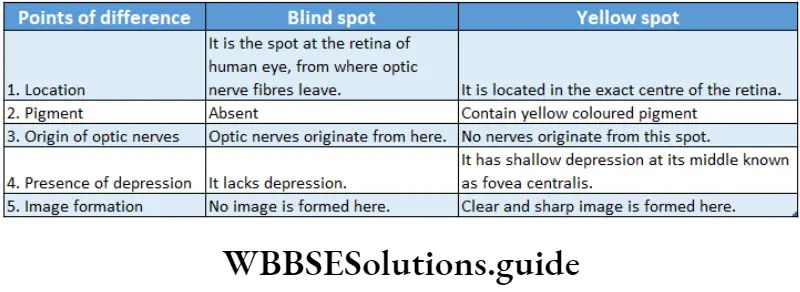
A depressed region is observed at the center of the retina. It is yellowish and so, known as yellow spot or macula lutea.
The clearest and brightest image is formed in this region. Its central region is depressed known as fovea centralis. It is the most photosensitive region of the retina.
The junction between the origin of the optic nerve and the posterior end of the retina lacks any photosensitive cells (rod and cone cells).
As a result, the image does not form in that region. This part of the retina is known as the blind spot or optic disc.
Different cellular layers of the retina: The retina consists of the following 10 layers—
Pigment epithelium: This outermost layer of the retina consists of pigmented cells. This is a non-neural layer that absorbs excess light which has passed through the other retinal layers and is immediately next to the choroid.
Photoreceptor layer: This layer includes the outer external segments of the photoreceptor cells, rods, and cones.
External limiting membrane: Although this appears to be a membrane, actually it is not. It is formed by intercellular junctions—the zonula adherent—binding the apical aspect of the Muller cells.
External nuclear layer: This consists of the cell bodies of the rods and cones.
External plexiform layer: This is a synaptic area that contains the terminals of the rods and cones.
Inner nuclear layer: This consists of the soma of the retinal interneurons (horizontal, bipolar, and amacrine cells). It integrates and modulates the activity of photoreceptors.
Inner plexiform layer: This is a synaptic area containing the terminals of the bipolar, amacrine, and ganglion cells.
Ganglion cell layer: This consists of the soma of the ganglion cells (multipolar neurons).
Optic nerve fiber layer: This layer is composed of the axons of the ganglion cells that gather to form a thick bundle, the optic nerve.
Internal (inner) limiting membrane: This membrane is composed of a basal lamina interposed between the vitreous body and the Muller cells.
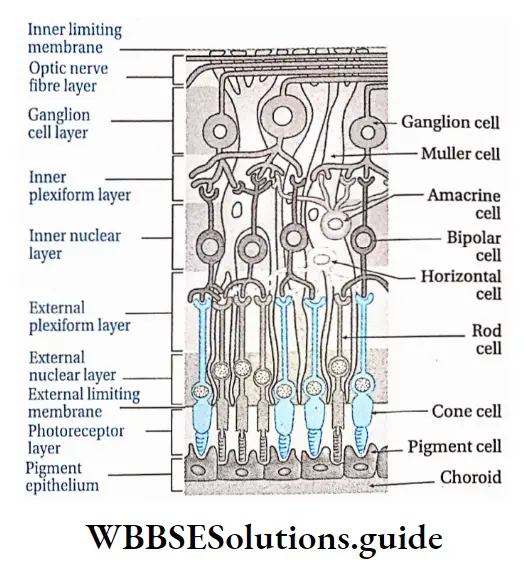
Photoreceptor cells of the retina: The human retina contains two types of photoreceptor cells—rod cells and cone cells. These are discussed below.
Rod cells: These cells are rod-shaped. They contain the pigment rhodopsin. Vitamin A is required for the synthesis of rhodopsin. The human eye contains 115-120 million rod cells.
Functions:
Rod cells help to see objects in dim light at night, which means they can absorb low-intensity light,
Rod cells generally form the black and white vision.
Cone cells: These cells are cone-shaped. They contain the pigment iodopsin. The human eye contains 6.0-6.5 million cone cells.
Functions:
Cone cells are capable of absorbing high-intensity light, so they help us to see objects in bright light,
They help in the perception of color and thus are responsible for color vision. The inactivity of cone cells leads to color blindness.
Functions of retina
The retina of the human eyeball acts as the photoreceptor organ. Rod cells of the retina help to see objects in dim light. On the other hand, cone cells help to see objects in bright light.
Light from different sources reflects on the lens and creates an image on the retina. This reflection is transmitted to the cerebrum by optic nerves. There it is translated and a sensation of vision is created.
The yellow spot of the retina, especially the fovea centralis, forms a clearer image of the object.
Rod cells of the retina cause black-and-white vision and cone cells causes colored vision.
Eye chambers
The human eyeball contains three chambers which are as follows—
- Anterior chamber: The chamber between the iris and cornea of the human eyeball is known as the anterior chamber. This chamber is filled with fluid aqueous humor.
- Posterior chamber: The thin chamber between the lens and iris of the eyeball is known as a posterior chamber. This chamber is also filled with aqueous humor.
- Vitreous chamber: The large chamber at the posterior part of the lens, between the lens and the retina is known as a vitreous chamber. This chamber is filled with fluid vitreous humor.
Refractory Media
All those parts of the eyes that convert parallel or divergent light rays into convergent light rays are known as refractory media. The refractory media of human eyes are—lens, aqueous humor, vitreous humor, and cornea.
Lens: It remains suspended from ciliary bodies by the suspensory ligament in the human eyeball. It is the main refractory medium of human eyes.
The lens is elastic in nature and bi-convex in shape. It is composed of transitional columnar epithelial tissue. It is as clear as crystal. It contains the protein crystallin. It is surrounded by a capsule.
Functions:
It is the main refractory medium of human eyes.
It helps to focus on objects based on distance. While seeing a nearby object, ciliary muscles contract and the lens becomes thick. While seeing distant objects, ciliary muscles relax, thus reducing the thickness of the lens.
Aqueous humor and vitreous humor: The clear fluid substance present in the anterior and posterior chambers of the human eye is known as aqueous humor.
On the other hand, the fluid substance present in the vitreous chamber of the human eye is known as vitreous humor.
Both aqueous and vitreous humor is made of salt, sugar, and protein, vitreous humor is viscous i.e., jelly-like.
Functions:
- Both aqueous and vitreous humor maintain intraocular pressure and inflate the eyeball. This is how they maintain the shape of the eyeball.
- They act as refractory media of the eyes.
- Aqueous humor provides nutrients to the lens, cornea, iris, etc.
Cornea: It is the convex, transparent part of the human eyeball which also acts as a refractory medium to some extent.
Accessory Protective Part Of Human Eye
The structure and functions of accessory protective parts of the eyes are described below.
Accessory Protective Part Of Human Eye Eye orbit: In the anterior part of the human cranium, beside the nose, within two hollow cavities the eyeballs are placed.
These two hollow cavities are known as eye orbits. Note that eye orbit has a thick layer of muscular tissue, on which eyeballs are placed. Eyeballs are bound to the eye orbit by six muscles. The optic nerve too, helps to bind the eyeball to eye orbit.
Accessory Protective Part Of Human Eye Functions: Due to the presence of muscular tissue from the interior and bony covering from the outside, the eye orbit protects the eyeball from mechanical injury.
Eye muscles: The six muscles by which eyeball remains bound to the eye orbit are known as eye muscles.
These are—
- Superior rectus muscle,
- Inferior rectus muscle,
- Medial rectus muscle,
- Lateral rectus muscle,
- Superior oblique muscle,
- Inferior oblique muscle.
Functions:
- With the help of these muscles, we can move the eyeballs down and sideways.
- Eyeballs can also be rotated by these muscles.
Eyelids: The human eye is covered by a thin, extended, skin layer on the upper part and lower part.
These are known as upper eyelids and lower eyelids respectively. At the corner of the human eye (near the nose), a small, red, muscular nictitating membrane is present in a vestigial condition.
Accessory Protective Part Of Human Eye Functions:
Eyelids protect the frontal part of the eyeball from dust.
Under bright light eyelids close, thus protecting the eye, rather than the lens, from bright light.
Eyebrow and eyelash: Each eye of humans has two special parts on upper region of the eyelids and the lower region of the forehead.
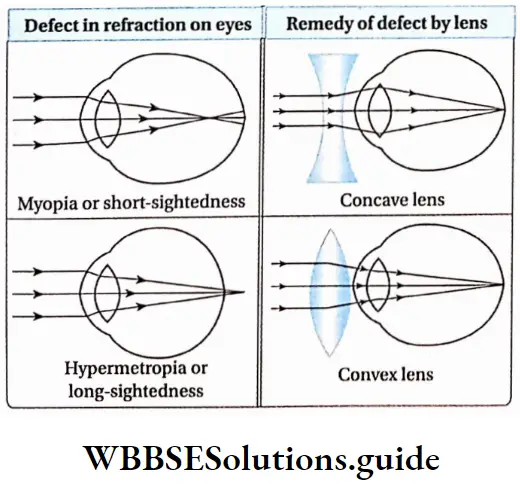
This part is curved like a bow and is known as an eyebrow. The eyelids are again lined by fine hairs which are known as eyelashes.
Accessory Protective Part Of Human Eye Function: Due to the presence of an eyebrow, rainwater, and sweat cannot enter the eyeball from the forehead.
Conjunctiva: The thin and transparent layer present beneath the upper eyelid and which extends upto the lower lid, covering the anterior part of each human eye is known as conjunctiva.
Conjunctiva is actually made up of squamous epithelium. Inflammation of the conjunctiva is known as conjunctivitis.
Accessory Protective Part Of Human Eye Functions:
It protects the eyeball from dust particles.
Being transparent, it allows light rays to pass through it easily into the eyeball to reach the lens.
Lacrimal gland: Lacrimal gland or tear gland is present in the upper lateral region of each orbit or beneath the upper and outer border of each eyelid. It opens into the upper eyelid by some tubules.
The tear produced in the tear gland is a fluid containing NaHC03, NaCI, etc. Tear also contains a bacteriolytic enzyme called lysozyme.
Accessory Protective Part Of Human Eye Functions:
Tears keep the upper surface of the eyeball moist. If the lacrimal gland gets damaged, secretion of tears is reduced, and conjunctiva contracts thereby causing dryness and burning sensation in the eye.
Tear wash out the dust particles present in the open the surface of the eyeball.
Phyllotaxy in plants – types and examples
Lysozyme, an antibacterial enzyme present in tears protects the eye from bacterial infection.
Physiological Function Of Eye
Vision is the main physiological function of the human eye. In case of the human eye helps us with two types of vision, such as—light vision and color vision.
Light vision: Eyes help us to see objects by providing a stereoscopic vision. The mechanism of vision by which eyes sense and visualize nearby and far away objects is given below.
Mechanism of vision:
- The human eye acts as a camera. Parallel or divergent light rays from objects pass through the conjunctiva, cornea, and aqueous humor and fall on the lens.
- After falling on the lens or incidence, light rays become convergent. These convergent rays pass through the vitreous humor, present behind the lens, and then fall on the yellow spot of the retina.
- Retina contains a photosynthetic pigment, called rhodopsin. Light splits rhodopsin and converts it into two chemical compound named retinene (retinal) and opsin.
- Light also brings changes in the structure of opsin which causes changes in membrane permeability.
- Changes in membrane permeability cause ion channels to open which results in potential difference and generation of action potential.
- This action potential i.e. impulse is carried by the optic nerve to the visual cortex of the cerebrum through the optic tract.
- Here the image is formed. Note, stimulus from the right eye goes to the visual cortex of the left cerebral hemisphere and stimulus from the left eye goes to the visual cortex of the right cerebral hemisphere. In the visual cortex, the stimulus is analyzed.
- By the special capability of the brain, the image becomes elongated. This results in the sensation of vision.
Color vision: Cone cells of the human eye help to determine the color of different objects.
Visual Accommodation
Human eyes cannot change the distance of the lens directly to observe objects nearer or farther. However, ciliary muscles and suspensory ligaments can adjust the curvature of the lens.
As a result, the focal length of the lens changes due to which the image of the object falls on the retina. This phenomenon is known as accommodation.
This is a type of reflex action. Human eyes have good visual accommodation. Light coming from any object located 25cm away can be easily sensitized by eyes.
This is known as the least distance of distinct vision. The ciliary bodies and suspensory ligaments of human eyes together are known as accommodation apparatus.
Some Important Eye Disorders
There are some important disorders related to the eyes which are as follows.
Myopia: It is the most common refractive error of the eye. Myopia is also referred to as short-sightedness as the person cannot see distant objects.
In this condition, parallel rays of light coming from distant objects, instead of focusing on the retina, focus in front of it.
As a result, objects located distantly cannot be seen clearly. It can be corrected by using glasses with a concave surface.
Hypermetropia or Hyperopia: It happens when the eyeball is shorter than normal and the parallel rays of light are brought to focus behind the retina.
It is also referred to as long-sightedness. In this case, nearby objects appear blurry while distant objects are seen clearly. It can be corrected by using glasses with convex lenses.
Astigmatism: Astigmatism is a common condition in which the curvature of the cornea or lens is not uniform.
This causes blurred vision of objects both near and far. This can be corrected by using glasses with cylindrical lenses.
Presbyopia: Presbyopia is an age-related eye condition that makes it more difficult to see near objects very clearly.
After the age of 40, the lens of the human eye becomes hard thereby losing the capacity of contraction-relaxation and thus people find difficult to see, particularly to read. It can be corrected by using glasses with bifocal or convex lenses.
Cataract: Due to aging, the lens becomes swollen, hard, and opaque. Vision becomes feeble and sometimes, is lost. This condition is known as cataract. It can be corrected by replacing the affected lens with an artificial one.
Glaucoma: The defects in the eyes that lead to damage of the optic nerve are known as glaucoma.
It happens due to an increase in intraocular pressure leading to the rupture of the optic nerve.
When blood flow is reduced in the optic nerve i.e., in the case of ischemia, the optic nerve is damaged.
Due to damaged optic nerve, vision is impaired and even blindness may occur.
Strabismus (squint): In this disorder, two eyes do not look exactly in the same direction at the same time.
It is caused due to dysfunction of the extraocular muscle. It is usually corrected by surgical procedures at an early stage.
Trachoma: It is a pathological condition caused by the bacterium Chlamydia trachomatis.
It is characterized by inflammation of the conjunctiva and cornea leading to pain and watering of the eyes.
In extreme cases, it may lead to complete blindness. Trachoma can be treated by antibiotics in the early stages and surgery in the late stages.
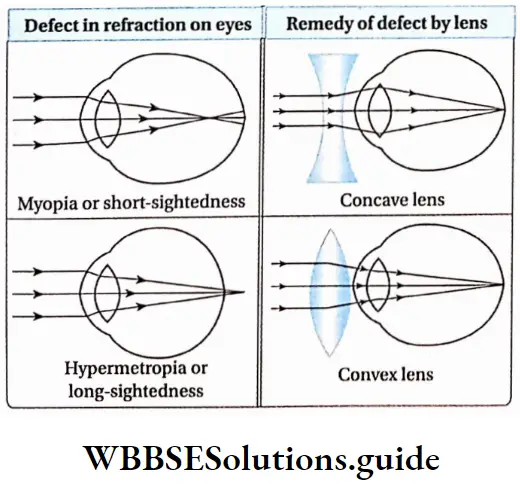
Human Ear
The human ear is the sense organ of hearing and equilibrium. It consists of three main parts—
- External ear,
- Middle ear and
- Inner ear. The ear receives the sound waves and helps in its interpretation.
Parts Of Ear
Different parts of the human ear are discussed under Separte Heads.
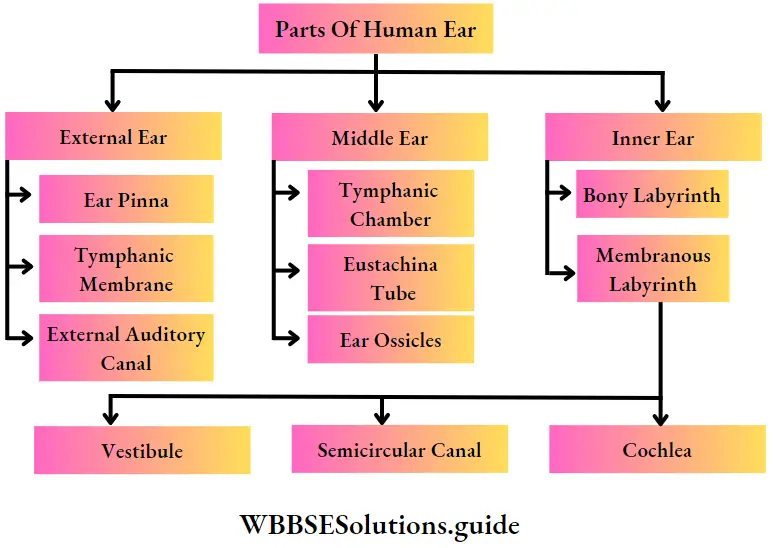
Sound waves can travel through solid, liquid, and gaseous medium. The human ear is the best example to Sound waves that can travel through solid, liquid and gaseous mediums. The human ear is the best example of solid bones in the middle ear and fluid medium in the inner ear.
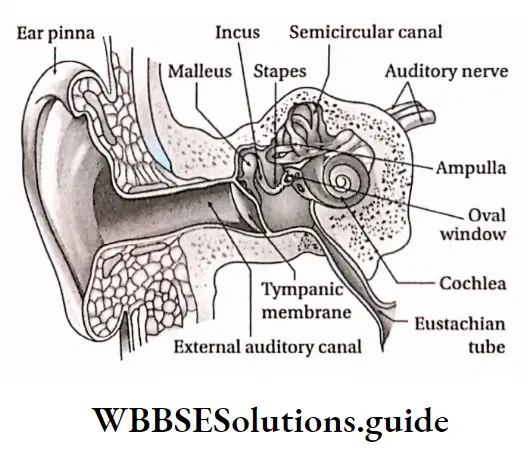
External Ear
The human external ear consists of three parts—pinna, external auditory canal, and tympanic membrane.
External Ear Pinna: The outer ridged cartilaginous part of the ear covered with skin, through which sound waves are received from the external environment is called the pinna.
External Ear Location: The pinna is an expanded cartilaginous portion, covered with skin that projects from both sides of the head.
External Ear Characteristics:
- Pinna is made of elastic cartilage. It has an expanded leaf-like structure, it has a skinny covering on cartilage.
- Along the upper periphery of the pinna, a fold is seen, known as a helix.
- The lower part of the pinna is muscular and so, it is calculated. This flexible lobe is known as the lobule.
- The muscles of the pinna are vestigial, hence, the human pinna cannot be moved.
Functions:
- Pinna collects sound waves from different sources and funnels them to the auditory canal.
- Therefore, pinna acts as the receiver of sound waves.
- Due to the presence of folds in pinna, it inhibits dust, insects, etc., from entering the auditory canal.
External auditory canal: This is the S-shaped passage through which sound waves travel from outside to the tympanum.
Location: External auditory canal or external auditory meatus, a part of the external ear, extends from an opening in the pinna to the tympanic membrane.
Characteristics:
- The external auditory canal is a slightly bent, tubular structure. It runs upward and then downward.
- It is supported by cartilage and temporal bone in the outer and inner portions respectively. The junction of the outer and inner portions is referred to as the osteocartilaginous junction.
- The inner wall of the auditory canal is covered by skin. The sweat gland of this layer has transformed into a ceruminous gland or wax gland which secrete cerumen or earwax.
Functions:
- It conducts the sound waves towards the tympanic membrane. 0 Since it is a bit bent, it protects the tympanic membrane from external mechanical injuries.
- The ceruminous gland in its wall secretes a waxy substance, cerumen that contains lysozyme and immunoglobulin. So, dust particles, insects, and germs cannot reach upto the tympanic membrane.
- Tympanic membrane or tympanum or ear drum: It is the membrane that acts as a partition between the external and middle ear and vibrates in response to sound waves.
Location: It is located in the inner region of the auditory canal i.e., as a separating membrane between the auditory canal and the middle ear.
Characteristics:
It is an elliptical, smooth, and translucent separating membrane. It separates the middle ear from the external ear.
It stretches from the frontal to the posterior end, across the end of the external auditory canal.
Its outer surface is concave and inner surface is
convex. It remains in stretched condition.
The tympanic membrane consists of three layers—the outer layer of stratified epithelium, a middle fibrous layer, and an inner layer of cuboidal epithelium.
Its inner layer is connected with the arm of the ear ossicle, the malleus.
Functions: The tympanic membrane is considered as the eardrum. Vibrating sound waves, transmitted by air strike the tympanic membrane.
This creates vibrations in the membrane. These vibrations are transmitted to the inner ear through ear ossicles in the form of waves.
Middle ear
Inner to the tympanic membrane, within the temporal bone of the human skull, the middle ear is located.
The three parts of the middle ear are—
- Tympanic cavity,
- Eustachian tube,
- Three ear ossicles.
Tympanic cavity: The small space in the middle ear surrounding the ear ossicles is called the tympanic cavity.
Location: It is an irregularly shaped, air-filled chamber, embedded in the inner portion of the temporal bone.
Characteristics:
- The tympanic cavity is an air-filled chamber.
- The inner wall of the chamber is lined by cuboidal epithelial tissue.
Functions:
- The lower part of the tympanic cavity is connected to the eustachian tube.
- It houses three little bones—malleus, incus, and stapes.
Eustachian tube: The tubular canal through which the tympanic cavity communicates with the nasopharynx is called the eustachian tube.
Location: It is located in the middle ear, from the lower portion of the tympanic membrane to the nasopharynx. It is also known as a pharyngotympanic tube or auditory tube.
Characteristics:
- The eustachian tube opens into the nasopharynx through an opening. So, the eustachian tube is also known as pharyngo-tympanic tube.
- Its inner wall is lined by ciliated epithelial tissue.
Functions:
Through this tube air from the mouth cavity and pharynx enters the tympanic cavity. As a result, air pressure on both sides of the tympanic membrane remains the same. So, the tympanic membrane does not burst even in loud sounds.
Due to the presence of ciliated epithelium in the inner wall, dust particles and mucous are present in the air. from the mouth cavity and pharynx, do not reach the tympanic cavity.
Auditory ossicles: These are the three bones in the middle ear, which are articulated from a chain for the transmission of sound from the external ear to the internal ear.
Location: The tympanic cavity of the middle ear contains three ear bones, connected with each other by bony joints. Ligaments bind the joints of these three bones.
Types: Three ear ossicles of the middle ear, from the end of the tympanic membrane, are—malleus, incus, and stapes.
Malleus: Malleus looks like a hammer. It bears a spherical head and an elongated arm. This arm is connected to the inner portion of the tympanic membrane and the spherical head joins with the next ossicle, incus.
Incus: Incus is the second ossicle. It appears like an anvil. Its frontal part has a concave cup-like ridge.
Within it, the head of a malleus is placed and it forms a joint. Its long appendage helps it to join with the third ossicle, stapes.
Stapes: It is the third and smallest ossicle of the human ear. It is also the smallest bone of the human body. It appears like a stirrup. It has a head, neck, two arms, and an oval base.
Its head remains bound to the appendage of the incus. On the inner surface of the tympanic cavity, an oval opening is seen, known as an oval window or fenestra ovalis. The base of the stapes is attached to this opening.
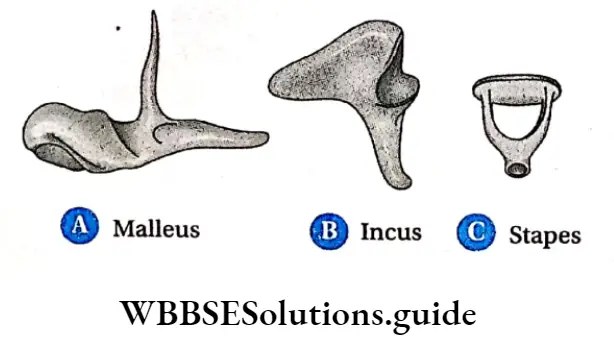
Functions: When sound waves strike the tympanic membrane, the vibrations are transmitted through the ossicles—malleus, incus, stapes, via the oval window to the inner ear.
Inner Ear
The inner ear is located next to the middle ear and is a double-walled structure. It has two main parts— a bony labyrinth and a membranous labyrinth.
Bony labyrinth: Bony labyrinth is located in a cavity, within the temporal bone. The space between the bony and membranous labyrinth is called perilymphatic space. This space is filled with perilymph.
Membranous labyrinth: It is a complex structure, containing canaliculi and membranous sacs.
The fluid present in it is known as endolymph. This part is connected to the auditory nerves.
It is composed of three parts—
- Vestibule,
- Three semicircular canals and
- Cochle
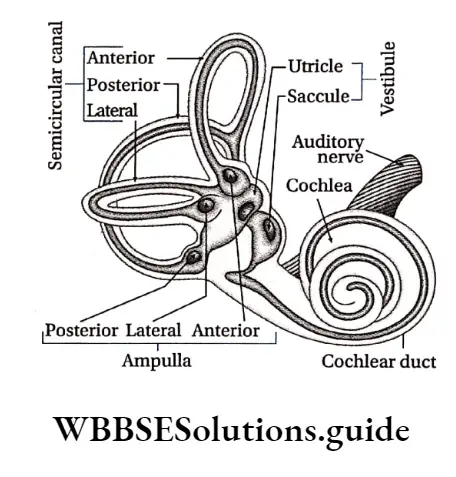
Vestibule: The extended portion of the membranous labyrinth of the inner ear, connected to the three semi-circular canals is known as the vestibule.
It is central sac-like part, which is again formed of two unequal parts— utricle and saccule and is known as the otolith organ.
Structural features:
The vestibule is an endolymph-filled, thin membrane-bound chamber,
This part contains two endolymph-filled sacs. The larger one is called utricle and the smaller one is called saccule.
The endolymph of vestibule contains granules of CaC03 and silica. These are known as otoliths,
Its inner wall is lined by ciliated epithelium and the base of the cells of this part are connected to nerve fibers of vestibular branches of the auditory nerve.
There are 2 sensory spots in the vestibule—the macula of the utricle and the macula of the saccule. The macula consists of sensory hair cells and supporting cells.
Functions: Movement of head causes displacement of the otolith. Thus, sensory cells of the utricle and saccule are stimulated.
This stimulation reaches the cerebellum through auditory nerves. In this way, vestibule of the inner ear maintains body balance with the help of the cerebellum.
Vestibular Apparatus
The three semicircular canals, endolymph containing sacs—utricle and saccule altogether are known as vestibular apparatus. It plays an important role in maintaining body balance.
Utricle And Saccule
Utricle: It is a large sac whose frontal part consists of three semicircular canals, containing ampullae. A duct opens at the dorsal part of the utricle which is known as utricosaccular duct.
Saccule: It is a comparatively smaller sac. The duct opening from the posterior end of the saccule is known as ductus endolymphaticus.
This duct joins with the utriculosaccular duct extends more at the dorsal surface and fuses into a closed sac called saccus endolymaphaticus. Another small duct from the saccule, known as ductus reuniens joins with the cochlear duct.
Three semicircular canals: The frontal part of the membraneous labyrinth contains three bow-like canals. These are known as semicircular canals.
Structural features:
- The three semicircular canals of the inner ear are located in three planes. These planes are located equilaterally.
- The base of each canal is swollen and is known as ampulla (plural: ampullae)
- Due to the presence of the common arm of two semicircular canals, each ear contains five ampullae. Each ampulla contains a sensory spot, called crista ampullaris. Each crista consists of longer hair cells and a gelatinous mass, called a cupula (lacks otolith)
- Endolymph is present between the semicircular canals, ampullae, and vestibule
- The inner wall of an ampulla contains sensory ciliated epithelial tissue.
Functions: The semicircular canal is under the control of the auditory nerve. Displacement of otolith maintains body balance.
Cochlea: The coiled part that appears like a snail and is located posterior to the membraneous labyrinth is known as the cochlea.
Structural features:
The cochlea’s interior is divided into three parallel, fluid-filled compartments by two membranes, the vestibular (Reissner’s) membrane and the basilar membrane,
Each compartment is referred to as a scala (staircase) since each one spiral about an axis or the central pillar of the cochlea like a winding staircase.
They are the (bony) scala vestibuli, the (membranous) scala media or cochlear duct, and the (bony) scala tympani.
The interiors of the scala vestibule and scala tympani are lined by a simple squamous epithelium. Inside scala vestibuli and scala tympani, perilymph is present,
The scala vestibule and scala tympani communicate with each other by a narrow passage, helicotrema. This structure permits perilymph to flow from the scala vestibule into the scala tympani.
At the proximal end of the cochlea, the scala vestibule, and scala tympani communicate with the oval and round window respectively,
The cochlear duct also referred to as the scala media, contains endolymph. In the cross-section of the cochlea, the triangular-shaped cochlear duct appears to be wedged between the scala vestibule and the scala tympani.
The Reissner’s membrane, the roof of the cochlear duct, serves as a division between the cochlear duct and the scala vestibuli. This membrane is composed of squamous epithelium.
Its function is unclear; however it is believed to play a role in the transmission of vibrations from the perilymph of the scala vestibule to the endolymph of the cochlear duct,
The floor of the cochlear duct, which separates it from the scala tympani, is the basilar membrane. The basilar membrane is an elastic structure.
It shows a gradual decrease in stiffness from the oval window (at the cochlear base) to the helicotrema (at the cochlear apex),
The gradual decrease in stiffness permits this membrane to be sensitive to high-frequency vibrations near the cochlear base, and low-frequency vibrations near its apex,
Thus, the Reissner’s membrane is interposed between the scala vestibule and the cochlear duct, and the basilar membrane is interposed between the cochlear duct and the scala tympani.
The receptors associated with the sense of hearing form a structure, the organ of Corti, which rests along the floor of the cochlear duct upon the basilar membrane,
The organ of Corti consists of supporting epithelial cells (pillar cells, cells of Hensen, cells of Claudius, etc.) and neurosensory receptor cells, called ‘hair cells’.
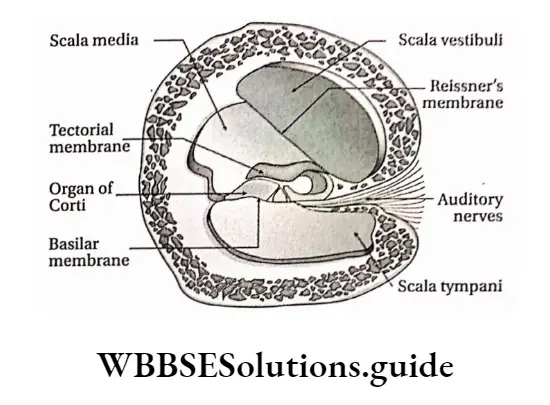
Each hair cell displays numerous stereocilia and a single kinocilium projecting from its apical cell surface,
The free ends of the stereocilia project into the tectorial membrane, an acellular, gelatinous sheet,
The hair cells are the receptors of the auditory system that act as transducers. They serve to convert mechanical energy into electrical energy that can be relayed to the brain-stem,
Hair cells synapse with the peripheral ends (dendritic processes) of the bipolar neurons whose cell bodies are housed in the spiral ganglion.
Leaf morphology important questions for NEET and exams
The central processes of these bipolar neurons form the cochlear nerve, which joins the vestibular nerve to form the vestibulocochlear nerve (VIII cranial nerve).
This nerve courses through the internal acoustic meatus to enter the cranial vault, and then enters the brainstem
Functions: Cochlea is stimulated by sound vibrations produced in the organ of the Corti. This sensation is transmitted to the cerebrum by auditory nerves. In this way, the cochlea helps in hearing.
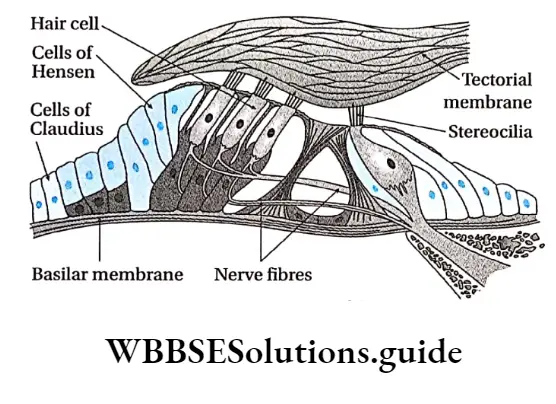
The Physiological Function Of The Ear
Physiological functions of the human ear are as follows— Hearing: The ear enables us to hear external sound.
Mechanism of hearing:
Sound waves from vibrating bodies are transmitted through air to the pinna.
From there, sound waves, through the auditory canal, reach the tympanic membrane. This vibration is transmitted through the ear ossicles of the tympanic cavity to the inner ear via an oval window.
Vibrations are transmitted in the form of waves to the perilymph of scala vestibuli through the fenestra ovalis and then transferred to the scala media through Reissner’s membrane.
The waves in the endolymph cause the basilar membrane to vibrate. This causes the hair cells to bend, pressing them against the tectorial membrane.
As a result of stimulation of the receptor cells, nerve impulses are generated in the associated afferent neurons.
These are conducted by auditory nerves to the auditory cortex of the brain. There it is analysed and we are able to hear.
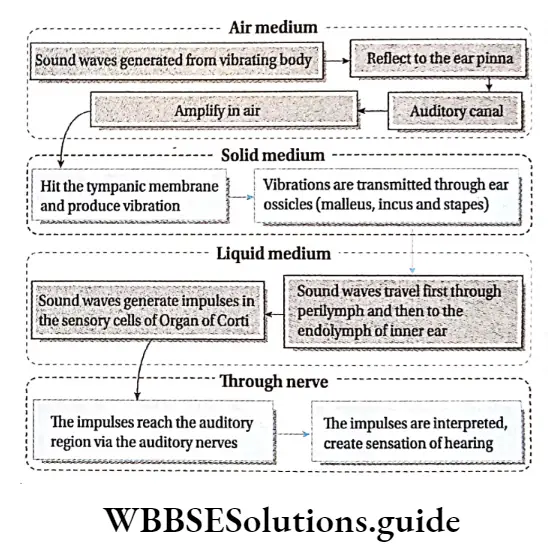
Understanding pitch of sound: The pitch of sound depends on the vibrations of sound waves.
Sounds of different vibrations cause stimulation along different regions of the basilar membrane depending on the pitch of the sound.
So, we can understand sounds of varied pitch. In the case of high-pitched sounds or sounds of high frequency, the receptor cells at the base of the cochlear duct are stimulated.
In the case of low-pitched sound, the receptor cells towards the tip are stimulated.
Understanding loudness of sound: Loudness of sound depends on the distribution of sound. Loudness is expressed by decibels (dB).
The greater the amplitude of sound, the more receptor cells of the organ of Corti in the basilar membrane are stimulated.
Hence, sound can be heard louder. Too loud sound damages the cells of the basilar membrane, causing deafness.
Maintenance of body balance:
- The vestibule and three semicircular canals of the human inner ear maintain the body balance.
- The vestibule and semicircular canals have sensory epithelial tissue. This part contains CaC03 and silica suspended in endolymph.
- These substances are displaced upon a change in body posture, This causes stimulation of cristae and maculae present in the ampulla and vestibule respectively.
- This stimulation is transmitted through auditory nerves of the vestibular branch that join with a cochlear branch to form the vestibulocochlear nerve or auditory nerve.
- The vestibular branch transmits the stimulus first to the vestibular nucleus and next to the cerebellum.
- The cerebellum receives stimuli from proprioceptors of the eyes, skeletal muscles, and joints. These stimuli are then transferred finally to the cerebrum and thus body balance is maintained.
Leaf modifications for storage, support, and reproduction
Notes
- Ampulla: Swollen part of semicircular canal.
- Ganglion: A structure containing a number of nerve cell bodies, linked by synapses and often forming a swelling on a nerve fiber.
- Kinocilium: A special type of cilium on the apex of hair cells located in the inner ear of the vertebrates.
- Motor end plate: The plate-like formation at the nerve terminal where an axon of a motor neuron establishes synaptic contact with the sarcolemma of the striated muscle fiber.
- Neurilemma: The plasma membrane of a neuronal cell body.
- Neurotransmitter: Chemicals that help in the transmission of nerve impulses throughout the nervous system.
- Nuclei: Aggregation of nerve cell bodies within the CNS (not to be confused with the nucleus of a cell).
- Ossicles: A very small bone usually occurring in the middle ear.
- Photoreceptor discs: The outer segment of rods and cone cells lack, ER, Golgi, and mitochondria and are filled with a hundred to a few thousand flattened membrane organelles, called photoreceptor discs.
- Plexus: A structure in the form of a network of nerves.
- Stereocilia: Mechanosensing organelles of hair cells, having a similar structure to microvilli.
- Threshold stimulus: The minimum stimulus required for a reflex action to occur.
Points To Remember
- Neurons are the basic structural and functional units of the nervous system.
- Each nerve cell (neuron) consists of a cell body or soma from which numerous processes arise.
- The human nervous system is divided into two types—central nervous system (CNS) and peripheral nervous system (PNS).
- The cell bodies within the central nervous system (CNS) are frequently clustered into groups called nuclei (not to be confused with the nucleus of a cell).
- The plasma membrane of the axon is called the axolemma, and the cytoplasm contained in it is called the axoplasm.
- Association neurons or interneurons are located entirely within the CNS and serve the associative, or integrative functions of the nervous system.
- The glial cells support neurons structurally and maintain their long-term neuronal integrity.
- The junction between two neurons is called a synapse. It is also called physiological value.
- A nerve is a cord-like structure composed of nerve fibers (axons) and connective tissue.
- A sensory nerve is composed of afferent fibers only a motor nerve of efferent fibers only, and a mixed nerve is composed of both. Most nerves are mixed.
- There are 12 pairs of cranial nerves and 31 pairs of spinal nerves.
- Meninges surround the brain and spinal cord and act as a try layered protective sheath or covering.
- The spinal cord is divided into cervical, thoracic, lumbar, and sacral regions, each served by spinal nerves.
- The autonomic nervous system deals with the visceral organs, like the heart, stomach, glands, and intestines.
- Any changes in the resting membrane potential (which is -70 mV), due to a stimulus of sufficient magnitude, that cause the membrane potential to move towards zero potential (less negative) mean depolarisation.
- A reflex is a quick, involuntary, stereotyped reaction of a gland or a muscle to a stimulus.
- Somatic (spinal) reflexes are responses of skeletal muscles.
- The retina contains the receptors for sight—rod and cone cells.
- The center of the retina contains a special region called the fovea centralis. It is an oval, yellowish area with a depression containing only cone cells.
- The ear is divisible into three parts—the external ear, the middle ear, and the inner ear, each performing a necessary function for the perception of sound.
- The external ear is comprised of the cartilaginous structure—pinna, external auditory canal, and the tympanic membrane.
- The middle ear is embedded in the temporal bone of the skull.